Published online Apr 7, 2012. doi: 10.3748/wjg.v18.i13.1470
Revised: February 3, 2012
Accepted: February 16, 2012
Published online: April 7, 2012
AIM: To investigate the immunological repertoire in the peritoneal cavity of gastric cancer patients.
METHODS: The peritoneal cavity is a compartment in which immunological host-tumor interactions can occur. However, the role of lymphocytes in the peritoneal cavity of gastric cancer patients is unclear. We observed 64 patients who underwent gastrectomy for gastric cancer and 11 patients who underwent laparoscopic cholecystectomy for gallstones and acted as controls. Lymphocytes isolated from both peripheral blood and peritoneal lavage were analyzed for surface markers of lymphocytes and their cytokine production by flow cytometry. CD4+CD25high T cells isolated from the patient’s peripheral blood were co-cultivated for 4 d with the intra-peritoneal lymphocytes, and a cytokine assay was performed.
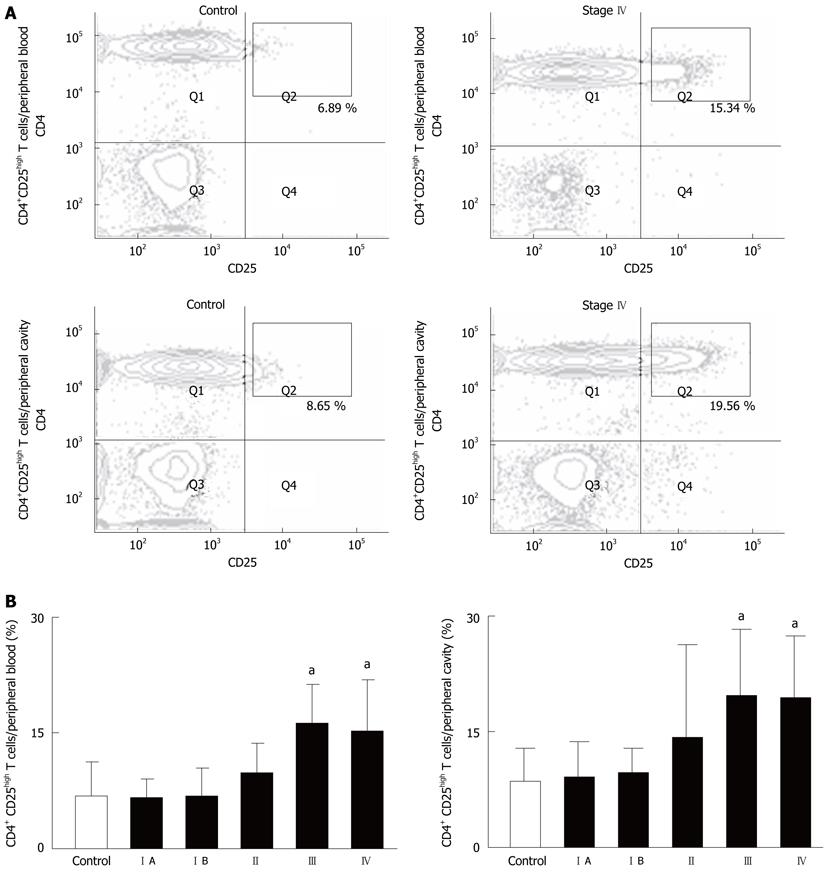
RESULTS: At gastrectomy, CCR7- CD45RA- CD8+ effector memory T cells were observed in the peritoneal cavity. The frequency of CD4+ CD25 high T cells in both the peripheral blood and peritoneal cavity was elevated in patients at advanced stage [control vs stage IV in the peripheral blood: 6.89 (3.39-10.4) vs 15.34 (11.37-19.31), P < 0.05, control vs stage IV in the peritoneal cavity: 8.65 (5.28-12.0) vs 19.56 (14.81-24.32), P < 0.05]. On the other hand, the suppression was restored with CD4+ CD25high T cells from their own peripheral blood. This study is the first to analyze lymphocyte and cytokine production in the peritoneal cavity in patients with gastric cancer. Immune regulation at advanced stage is reversible at the point of gastrectomy.
CONCLUSION: The immunological milieu in the peritoneal cavity of patients with advanced gastric cancer elicited a Th2 response even at gastrectomy, but this response was reversible.
- Citation: Yoneda A, Ito S, Susumu S, Matsuo M, Taniguchi K, Tajima Y, Eguchi S, Kanematsu T, Nagata Y. Immunological milieu in the peritoneal cavity at laparotomy for gastric cancer. World J Gastroenterol 2012; 18(13): 1470-1478
- URL: https://www.wjgnet.com/1007-9327/full/v18/i13/1470.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i13.1470
Tumor progression is governed not only by the genetic changes intrinsic to cancer cells, but also by epigenetic and environmental factors. Therefore, neoplastic cell factors and biophylactic side factors such as immune reactions are interacting in the survival and development of micrometastasis. Increasing evidence gleaned from studies in immune-compromised hosts suggests that the cellular mechanisms of immunosurveillance influence tumor development. There are several lines of research which indicate the critical role of the immune system in controlling the growth of malignant cells[1-5]. Thus, impairment of anti-tumor immunity, which leads to immunologic toleration of malignant cells, contributes to the development and progression of peritoneal metastasis[6]. The elimination phase of the cancer immunosurveillance mechanism is thought to be a continuous process, and local control of metastatic invasion by the immune system may be critical for survival. However, the role of lymphocytes in the peritoneal cavity for anti-tumor immunity in gastric cancer patients is unknown[7].
Studies in rodents have demonstrated that adoptive immunotherapy with antigen-specific CD8+ T cells is effective for cancer, and there is evidence that this approach has therapeutic activity in humans[8-10]. Memory T cells circulate throughout all tissues of the body and are primed to rapidly produce secondary immune responses upon antigen challenge[11]. The nature of the cells that mediate the different facts of immunological memory remains unresolved. Natural killer T cells are a specialized subset of T cells. They express T-cell and natural killer-lineage cell surface markers and key cytokines, which regulate the course of the immune response. There are many mechanisms that regulate and dampen the immune response to cancers[12-15]. Regulatory T cells protect the host from autoimmune disease by suppressing self-reactive immune cells. As such, regulatory T cells may also block antitumor immune responses. Regulatory T cells have been an active research area in basic as well as in clinical immunology[16-18]. Th1 immune responses are considered to be essential for eradicating malignant cells. Based on the cytokine profile, interferon-gamma is a Th1 cytokine with an antitumor effect. Interleukin-10, a Th2 cytokine, inhibits Th1 immune responses and enhances the production of other Th2 cytokines[19-22].
In order to clarify the clinical significance of the host immune response within the peritoneal cavity in patients with gastric cancer, we conducted an immunological analysis of the peritoneal lavage obtained from patients at the time of gastrectomy.
A total of 75 patients (50 males and 25 females; mean age: 64.3 years) were included in this study. Sixty-four patients were histologically diagnosed as having gastric cancer. Among these, 56 had gastrectomy, 2 underwent bypass operation, and 6 had exploratory laparotomy. Eleven patients who underwent laparoscopic cholecystectomy for benign disease acted as controls. The resected specimens were histologically examined by hematoxylin and eosin staining according to the general rules of the Japanese Classification of Gastric Carcinoma[23]. The investigation protocol was approved by the Institutional Review Board of the Nagasaki University School of Medicine (#14122694). Written informed consent was obtained from all patients. The stages of gastric cancer patients were as follows: stage IA, n = 25 patients; stage IB, n = 13; stage II, n = 7; stage III, n= 7; and stage IV, n = 12. The clinicopathological features of the patients are shown in Table 1.
| Variables | No. of patients |
| Total cases | 64 |
| Age (yr) | 67.5 ± 2.8 |
| Sex (male/female) | 42/22 |
| Depth of tumor invasion | |
| T1 | 32 |
| T2 | 20 |
| T3 | 9 |
| T4 | 3 |
| Lymphnode metastasis | |
| N0 | 34 |
| N1 | 12 |
| N2 | 14 |
| N3 | 4 |
| Peritoneal metastasis | |
| Absent | 56 |
| Present | 8 |
| Cytology | |
| Negative | 57 |
| Positive | 7 |
| Stage | |
| Stage IA | 25 |
| Stage IB | 13 |
| Stage II | 7 |
| Stage III | 7 |
| Stage IV | 12 |
Endotracheal general anesthesia was induced and 10 mL of peripheral blood was taken from all patients. Four hundred milliliter of physiological saline was poured into the peritoneal cavity prior to manipulation of the tumor, and was recovered after being gently stirred. Half of the peritoneal lavage was allocated for conventional cytology and carcinoembryonic antigen (CEA) analysis by an enzyme-linked immunosorbent assay. The other half of the peritoneal lavage was immediately centrifuged at 2000 rpm for 10 min, and the supernatants were assayed for CEA values. The peritoneal CEA levels were then measured using an enzyme immunoassay kit (IMx-SERECT CEA, Dainabot, Tokyo) and the protein concentration was determined using a protein assay kit (Bio-Rad, Richmond, CA, United States). The cell component was used for lymphocyte analysis. Lymphocytes from peripheral blood were isolated by density centrifugation over Ficoll-PaqueTM gradients (Amersham, Uppsala, Sweden).
The following monoclonal antibodies were used in the present study: fluorescein isothiocyanate (FITC)-conjugated anti-CD8, FITC-CD25, FITC-CD45RA, phycoerythrin (PE)-conjugated anti-CD4, PE-CD56, PE-CCR7, PE-IFN-γ, PE-IL-10, PE-Foxp3, cychrome (Cy)-conjugated anti-CD3, and Cy-CD8 (BD Pharmingen, San Diego, CA, United States). Single-cell suspensions were stained in phosphate-buffered saline-1% fetal calf serum at saturating concentrations according to standard procedures. Flow cytometry was performed on the BD BiosystemsFACSCanto II system (BD Biosciences, San Diego, CA, United States), and FACSDiva software (BD Biosciences, San Diego, CA, United States) was used for analysis. All analyses of T cells were carried out after gating by CD3. The ratio of the percentage of CD4 and CD8 cells was represented as the CD4/CD8 ratio.
Intracellular staining for Foxp3 was performed using the Human Foxp3 Buffer set (BD Pharmingen, San Diego, CA, United States) according to the manufacturer’s protocol.
Anti-IFN-γ-PE and anti-IL-10-PE mAbs were used for the intracellular analysis of cytokine production. Peripheral and intra-peritoneal lymphocytes were activated with 10 ng/mL phorbol 12-myristate-13-acetate (PMA), 0.5 μg/mL Ionomycin, and 1 μL/mL GolgiPlug (BD Pharmingen, San Diego, CA, United States) for 4 h. Cells were washed, fixed and permeabilized by Cytofix/Cytoperm solution (BD Pharmingen, San Diego, CA, United States), and stained with titrated amounts of cytokine-specific antibodies.
Next, the CD4+ CD25 + T cells were isolated from peripheral blood by magnetic beads (Miltenyi Biotech,BergischGladbach, Germany). These CD4+ CD25 + T cells were mixed with intraperitoneal lymphocytes at a ratio of 1:10 and co-cultivated for 4 d in RPMI with 10% FBS. The CD4+ CD25- T cells were co-cultivated with intraperitoneal lymphocytes as controls. The cytokine assay was performed by the intracellular cytokine method after 4 d of co-cultivation.
The statistical analysis was performed using the Kruskal-Wallis test (non-parametric ANOVA) using a personal computer and the StatViewV.5.0 software package (SAS Institute, Cary, NC, United States). P values less than 0.05 were considered to indicate statistical significance.
For the interaction between peripheral blood and the peritoneal cavity, we investigated the CEA values in both serum and peritoneal lavage at the time of surgery. The serum CEA values were elevated only in patients with stage IV disease. On the other hand, the values in peritoneal lavage were found to be elevated even at stage III, and they were also related to the clinical stage (Table 2).
| Source | Control | Stage I A | Stage I B | Stage II | Stage III | Stage IV |
| CEA | ||||||
| PB (ng/mL) | Not tested | 2.09 (1.39-2.78) | 2.03 (0.96-3.1) | 3.06 (2.04-4.07) | 2.54 (0.38-4.69) | 7.98 (1.18-15.82) |
| PL (ng/g protein) | 56.53 (21.82-91.24) | 44.17 (27.37-60.96) | 61.95 (11.98-111.91) | 83.14 (7.31-187.54) | 262.63 (7.26-517.26) | 1234.00 (87.77-2380.22) |
| CD4/CD8 | ||||||
| PB (ratio) | 5.379 (2.705-8.052) | 5.595 (3.224-7.967) | 4.571 (2.057-7.086) | 5.277 (1.369-9.184) | 7.999 (3.366-12.632) | 4.156 (2.228-6.083) |
| PL (ratio) | 0.494 (0.338-0.649) | 0.553 (0.421-0.685) | 0.697 (0.511-0.883) | 0.638 (0.395-0.881) | 1.242 (0.961-1.522) | 1.158 (0.907-1.408) |
| CD45RA-/CCR7- | ||||||
| PB (%) | 60.43 (46.42-74.44) | 58.29 (48.93-67.64) | 53.92 (32.65-75.2) | 57.36 (42.01-72.71) | 49.01 (29.31-68.71) | 45.73 (32.79-58.67) |
| PL (%) | 81.17 (81.12-93.22) | 81.67 (76.35-87.01) | 76.2 (59.43-92.96) | 72.3 (61.01-83.58) | 68.36 (58.70-78.02) | 51.92 (38.34-65.50) |
| NKT | ||||||
| PB (%) | 9.19 (5.83-12.54) | 7.59 (5.63-9.56) | 9.47 (4.41-14.53) | 10.71 (1.55-19.87) | 5.43 (0.54-10.33) | 7.16 (3.95-10.3) |
| PL (%) | 18.1 (9.83-26.37) | 17.25 (13.54-20.97) | 15.74 (9.23-22.25) | 15.38 (7.71-23.04) | 9.66 (1.2-18.11) | 9.91 (6.94-12.88) |
After purification of lymphocytes from peritoneal lavage, we investigated the phenotypes of lymphocytes in both peripheral blood and the peritoneal cavity. The mean value of the CD4/CD8 ratio for all patients was 2.17 in peripheral blood. The CD8+ T cells were dominant in the peritoneal cavity and the CD4/CD8 ratio was reversed. The ratio in patients with stage III or IV was significantly higher than in stage I or control patients (Table 2).
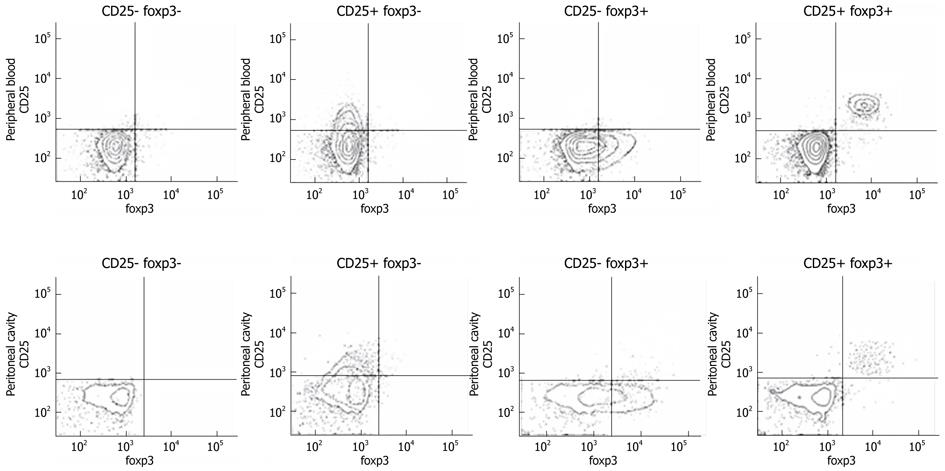
The CCR7- CD45RA- CD8+ T cells were counted as effector memory T cell subsets. The percentage of effector memory T cells in the peritoneal cavity was higher than that in peripheral blood. However, the percentage decreased in association with the clinical stage (Table 2). The CD3+CD56+ cells were measured as natural killer T cells. The percentage of these cells in the peritoneal lavage was also low in patients with stage III or stage IV (Table 2). As the co-staining of foxp3 and CD25 revealed a high correlation between both populations, CD25high was used following cytokine producing assays (Figure 1). The frequency of CD4+ CD25 high T cells in patients with advanced stage cancer was higher than that in control patients in both peripheral blood and the peritoneal cavity (Figure 2A and B).
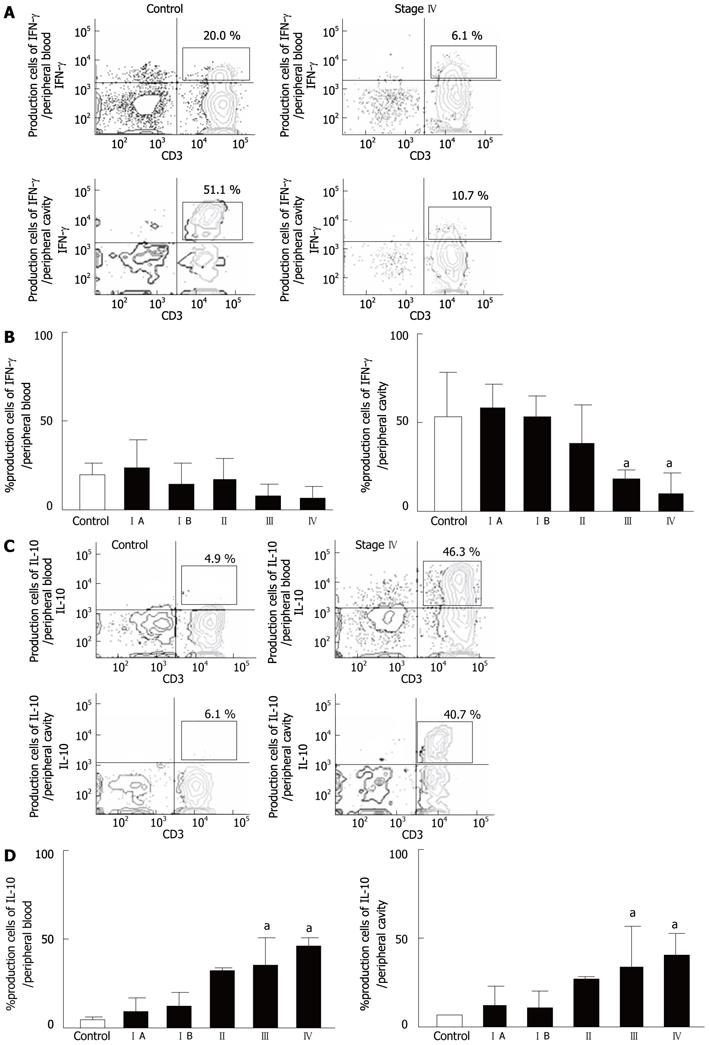
The cytokine production from CD3+ T cells after stimulation with PMA + ionomycin was evaluated by a cytokine production assay. The lymphocytes in the peritoneal cavity were more sensitive for the production of IFN-γ than those in the peripheral blood. The ratio of IFN-γ producing cells in the peritoneal cavity was significantly lower in patients with advanced stage disease in comparison to the controls (Figure 3A and B). The ratio of IL-10 producing cells in the peritoneal cavity in patients with advanced stages was higher in comparison to the controls (Figure 3C and D).
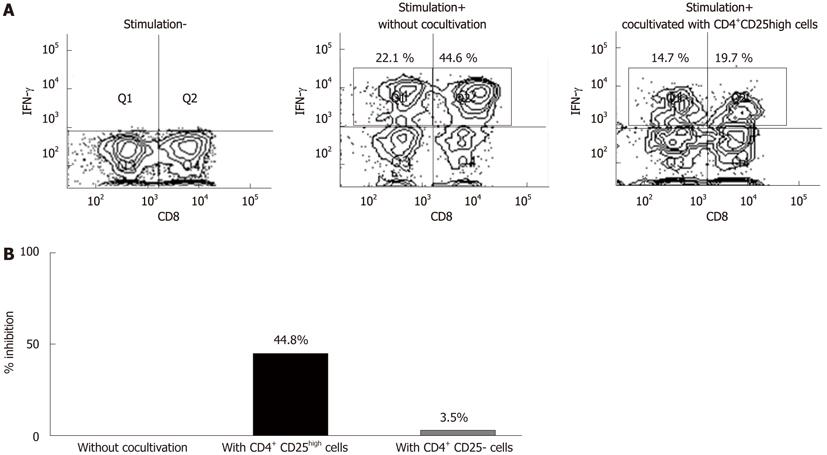
In order to investigate whether the suppression of IFN-γ production from T cells in the peritoneal cavity at advanced stages was caused by CD4+ CD25high T cells, further assays were performed. The IFN-γ production of CD8+ T cells was suppressed in intra-peritoneal lymphocytes co-cultivated with isolated CD4+ CD25high T cells from self-peripheral blood (Figure 4A). No inhibition was seen when the lymphocytes were co-cultivated with CD4+ CD25- cells (Figure 4B).
The peritoneal cavity is a compartment in which the immunological host-tumor interaction can occur[24]. This study investigated lymphocytes in the peritoneal cavity of patients with gastric cancer in relation to anti-tumor immunity. Some tumors can acquire the ability to down-regulate immune responses and exploit this action to promote tumor cell proliferation, survival, and invasion[10,25]. Therefore, the presence of leukocytes in the peritoneal cavity may be a consequence of an immune response that favors either dissemination of tumor cells or a protective host response. Malignant ascites has been used as a common source of immunological analysis in previous reports[11,26]. To the best of our knowledge, there are no reports describing the lymphocyte and cytokine production ability in peritoneal lavage from patients with gastric cancer at the time of gastrectomy.
In our initial experiments, the CEA values in peritoneal lavage were found to correlate with the clinical stages. Interestingly, the CEA values were elevated even in cases without serosal invasion. This result suggests that some fragments of cancer cells may spread throughout the peritoneal cavity and induce an immune reaction between the tumor and host[26,27].
The frequency of CD4+ T cells in all patients was higher than that of CD8+ T cells in peripheral blood, but this pattern was reversed in peritoneal lavage fluid. CD8+ T cells were dominant in the peritoneal cavity. Our data suggested that the immunological environment in the peripheral blood is different from that in the peritoneal cavity. There were significant differences in the CD4/CD8 ratio in the peritoneal cavity between gastric cancer patients at advanced stage and control patients. Cancer progression may have an effect on the balance of the T cell population in the peritoneal cavity.
Immunological memory is demonstrated by following T cell subsets: lymph-node-homing cells lacking inflammatory and cytotoxic function (defined as central memory T cells, CCR7+ CD45RA-) and tissue-homing cells endowed with various effector functions (defined as effector memory T cells, CCR7- CD45RA-). These two subsets allow for the division of labor among memory cells. Effector memory T cells represent a readily available pool of antigen-primed cells that can enter peripheral tissues to mediate inflammatory reactions or cytotoxicity, thus rapidly containing invasive pathogens and cancer antigens[11,28-31]. Our data show that CD8+ effector memory T cells were rich in the peritoneal cavity. This indicates the migration of effector memory cells from the peripheral blood to local sites. However, in advanced cases, the frequency of CD8+ effector memory cells in the peritoneal lavage was low. These results suggest that the peritoneal cavity exerts the local immune response, more than peripheral blood.
Natural killer T cells, a unique lymphocyte subpopulation, are characterized by the expression of invariant antigen receptors[12,13]. Natural killer T cells have been suggested to serve as a bridge between innate and acquired immunity[14,15]. However, the mechanisms underlying the anti-tumor effect of human natural killer T cell-mediated immunotherapy remain unclear so far. The frequency of natural killer T cells was lower in patients with stages III and IV than in control patients. Therefore, a decrease in the number of natural killer T cells in the peritoneal cavity may be one aspect of the interaction between host-immunity and cancer progression.
Recent studies have shown that CD4+ CD25high foxp3+ T cells exhibiting regulatory/suppressive properties are naturally present in humans[16-18]. The roles of regulatory T cells have been active topics of research in both basic and clinical immunology. Naturally-occurring regulatory T cells represent a small fraction (5%-6%) of the overall CD4+ T cell population, and play an important role in down-regulation of the response of T cells to foreign and self antigens[31]. The depletion of this subset of regulatory T cells in normal hosts results in various autoimmune diseases because the host immune system is unchecked and attacks the body’s own tissues[28]. Despite the importance of these cells in preventing autoimmune disease, their presence in the tumor microenvironment diminishes anti-tumor immune responses[32-36].
Within the CD4+ T cell subset, there is a population of naturally occurring foxp3+ T cells that are defined as regulatory T cells. These cells can be identified as CD4+foxp3+ T cells by flow cytometry. However, because foxp3 is intracellular and requires permeabilization of cells for detection by flow cytometry, regulatory T cells are isolated as CD4+CD25high T cells, which were shown to have functional suppressive abilities in our co-culture experiments[37]. In the present study, the mean percentage of CD4+ CD25high T cells in the peritoneal cavity in advanced gastric cancer patients was higher than that of control patients. After the co-cultivation of the self- CD4+ CD25high T cell population of intra-peritoneal lymphocytes, the production of IFN-γ was inhibited.
IFN-γ, a Th1 cytokine, not only exerts an anti-tumor effect, but also inhibits the proliferation of Th2 clones[19-20]. IL-10, a Th2 cytokine, suppresses the synthesis of Th1 cytokines such as IFN-γ[21-22]. This study showed that the production of intracellular cytokines in the peritoneal cavity was higher than that in the peripheral blood after appropriate stimulation. IFN-γ production was down-regulated in advanced cases, but not in the controls and stage I patients. On the other hand, IL-10 production was up-regulated, which revealed the switch of Th1 and Th2 responses in the peritoneal cavity of these patients. IFN-γ production in intra-peritoneal lymphocytes was suppressed after co-cultivation with self-CD4+ CD25high T cells, but not CD4+ CD25- T cells. Interestingly, the replacement of CD4+ CD25- T cells for CD4+ CD25high T cells could recover the production of IFN-γ in intra-peritoneal lymphocytes.
The peritoneal cavity is a compartment in which immunological host-tumor interactions can occur. Neoplastic cell factors and biophylactic side factors such as immune reactions are interacting in the survival and development of micrometastasis. However, the role of lymphocytes in the peritoneal cavity of gastric cancer patients is unclear.
Clinical and experimental studies have established that leukocyte infiltrations around tumors promote the development or regression of solid tumors, butwhether the organ-specific cellular and molecular programs promote tumor growth or exhibit anti-tumor immunity by leukocytes are incompletely understood. Recent studies have shown that CD4+ CD25high foxp3+ T cells exhibiting regulatory/suppressive properties are naturally present in humans. The roles of regulatory T cells have been active topics of research in both basic and clinical immunology.
In most previous studies, malignant ascites have been a common source of immunological analysis. However, there are no reports describing the lymphocyte and cytokine production ability in peritoneal lavage from patients with gastric cancer at the time of gastrectomy. In the present study, CD4+ CD25high T cells were found to be increased in the peritoneal cavity of advanced gastric cancer patients, but in the co-cultivation of the self- CD4+ CD25high T cell population of intra-peritoneal lymphocytes, the production of IFN-γwas inhibited.
Peritoneal lavage samples from patients with gastric cancer are more susceptible than peripheral blood for monitoring the interaction between the host’s immune system and tumor cells.
Regulatory T cells: Regulatory T cells contribute to the maintenance of immunologic self-tolerance. Recent reports underscore that regulatory T cells not only play a role in the maintenance of immunotolerance but are also potent inhibitors of antitumor immune responses.
The authors have investigated T-cells isolated from peripheral blood and peritoneal lavage in patients with gastric cancer and controls. Main findings are that in stage III and IV gastric cancers the lavage fluid contains less CD8 memory cells, NKT cells and more CD25high regulatory T cells.
Peer reviewer: Rasmus Goll, MD, Department of Gastroenterology, University Hospital of North Norway, Sykehusveien, Tromso 9038, Norway
S- Editor Gou SX L- Editor Webster JR E- Editor Zhang DN
| 1. | Huber V, Fais S, Iero M, Lugini L, Canese P, Squarcina P, Zaccheddu A, Colone M, Arancia G, Gentile M. Human colorectal cancer cells induce T-cell death through release of proapoptotic microvesicles: role in immune escape. Gastroenterology. 2005;128:1796-1804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 412] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 2. | Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pagès C, Tosolini M, Camus M, Berger A, Wind P. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4318] [Cited by in RCA: 4902] [Article Influence: 258.0] [Reference Citation Analysis (0)] |
| 3. | Susumu S, Nagata Y, Ito S, Matsuo M, Valmori D, Yui K, Udono H, Kanematsu T. Cross-presentation of NY-ESO-1 cytotoxic T lymphocyte epitope fused to human heat shock cognate protein 70 by dendritic cells. Cancer Sci. 2008;99:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Koizumi K, Hojo S, Akashi T, Yasumoto K, Saiki I. Chemokine receptors in cancer metastasis and cancer cell-derived chemokines in host immune response. Cancer Sci. 2007;98:1652-1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Tsujimoto H, Ono S, Ichikura T, Matsumoto Y, Yamamoto J, Hase K. Roles of inflammatory cytokines in the progression of gastric cancer: friends or foes? Gastric Cancer. 2010;13:212-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Nan KJ, Wei YC, Zhou FL, Li CL, Sui CG, Hui LY, Gao CG. Effects of depression on parameters of cell-mediated immunity in patients with digestive tract cancers. World J Gastroenterol. 2004;10:268-272. [PubMed] |
| 7. | Atanackovic D, Block A, de Weerth A, Faltz C, Hossfeld DK, Hegewisch-Becker S. Characterization of effusion-infiltrating T cells: benign versus malignant effusions. Clin Cancer Res. 2004;10:2600-2608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Cheever MA, Greenberg PD, Fefer A. Specificity of adoptive chemoimmunotherapy of established syngeneic tumors. J Immunol. 1980;125:711-714. [PubMed] |
| 9. | Dudley ME, Wunderlich JR, Robbins PF, Yang JC, Hwu P, Schwartzentruber DJ, Topalian SL, Sherry R, Restifo NP, Hubicki AM. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science. 2002;298:850-854. [PubMed] |
| 10. | Dudley ME, Wunderlich JR, Yang JC, Sherry RM, Topalian SL, Restifo NP, Royal RE, Kammula U, White DE, Mavroukakis SA. Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. J Clin Oncol. 2005;23:2346-2357. [PubMed] |
| 11. | Sallusto F, Lenig D, Förster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4426] [Cited by in RCA: 4562] [Article Influence: 175.5] [Reference Citation Analysis (0)] |
| 12. | Taniguchi M, Harada M, Kojo S, Nakayama T, Wakao H. The regulatory role of Valpha14 NKT cells in innate and acquired immune response. Annu Rev Immunol. 2003;21:483-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 537] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 13. | Brigl M, Brenner MB. CD1: antigen presentation and T cell function. Annu Rev Immunol. 2004;22:817-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 808] [Cited by in RCA: 823] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 14. | Taniguchi M, Seino K, Nakayama T. The NKT cell system: bridging innate and acquired immunity. Nat Immunol. 2003;4:1164-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 189] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 15. | Motohashi S, Nakayama T. Clinical applications of natural killer T cell-based immunotherapy for cancer. Cancer Sci. 2008;99:638-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531-562. [PubMed] |
| 17. | Linehan DC, Goedegebuure PS. CD25+ CD4+ regulatory T-cells in cancer. Immunol Res. 2005;32:155-168. [PubMed] |
| 18. | Imai H, Saio M, Nonaka K, Suwa T, Umemura N, Ouyang GF, Nakagawa J, Tomita H, Osada S, Sugiyama Y. Depletion of CD4+CD25+ regulatory T cells enhances interleukin-2-induced antitumor immunity in a mouse model of colon adenocarcinoma. Cancer Sci. 2007;98:416-423. [PubMed] |
| 19. | Fernandez-Botran R, Sanders VM, Mosmann TR, Vitetta ES. Lymphokine-mediated regulation of the proliferative response of clones of T helper 1 and T helper 2 cells. J Exp Med. 1988;168:543-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 276] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Rayman P, Wesa AK, Richmond AL, Das T, Biswas K, Raval G, Storkus WJ, Tannenbaum C, Novick A, Bukowski R. Effect of renal cell carcinomas on the development of type 1 T-cell responses. Clin Cancer Res. 2004;10:6360S-6366S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 452] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 21. | Fiorentino DF, Zlotnik A, Vieira P, Mosmann TR, Howard M, Moore KW, O'Garra A. IL-10 acts on the antigen-presenting cell to inhibit cytokine production by Th1 cells. J Immunol. 1991;146:3444-3451. [PubMed] |
| 22. | Bai XF, Zhu J, Zhang GX, Kaponides G, Höjeberg B, van der Meide PH, Link H. IL-10 suppresses experimental autoimmune neuritis and down-regulates TH1-type immune responses. Clin Immunol Immunopathol. 1997;83:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma--2nd English edition--response assessment of chemotherapy and radiotherapy for gastric carcinoma: clinical criteria. Gastric Cancer. 2001;4:1-8. [PubMed] |
| 24. | Olszewski WL, Kubicka U, Tarnowski W, Bielecki K, Ziolkowska A, Wesolowska A. Activation of human peritoneal immune cells in early stages of gastric and colon cancer. Surgery. 2007;141:212-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Mori T, Shimizu M, Iwaguchi T. Immunological characterization and clinical significance of low mobility cells appearing in the peripheral blood mononuclear cells of cancer patients. Eur J Cancer Clin Oncol. 1988;24:1463-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Marutsuka T, Shimada S, Shiomori K, Hayashi N, Yagi Y, Yamane T, Ogawa M. Mechanisms of peritoneal metastasis after operation for non-serosa-invasive gastric carcinoma: an ultrarapid detection system for intraperitoneal free cancer cells and a prophylactic strategy for peritoneal metastasis. Clin Cancer Res. 2003;9:678-685. [PubMed] |
| 27. | Jung M, Jeung HC, Lee SS, Park JY, Hong S, Lee SH, Noh SH, Chung HC, Rha SY. The clinical significance of ascitic fluid CEA in advanced gastric cancer with ascites. J Cancer Res Clin Oncol. 2010;136:517-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2123] [Cited by in RCA: 2334] [Article Influence: 111.1] [Reference Citation Analysis (0)] |
| 29. | Berger C, Jensen MC, Lansdorp PM, Gough M, Elliott C, Riddell SR. Adoptive transfer of effector CD8+ T cells derived from central memory cells establishes persistent T cell memory in primates. J Clin Invest. 2008;118:294-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 698] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 30. | Ye SW, Wang Y, Valmori D, Ayyoub M, Han Y, Xu XL, Zhao AL, Qu L, Gnjatic S, Ritter G. Ex-vivo analysis of CD8+ T cells infiltrating colorectal tumors identifies a major effector-memory subset with low perforin content. J Clin Immunol. 2006;26:447-456. [PubMed] |
| 31. | Wang HY, Wang RF. Regulatory T cells and cancer. Curr Opin Immunol. 2007;19:217-223. [PubMed] |
| 32. | Nishikawa H, Kato T, Hirayama M, Orito Y, Sato E, Harada N, Gnjatic S, Old LJ, Shiku H. Regulatory T cell-resistant CD8+ T cells induced by glucocorticoid-induced tumor necrosis factor receptor signaling. Cancer Res. 2008;68:5948-5954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 33. | Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, Evdemon-Hogan M, Conejo-Garcia JR, Zhang L, Burow M. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3582] [Cited by in RCA: 3875] [Article Influence: 184.5] [Reference Citation Analysis (0)] |
| 34. | Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, Nomura T, Sakaguchi S. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2013] [Cited by in RCA: 2245] [Article Influence: 132.1] [Reference Citation Analysis (0)] |
| 35. | Onishi Y, Fehervari Z, Yamaguchi T, Sakaguchi S. Foxp3+ natural regulatory T cells preferentially form aggregates on dendritic cells in vitro and actively inhibit their maturation. Proc Natl Acad Sci USA. 2008;105:10113-10118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 558] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 36. | Stanzer S, Dandachi N, Balic M, Resel M, Samonigg H, Bauernhofer T. Resistance to apoptosis and expansion of regulatory T cells in relation to the detection of circulating tumor cells in patients with metastatic epithelial cancer. J Clin Immunol. 2008;28:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Gnjatic S, Altorki NK, Tang DN, Tu SM, Kundra V, Ritter G, Old LJ, Logothetis CJ, Sharma P. NY-ESO-1 DNA vaccine induces T-cell responses that are suppressed by regulatory T cells. Clin Cancer Res. 2009;15:2130-2139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |