Published online Apr 14, 2012. doi: 10.3748/wjg.v18.i14.1689
Revised: October 16, 2011
Accepted: January 18, 2012
Published online: April 14, 2012
AIM: To analyze the literature on the use of Chinese herbal medicines for the treatment of cholecystitis.
METHODS: The literature on treatment of cholecystitis with traditional Chinese medicines (TCM) was analyzed based on the principles and methods described by evidence-based medicine (EBM). Eight databases including MEDLINE, EMbase, Cochrane Central (CCTR), four Chinese databases (China Biological Medicine Database, Chinese National Knowledge Infrastructure Database, Database of Chinese Science and Technology Periodicals, Database of Chinese Ministry of Science and Technology) and Chinese Clinical Registry Center, were searched. Full text articles or abstracts concerning TCM treatment of cholecystitis were selected, categorized according to study design, the strength of evidence, the first author’s hospital type, and analyzed statistically.
RESULTS: A search of the literature published from 1977 through 2009 yielded 1468 articles in Chinese and 9 in other languages; and 93.92% of the articles focused on clinical studies. No article was of level I evidence, and 9.26% were of level II evidence. The literature cited by Science Citation Index (SCI), MEDLINE and core Chinese medical journals accounted for 0.41%, 0.68% and 7.29%, respectively. Typically, the articles featured in case reports of illness, examined from the perspective of EBM, were weak in both quality and evidence level, which inconsistently conflicted with the fact that most of the papers were by authors from Level-3 hospitals, the highest possible level evaluated based on their comprehensive quality and academic authenticity in China.
CONCLUSION: The published literature on TCM treatment of cholecystitis is of low quality and based on low evidence, and cognitive medicine may functions as a useful supplementary framework for the evaluation.
- Citation: Dong ZY, Wang GL, Liu X, Liu J, Zhu DZ, Ling CQ. Treatment of cholecystitis with Chinese herbal medicines: A systematic review of the literature. World J Gastroenterol 2012; 18(14): 1689-1694
- URL: https://www.wjgnet.com/1007-9327/full/v18/i14/1689.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i14.1689
Cholecystitis, defined as a type of acute or chronic inflammation occurring in the gallbladder caused by infection, bile stimulus, reflux of pancreatic juice to the biliary passage, as well as bilirubin and lipoid metabolic disorders etc. Cholecystitis is often secondary to previously asymptomatic gallstone disease[1]. Around 90%-95% of cholecystitis cases are claimed to be caused by gallstone disease, the incidence of which is 8%-10% in America and 3%-11% in China[2,3]. Recent epidemiological studies have shown that the incidence of cholelithiasis has been continuously rising, and the rate is doubling every 10 years[4]. The incidence rate of cholelithiasis grows steadily with age, varies by race, and occurs more frequently in female patients than in male patients[2].
For symptomatic cholecystitis, antibiotics and antispasmodic treatment are conventional therapy while cholecystectomy or laparoscopic cholecystectomy are also appropriate modalities of treatment[5]. However gallstone disease of this type may recur within several months. Gallstones may also recur in the biliary tract after cholecystectomy[2]. Therefore, it is important to identify effective treatment options and adjuvant therapeutic methods for cholecystitis. Traditional Chinese medicines (TCM) has a long history of use for treating cholecystitis and has developed an intecrate system of medical examination and treatment. Classic TCM works such as Huang Di Nei Jing and Shang Han Za Bing Lun have both expounded on this disease in depth. In TCM, cholecystitis is categorized as a type of illness with symptoms such as aching over the lateral torso, jaundice, hepatic distention, gallbladder distention and abdominal pain, etc[6,7]. Cholecystitis is considered by TCM to be caused mainly by unrestrained food and drink, exogenous heat and moisture, chronic illness and/or injury[8].
The large quantity of research literature on the TCM treatment of cholecystitis in China stimulates the development of innovative and improved therapeutic methods for the treatment of the disease. However, even basic information about the literature such as the level of evidence, quantity, trends in publication, and existence of research institutes remains unclear since they have not been sufficiently studied or evaluated outside of China due to barriers by language and access. Thus, a comprehensive analysis of this large quantity of literature is urgently required.
Based on the principles and methods described by evidence-based medicine (EBM), this study conducted an examination and statistical analysis of current literature on the treatment of cholecystitis with TCM, aiming to discuss the necessity for a systematic review as well as producing a reference to enable better research of TCM.
Electronic literature searches were conducted on the following databases: China Biological Medicine Database (CBM), Chinese National Knowledge Infrastructure Database (CNKI), Database of Chinese Science and Technology Periodicals (VIP), Database of Chinese Ministry of Science and Technology (Wanfang), The Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (via PubMed) and EMbase. The databases were searched from the earliest possible date until June 1, 2009. The search terms included (“Cholecystitis” or “Acalculous Cholecystitis” or “ Emphysematous Cholecystitis” or “Cholecystitis, Acute” or “Cholecystitis, Chronic”) and (“Chinese herbs” or “TCM” or “Chinese medicine” or “Integrated TCM WM” or “herb” or “herbs” or “traditional Chinese medicine” or” Drugs, Chinese Herbal”). The search terms were adjusted depending on the database being searched. Titles and abstracts of all citations were screened independently by two reviewers (Dong ZY and Wang GL).
Articles on TCM treatment of cholecystitis were included; and articles on cholecystitis treated by integrated traditional Chinese and modern medicine were included.
The full-text of articles that met all the selection criteria was retrieved. The data were screened independently by two reviewers (Dong ZY and Wang GL) using a self-made data extraction form which collected the following information: year of publication, first author, the organization of the first author, the hospital level of the first author, titles of authors, study design, type of article, journal name, and indexed/citation situation by medical indexing databases. The first author of each article was contacted if there were any missing data. Articles that did not meet the inclusion criteria were excluded by reading the titles and summaries. Disagreements whether a paper was to be included were resolved by discussion.
Methodology of data classification were listed below. (1) Classified by types of study[9]; (2) Classified according to indexed/citation situation (evaluated according to 2008 edition of “Guide to the Core Journals”, and the list of MEDLINE contains Chinese journals 2008)[10,11]; (3) Classified according to the first authors’ hospital-level[12]: Level-3 hospital - The national, provincial, municipal large hospitals and affiliated hospitals of medical colleges; Level-2 hospital - General hospitals of cities, counties, districts, hospitals affiliated to factories, mining enterprises and institutions; Level-1 hospital - Countryside primary hospitals, townships or neighborhood community and private clinics and hospitals; and (4) Classified according to the strength of evidence (Grading quality of evidence and strength of recommendations, strength grading standards by Cochrane Collaboration)[13].
Statistical data were collected and recorded in Excel and SPSS 17.0. Percentages, percentage bar charts and trends lines were produced to analyze the situation and trends, while the constituent ratios were expressed in terms of percentages in order to perform a descriptive analysis.
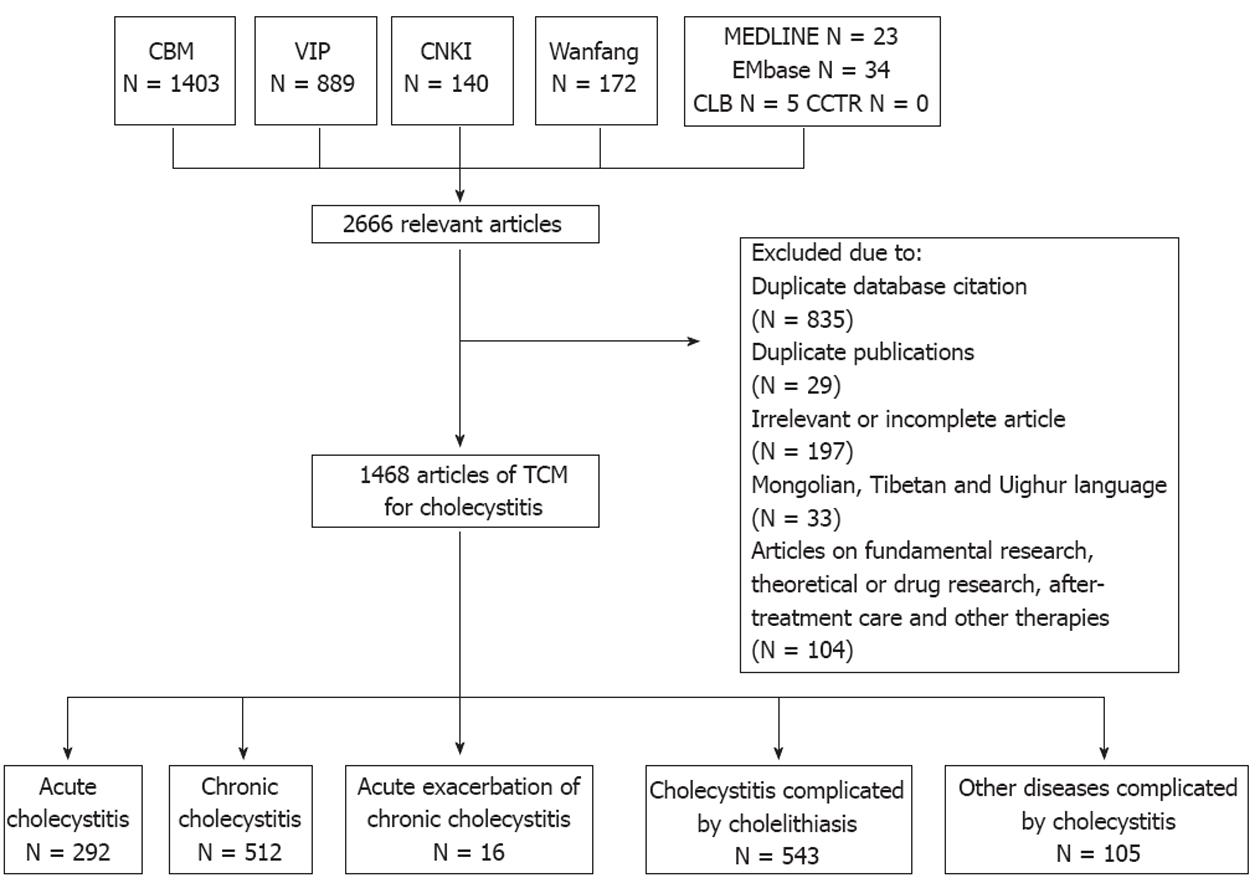
Altogether 2666 potentially relevant articles were retrieved from eight databases, among which 1822 were written in Chinese and 835 were duplicate citations between databases. Twenty-nine duplicate articles were excluded; there were 197 irrelevant or incomplete articles; 33 articles were written in Mongolian, Tibetan and Uighur; and 104 articles were on fundamental research, theoretical or drug research, after-treatment care and other therapies. Thus, there were 1468 articles on the TCM treatment of cholecystitis in total. Among these articles, there were 292 concerning cholecystitis, 512 regarding chronic cholecystitis, 16 regarding acute exacerbation of chronic cholecystitis, 543 regarding cholecystitis complicated by cholelithiasis, and 105 on other diseases complicated by cholecystitis. Among the retrieved articles, 9 were foreign articles, including 2 in Bulgarian, 1 in Russian and 6 in English (Figure 1).
We also searched Evidence Based Complementary and Alternative Medicine (eCAM), The American Journal of Chinese Medicine (AJCM), Journal of Chinese Integrative Medicine (J Chin Integr Med), Chinese Journal of Integrated Traditional and Western Medicine and Alternative Medicine Review (Altern Med Rev). No relevant articles were found in any of these sources.
In total, 1468 articles on TCM treatment of cholecystitis were retrieved: 15 articles on treatment and care, 24 on animal and fundamental experimental research, 25 on theoretical research, 9 on relevant drug research and 22 on other therapies including massage, ear points, diet, infrared ray, acupuncture and ultrasonic therapy, etc. The data revealed that researches on clinical treatment covered the majority of the relevant literature, with the percentage as high as 93.92%, and that TCM was applied to treat almost all types of cholecystitis (Table 1).
| Acute cholecystitis | Chronic cholecystitis | Acute exacerbation of chronic cholecystitis | Cholecystitis complicated by cholelithiasis | Other diseases complicated by cholecystitis | Total | |
| Clinical trial study | 292 | 512 | 16 | 543 | 105 | 1468 |
| Treatment and care | 3 | 0 | 0 | 12 | 0 | 15 |
| Animal and fundamental experimental research | 3 | 3 | 0 | 17 | 1 | 24 |
| Theoretical research | 3 | 10 | 0 | 10 | 2 | 25 |
| Other therapies | 3 | 12 | 0 | 7 | 0 | 22 |
| Relevant drug research | 2 | 4 | 1 | 2 | 0 | 9 |
| Total | 306 | 541 | 17 | 591 | 108 | 1563 |
The 1468 articles were categorized according to the Cochrane collaboration criteria as shown in Table 2. No article was included into the category of the highest evidence strength, namely level I, while 136 (9.26%) articles were categorized into level II, 101 articles (6.88%) into level III, 961 articles (65.46%) into level IV; and 270 articles (18.39%) into level V. This revealed that, with randomized controlled trial (RCT) forming a low percentage, the evidence level of the research literature on TCM treatment of cholecystitis appears to be relatively low, requiring a further systematic evaluation of RCT in order to determine the efficacy and safety of the TCM treatment of cholecystitis.
| Acute cholecystitis (H/M) | Chronic cholecystitis (H/M) | Acute exacerbation of chronic cholecystitis | Cholecystitis complicated by cholelithiasis (H/M) | Other diseases complicated by cholecystitis (H/M) | Total | Evidence level | |
| Systemic review | 0 | 0 | 0 | 0 | 0 | 0 | I |
| RCT | 35 (2/2) | 62 (6/0) | 6 (1/0) | 28 (1/1) | 5 (1/0) | 136 | II |
| Case-control | 19 (1/0) | 40 (2/1) | 1 | 37 (4/1) | 4 (1/0) | 101 | III |
| Case report | 203 (9/3) | 336 (26/0) | 7 (1/0) | 344 (27/1) | 71 (7/0) | 961 | IV |
| Experience reports/Masters experience | 31 (2/0) | 54 (4/0) | 2 | 109 (7/2) | 20 (1/0) | 216 | V |
| Review | 5 (1/0) | 19 | 0 | 25 (2/0) | 5 (1/0) | 54 | V |
| Total | 293 | 511 | 16 | 543 | 105 | 1468 |
Among the 1477 articles on TCM treatment of cholecystitis both in Chinese and English, 107 (7.24%) were included by core Chinese journals. The 10 articles included in MEDLINE and the 6 in SCI represented 0.68% and 0.41% of the articles, respectively. This reflects a seemingly inadequate writing quality, low research level of the literature, and a generally low international recognition.
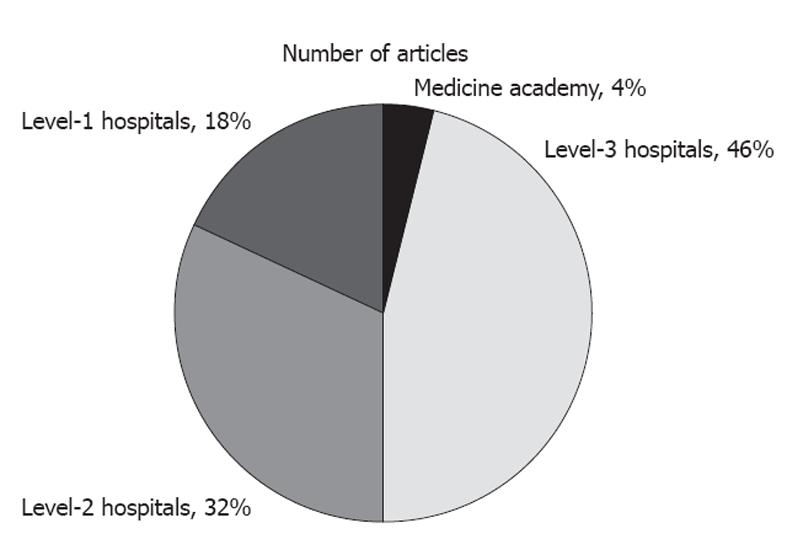
The 1468 Chinese articles on TCM treatment of cholecystitis were categorized according to the first authors’ hospital levels as shown in Table 3. Among the literature, authors from level-3 hospitals contributed 464 articles (31.61%); level-2 hospitals 538 (36.65%); medical schools and universities 51 (3.47%); research institutes 15 (1.02%); and level-1 hospitals, township hospitals and private clinic/hospitals contributed 400 (27.25%). This shows that the authors of the research literature in this study mainly came from level-3 and level-2 hospitals, which accounted for 68.26% of the total. The RCT distributed as such: level-3 hospitals contributed 62 articles (45.59%); level-2 hospitals 43 (31.62%), level-1 hospitals and others 25 (18.38%); medical schools and universities 6 (4.41%) (Figure 2). Literature with a higher evidence level was also mainly contributed by authors from level-3 hospitals and medical schools/universities.
| Acute cholecystitis | Chronic cholecystitis | Acute exacerbation of chronic cholecystitis | Cholecystitis complicated by cholelithiasis | Other diseases complicated by cholecystitis | Total | |
| Level-3 hospitals | 107 | 149 | 10 | 163 | 35 | 464 |
| Level-2 hospitals | 106 | 197 | 5 | 193 | 37 | 538 |
| Level-1 hospitals and others | 76 | 132 | 1 | 163 | 28 | 400 |
| Medical schools and universities | 4 | 26 | 0 | 16 | 5 | 51 |
| Research institutes | 0 | 7 | 0 | 6 | 2 | 15 |
From the above analysis, two major weaknesses were revealed by the selected literature on TCM treatment of cholecystitis. The first one is that only few papers were included by SCI and MEDLINE. Although it is not appropriate to evaluate the quality of papers merely according to whether they are included by SCI, MEDLINE and other core medical databases, it is an objective index to certain degrees, based on the strict selection rules and expert evaluation system of SCI and MEDLINE[14].
The second weakness of the literature in general lies in its low evidence level. The concept of evidence levels originated from the emergence and development of EBM, and was first proposed by the clinical epidemiologist Dave Sackett from McMaster University of Canada in 1990[15-17]. High-quality papers and RCTs require an adequate high-quality research platform. Is the large quantity of papers with low evidence level given rise to by an inadequate platform for the research of TCM? To answer this question, after analyzing the distribution of the hospitals, institutions or universities of the first authors, we discovered that 35.08% of the papers were contributed by authors from level-3 hospitals and universities. This accounts for all the articles included by SCI or published in core journals not included in SCI, while 64.92% of the articles were from level-1 and level-2 hospitals with a relatively low research capacity, which indicates a close correlation between the quality of published papers and the research platform. We also found from the data that RCTs hold only less than 10% of all TCM clinical studies, which is an outstanding difference compared to the 70% share of RCTs in the clinical study of modern medicine. Why such a low percentage TCM clinical study is from RCTs is a significant question that deserves further consideration[18].
EBM is a young discipline; the first International EBM Research Center was established in the United Kingdom in 1993, and the first EBM Research Center in China was set up three years later and quickly motivated the spread of EBM theory within China. Although the preference of Chinese TCM researchers for clinical study models somewhat limits the strict RCT research to a certain degree, TCM has its own unique treatment models and standards which deserves proper recognition. For example, it advocates individualized treatment and medication. Namely, different treatment methods and medication might be applied to the same disease and even the same syndrome according to different physical conditions of the individual patient or even according to the different time and place that the illness occurs. This makes it hard for TCM to conduct a high-quality RCT which might be the major cause resulting in the low evidence level of these Chinese papers.
By examining the literature on the treatment of cholecystitis with TCM according to the principles of EBM, we hope to expose the problems and weakness in current TCM clinical studies so as to raise the quality of TCM research.
Here arises the question, how to evaluate the therapeutic effectiveness of TCM more scientifically? This is the right and urgent question that not only TCM but also the entire alternative and complementary medicine should address. EBM experts are trying to further perfect the research standard of RCTs and drafting research guidelines that can better meet the characteristics of TCM. Besides, more scholars are trying to improve the present frame of EBM. Professor Keine[18] from the Institute for Applied Epistemology and Medical Methodology in Germany has conducted a study of cognition-based medicine. Cognition-based medicine is a newly-developed methodological system of scientific medicine. Its primary element is the criteria-based assessment of therapeutic causality at the level of the individual patient[19]. Principles and criteria of single-case causality assessment have been analyzed and explained. Cognition-based medicine enables a methodological professionalization of clinical judgment as well as the explication of physician experience and expertise. Cognition-based medicine study design expands the current range of clinical research, extending from criteria-based causality assessment in single cases to new forms of cohort evaluations. Though cognition-based medicine studies only started recently, this trend is inspiring and promising. It will not only facilitate the evaluation of TCM, which greatly emphasize individualized medical treatment solution, but also accord with the trend of medical development which stresses the significance of individualized treatment, and cognition-based medicine, a beneficial complement to EBM, may play a significant role in clinical research[20,21].
The authors are thankful to Maxim S Petrov (The University of Auckland, Auckland, New Zealand); Professor You-Ping Li (Chinese Cochrane Centre/Chinese Evidence-Based Medicine Centre/West China Hospital, Sichuan University, China); Dr. Li-Ting Xiao, Dr. Yi-Cai Xiao and Dr. Liang Peng (The First Affiliated Hospital of Guangxi Medical University, Nanning, China); Dr. Qian-Wei Shi (Changhai Hospital Affiliated Second Military Medical University, Shanghai, China); and Karin Dearness (McMaster University, Canada) for their help in this study.
Epidemiological studies have shown that the incidence of cholelithiasis in recent years has been continuously rising and doubling every 10 years. For symptomatic cholecystitis, antibiotics and antispasmodic treatment are adopted clinically as conventional therapy while cholecystectomy or laparoscopic cholecystectomy are also considered as surgical modalities. However, gallstone disease of this type may recur within several months. Gallstones may also recur in the biliary tract after cholecystectomy. Therefore, it is important to identify effective treatment options and adjuvant therapeutic methods for cholecystitis.
By analyzing, from the perspective of evidence-based medicine, the substantial amount of Chinese literature over the past 10 years concerning the use of traditional Chinese medicine in the treatment of cholecystitis, the authors discovered the problems existing in these relevant studies, and proposed that cognitive medicine could provide supplementary methodology for future research.
When reviewing the large amount of relevant Chinese literature according to the evaluation standards provided by evidence-based medicine, most of the articles appear to be of poor design, quality and evidence level. However, many of these studies showed that traditional Chinese medicine functions effectively in treating cholecystitis. Cognition-based medicine, a beneficial complement to evidence-based medicine, may play a significant role in clinical research.
More appropriate randomized controlled trials with large samples should be designed and conducted in order to reasonably evaluate the efficacy of traditional Chinese medicine in the treatment of cholecystitis, and cognitive medicine also functions as a useful supplementary framework for the evaluation.
Evidence-based Medicine (EBM) aims to apply the best available evidence gained from the scientific method to clinical decision making. It seeks to assess the strength of evidence of the risks and benefits of treatments and diagnostic tests. Cognition-based medicine is a newly-developed methodological system of scientific medicine. Its primary element is the criteria-based assessment of therapeutic causality at the level of the individual patient. Principles and criteria of single-case causality assessment have been analyzed and explicated. Cognition-based medicine enables a methodological professionalization of clinical judgment as well as the explication of physician experience and expertise. Cognition-based medicine study designs expand the current range of clinical research, extending from criteria-based causality assessment in single cases to new forms of cohort evaluations. Though cognition-based medicine study only started in recent years, this trend is inspiring and promising.
The main stay of cholecystitis treatment is either laparoscopic cholecystectomy while it is a “hot” or conservative management with antibiotics and analgesia followed by laparoscopic cholecystectomy approximately 8 wk later. However, alternative medical therapies are used when the patient is unfit for surgical intervention. The article is suitable for publication in WJG.
Peer reviewer: Dr. Abdul-Wahed Meshikhes, MD, FRCS, Chairman and Consultant Surgeon, Department of Surgery, King Fahad Specialist Hospital, Amir Bin Thabit St, Dammam, 31444 Eastern Province, Saudi Arabia
S- Editor Shi ZF L- Editor Ma JY E- Editor Zhang DN
| 1. | Sleisenger MH, Fordtran JS, editors . Gastrointestinal Disease: pathophysiology, diagnosis, management. 5th Ed. Philadelphia: WB Saunders Co 1994; 798-799. |
| 2. | Domino FJ, Editor . The 5-Minute Clinical Consult, 2008. 16th Ed. Philadelphia, PA: Lippincott williams and wilkins 2007; . |
| 3. | Zhuang X, Li LM. An epidemiological study of risk factors for cholelithiasis. Zhonghua Liuxingbing Xue Zazhi. 1999;20:181-183. |
| 4. | Biliary Surgery Unit of Surgical Society of China. 10 years of change about cholelithiasis in China. Zhongguo Shiyong Waike Zazhi. 1995;33:652-658. |
| 5. | Gurusamy KS, Samraj K. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev. 2006;CD005440. [PubMed] |
| 6. | Yellow Emperor Qibo. wangbin (Tang), note. Huang Di Nei Jing. 1st ed. Beijing: Chinese Classical Works Publishing House 2003; 16-18. |
| 7. | Zhang ZJ. Yang JP, Luo L, He Y, editor. Shang Han Lun. 1st ed. Beijing: China Press of Traditional Chinese Medicine 2006; 96-98. |
| 8. | Traditional Chinese Internal Medicine. 1st ed. Zhou ZY, editor. Beijing: China Press of Traditional Chinese Medicine 2003; 270-302. |
| 9. | Clinical Epidemiology. 3th ed. Wang JL, editor. Beijing: People’s Medical Publishing House 2008; 49-50. |
| 10. | Peking University Library Editor: A Guide to the Core Journal (2008 Edition). Beijing: Peking University Press 2009; . |
| 11. | The list of MEDLINE contains about Chinese journals. Available from: http: //www.omschina.org.cn/news/ gonggao/2008/ 1221/3668.html. |
| 12. | Ministry of health of the people¡¯s republic of China. Available from: http: //www.moh.gov.cn/publicfiles/ business/ htmlfiles/ mohylfwjgs/s7655/200911/44379.htm. |
| 13. | Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, Bowman M. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556. [PubMed] |
| 14. | SCI (Science Citation Index) and MEDLINE. Available from: http: //thomsonreuters.com/. |
| 15. | Oxman AD, Sackett DL, Guyatt GH. Users’ guides to the medical literature. I. How to get started. The Evidence-Based Medicine Working Group. JAMA. 1993;270:2093-2095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 86] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Guyatt GH, Sackett DL, Cook DJ. Users’ guides to the medical literature. II. How to use an article about therapy or prevention. B. What were the results and will they help me in caring for my patients? Evidence-Based Medicine Working Group. JAMA. 1994;271:59-63. [PubMed] |
| 17. | Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268:2420-2425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2300] [Cited by in RCA: 1976] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 18. | Wu T, Li Y, Bian Z, Liu G, Moher D. Randomized trials published in some Chinese journals: how many are randomized? Trials. 2009;10:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 192] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 19. | Kiene H. [What is cognition-based medicine?]. Z Arztl Fortbild Qualitatssich. 2005;99:301-306. [PubMed] |
| 20. | Raspe H. [Cognition-based medicine from the viewpoint of evidence-based medicine]. Z Arztl Fortbild Qualitatssich. 2005;99:295-300. [PubMed] |
| 21. | Teut M, Warning A. [Leeches, phytotherapy and physiotherapy in osteo-arthrosis of the knee--a geriatric case study]. Forsch Komplementmed. 2008;15:269-272. [PubMed] |