Published online Nov 7, 2011. doi: 10.3748/wjg.v17.i41.4619
Revised: June 9, 2011
Accepted: June 16, 2011
Published online: November 7, 2011
AIM: To evaluate the effect of hands-on training of gastroenterology fellows in gastric polypectomy using an ex vivo simulator.
METHODS: Eight gastroenterology fellows at Mackay Memorial Hospital, Taipei were evaluated in gastric polypectomy techniques using a pig stomach with artificial polyps created by a rubber band ligation device. The performance of four second year (year-2) fellows who had undergone one year of clinical training was compared with that of four first year (year-1) fellows both before and after a 4-h workshop using the ex vivo simulator. The workshop allowed for hands-on training in the removal of multiple artificial polyps and the placement of hemoclips at the excision site. Evaluation included observation of technical skills, procedure time, and the fellows’ confidence scale.
RESULTS: One week after the workshop, the year-1 fellows were re-evaluated and had significantly improved mean performance scores (from 17.9 ± 1.8 to 22.5 ± 0.7), confidence scale (from 4.5 ± 1.0 to 7.8 ± 0.5) and procedure time (from 615.0 ± 57.4 s to 357.5 ± 85.0 s) compared with their baseline performance. After 4 h of training using the ex vivo simulator, the skills of the year-1 fellows were statistically similar to those of the year-2 fellows.
CONCLUSION: Use of this ex vivo simulator significantly improved the endoscopic gastric polypectomy skills of gastroenterology fellows who had not had previous clinical training in gastric polypectomy.
-
Citation: Chen MJ, Lin CC, Liu CY, Chen CJ, Chang CW, Chang CW, Lee CW, Shih SC, Wang HY. Training gastroenterology fellows to perform gastric polypectomy using a novel
ex vivo model. World J Gastroenterol 2011; 17(41): 4619-4624 - URL: https://www.wjgnet.com/1007-9327/full/v17/i41/4619.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i41.4619
Interventional endoscopy continues to advance, requiring that endoscopists obtain practical training in skills needed for therapeutic intervention. This has traditionally been accomplished by having trainees perform endoscopy on patients under close supervision. However, the use of animal models is a safe way to practice the techniques used in therapeutic endoscopy[1]. Since the mid-1990s, an ex vivo porcine-tissue simulator has been widely used in many hands-on training programs. It has been shown to facilitate skill in a variety of endoscopic procedures, such as hemostasis for arterial or variceal bleeding[2,3]. It is also useful in training trainers for endoscopy programs[4].
Endoscopic polypectomy is one such skill that must be acquired, including removal of gastric polyps incidentally discovered during endoscopic evaluations. Hyperplastic polyps are by far the most common histologic type of gastric polyp, occurring most commonly in the antrum[5]. When such polyps are larger than 1 cm, the risk of neoplastic transformation increases. Therefore, endoscopic polypectomy may be necessary both for accurate diagnosis and as definitive treatment[6,7]. Larger polyps, however, may be more difficult for inexperienced endoscopists to manage, as are those in more challenging locations. Fellows in gastroenterology training programs need to become familiar with the practical skills required, both in removing the polyp and closing the resulting mucosal defect[8].
We developed a method to simulate artificial polyps in an ex vivo pig-stomach model for use in our gastroenterology fellowship training program. As far as we are aware, this novel approach has not previously been described. We designed this study to evaluate this model in training gastroenterology fellows.
The study group comprised eight gastroenterology fellows at Mackay Memorial Hospital, Taipei, Taiwan, four in the second year (year-2) and four in the first year (year-1) of subspecialty training. Year-2 fellows had already learned to perform endoscopic gastric polypectomy in patients under the supervision of an experienced supervisor certified by the Digestive Endoscopic Society of Taiwan. Year-1 fellows were certified in diagnostic endoscopy after one year of training but had no prior experience performing gastric polypectomy, although they had assisted other endoscopists in placing hemoclips. None of the eight fellows had ever used an ex vivo pig-stomach simulator prior to this study. One instructor conducted workshop training, and two reviewers evaluated the fellows’ skill in performing polypectomy. The instructor and reviewers each had more than 10 years’ experience in interventional endoscopy and were certified as instructors by the Digestive Endoscopic Society of Taiwan.
The ex vivo pig-stomach simulator was a modified version of the compactEASIE model[2,3]. Fresh pig stomachs, including short segments of the lower esophagus and duodenum, were purchased from a slaughterhouse early in the morning of the day they were to be used and were stored in cool saline until preparation. For the simulator, the stomach was placed in a hand-made container composed of layered polystyrene boards cut so as to accommodate the esophagus, stomach, and duodenum (Figure 1). It was irrigated copiously with tap water until clean. Defects in the viscera were closed using appropriately sized Kelly forceps. A flexible overtube (Sumitoma Corp, Tokyo, Japan) with an air-tight valve was inserted into the short segment of the lower esophagus and a plastic band placed to seal the space between the overtube and esophagus. The distal end of the small bowel was closed with Kelly forceps for a good air-tight effect. An electronic-conduction pad was placed between the stomach and the polystyrene board, and an electrosurgical generator (VIO 200D; ERBE Corp., Tuebingen, Germany) with standard settings was used.
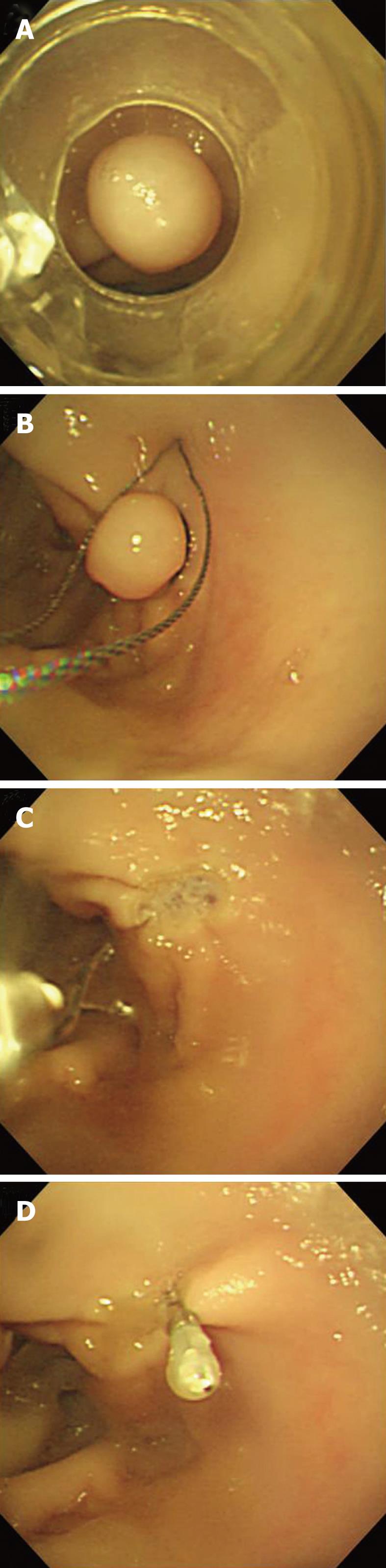
The instructor created simulated gastric polyps by using a pneumatically-activated esophageal variceal ligation device (MD-48709; Sumitoma Corp, Tokyo, Japan). For the skills assessment portion of the study, a polyp was created in the cardia in essentially the same location for each fellow being evaluated (Figure 2A). The endoscope (GIF Q230; Olympus Optical Co. Ltd, Tokyo, Japan) and other equipment (polypectomy snare: SD-8P-1; Olympus Optical Co. Ltd, Tokyo, Japan; hemoclip applicator: HX-100 LR; Olympus Optical Co. Ltd, Tokyo, Japan) were retired from clinical use and all used exclusively in animals at the time of the study. The Institutional Review Board at Mackay Memorial Hospital approved this training project.
Fellows were assessed for their ability to set up the equipment, to remove the entire polyp safely and to close the mucosal defect so as to prevent hemorrhage or perforation. They were required to advance the snare to encircle the target tissue and then transect the polyp with an electrosurgical cutting device attached to the snare. They then had to ensure closure of the mucosal defect by placing hemoclips, which required understanding of how to load the clips, and also direct an assistant in proper placement (Figure 2B-D).
Following a baseline skills assessment, the four year-1 fellows attended a 4-h workshop led by one instructor, with an assistant to handle the instruments. There was an initial 1-h lecture about gastric polypectomy, followed by the instructor demonstrating the procedure for 1 h, including proper techniques, equipment settings, and communication with the assistant. The final 2 h involved hands-on practice by the fellows (30 min each). For this session, multiple gastric polyps were artificially created ahead of time in various locations within the porcine stomach using a preloaded multiband esophageal variceal ligation device (Speedband Superview Super 7; Microvasive, MA, United States). This allowed each fellow to practice removing a number of simulated polyps for training (Figure 3). While one fellow was practicing, the other three acted as observers and benefitted by hearing the instructions, feedback, and correction of technical errors given to the others.
Skills assessments were all conducted by two reviewers who had not conducted the training session, and again with an assistant for the actual procedure. All eight fellows were assessed at baseline. A second evaluation was conducted for year-1 fellows a week after they had attended the workshop. Before each evaluation, fellows indicated on a 10-point visual analogue scale their own degree of confidence in performing the procedure. The reviewers met before each evaluation session to standardize the evaluation criteria. Each independently completed a standard assessment checklist for each fellow. The time to complete the procedure was recorded. The standard rating score was based on a 5-point score (1-5 from poor to excellent) for each of 5 items: (1) setting up and testing the equipment; (2) issuing correct instructions to the assistant; (3) proper localization of the polyp; (4) removal of the polyp with minimal tissue injury; and (5) successful application of the hemoclips. The scores for each item were summed for the final performance score.
The primary aim was to assess changes in performance score, procedure time, and confidence among the year-1 fellows before and after workshop training. This was done by using paired t tests. The results for the year-1 fellows at both baseline and again after training were also compared with those of the year-2 fellows, using unpaired t tests. Date was analyzed using SPSS 11.0 (SPSS Inc, Chicago, Ill). Results were considered to be statistically significant if the P value was < 0.05.
Year-1 and -2 fellows were of comparable age and academic background. Year-2 fellows had done about twice as many diagnostic endoscopies as the year-1 fellows. At baseline assessment, year-2 fellows had a significantly higher mean performance score (21.1 ± 0.9 vs 17.9 ± 1.8), confidence scale (7.8 ± 0.5 vs 4.5 ±1.0), and shorter procedure time (377.5 ± 156.3 s vs 615.0 ± 57.4 s) than year-1 fellows.
One week after the workshop using the ex vivo simulator, the year-1 fellows were re-evaluated and had significantly improved mean performance scores (from 17.9 ± 1.8 to 22.5 ± 0.7), confidence scale (from 4.5 ± 1.0 to 7.8 ± 0.5) and procedure time (from 615.0 ± 57.4 s to 357.5 ± 85.0 s)
compared with their baseline performance. The significantly improved scores were attributed to doing a better job of setting up the equipment and in communicating with the assistant (Table 1). There were no significant differences between the final assessments for the year-1 fellows and those of the year-2 fellows.
| Year-2 initialassessment | Year-1 initialassessment | Year-1 finalassessment | Pvalue1 | Pvalue2 | Pvalue3 | |
| Setting up equipment | 3.6 ± 0.5 | 3.3 ± 0.5 | 5.0 ± 0.0 | 0.160 | < 0.001 | 0.003 |
| Communication with the assistant | 4.5 ± 0.6 | 3.6 ± 0.3 | 4.6 ± 0.3 | 0.180 | 0.35 | 0.007 |
| Proper localization and snaring | 4.4 ± 0.5 | 4.0 ± 0.8 | 4.4 ± 0.5 | 0.229 | 0.50 | 0.107 |
| Removal of polyp and avoidance of tissue injury | 4.1 ± 0.3 | 4.5 ± 0.3 | 4.6 ± 0.3 | 0.104 | 0.15 | 0.091 |
| Successful application of hemoclips | 4.4 ± 0.5 | 2.6 ± 0.5 | 3.6 ± 0.9 | 0.001 | 0.088 | 0.081 |
Our study demonstrated the feasibility of using the ex vivo pig stomach with artificially created polyps to improve the practical skills of gastroenterology fellows learning the techniques of gastric polypectomy. In theory, this should minimize risks to patients, as the fellows can practice the necessary maneuvers on the ex vivo model.
The most important advantage of the method we devised is the ease with which artificial polyps can be created. A previously described method is to lift the mucosa with surgical forceps and ligate the base with a suture[9]. However, using the multiband esophageal variceal ligator to raise the tissue and band allows rapid creation of multiple polyps in different locations within the stomach and allows the fellows to practice on a variety of lesions such as they might encounter clinically. Reducing the time required to prepare the model makes it more user-friendly. The entire setup is relatively inexpensive and easily portable.
Practicing with the ex vivo simulator has several other advantages over traditional clinical training in which an instructor supervises the trainee who performs the procedure in an actual patient. Clinical endoscopy may be a prolonged and difficult procedure in some patients. If the patient is unstable, the instructor may have to take over the procedure. Even if able to carry out the entire procedure themselves, fellows may feel less free to ask questions or receive feedback in the clinical setting. Also, unlike polyps of the colon, gastric polyps are relatively uncommon, with an incidence of less than 2%[10,11]. This means that in the course of subspecialty training, a fellow is unlikely to have many opportunities to perform gastric polypectomy under supervision. The four year-2 fellows we assessed had performed only a mean of 5 gastric polypectomies, with only one having the chance to do two such procedures in the second year of training.
A satisfactory outcome for gastric polypectomy requires expertise in multiple skills, including preparation of the electrosurgical cutting device and accessories, in addition to the endoscopic techniques such as proper snaring, stretching the polyp away from the intact mucosa, safe cutting and finally application of hemoclips to close the mucosal defect. Knowing that so many skills are required puts additional pressure on trainees, especially the first few times they perform the procedure. When they have to do so in a real patient, lack of confidence may increase the risk of technical errors and unpredictable outcomes[12]. Our year-1 fellows had considerable improvement in the confidence scale from a mean score of 4.5 ± 1.0 before training to 7.8 ± 0.5 after using the simulator in the workshop. They were able to practice the procedure a number of times without fear of injuring a patient. This contention is supported by the fact that their performance scores did appear to improve after the training.
As noted above, the most obvious improvement after the workshop was in setting up the equipment and communicating with the assistant. The educational experience in this workshop transcends a “simulation experience” because it also involves lectures, student-student interaction, and interaction with a faculty member which are all in a non-simulated environment. Of course this exposure would be in addition to a formal teaching setting with mentoring, and this by no means will or can replace that. While the mean score for hemoclip application improved from baseline (2.6 ± 0.5 to 3.6 ± 0.9), it did not reach 4 points. This experience is similar to that noted by Hochberger et al[1] when they first designed the compactEASIE model. This particular technique involves more intricate maneuvers and several steps, increasing the opportunities to make mistakes. It thus appears the application of hemoclips may require more training sessions for the fellows to achieve competency, which is all the more reason for ensuring that a good simulator is available. Familiarity with loading of the device, delivery, and deployment may enhance safe and successful application[13].
The expense of conducting a hands-on workshop may be a limiting factor for some training programs. Our 4-h workshop cost about US $350 overall using our hand-made simulator, endoscopes and accessories retired from clinical practice and pig stomachs. Because this workshop was a project of our Clinical Skills Training Center, the instructor, reviewers and assistants were all volunteers, and no facility fee was needed. The Olympus GIF Q230 endoscopes, polypectomy snare, and hemoclip device were retired from our clinical service and cost almost nothing to use. The hemoclips and rubber band ligation cost US $300. The price of one hand-made simulator was US $35 and pig stomachs were US $15 each. We therefore believe this hand-made ex-vivo porcine-stomach simulator could be used by most institutions without requiring a huge capital outlay.
Our study had a number of limitations. Firstly, this was an in-house project; we didn’t recruit fellows from other sites therefore had a very small sample, precluding rigorous statistical analysis. The performance evaluations by the two reviewers were unblinded. Because we didn’t invite outside experts as reviewers, there may have been observational bias. Evaluation with a video recording of the entire procedure is an alternative blinded method, but this approach can’t adequately assess the equipment setup process or communication with the assistant. Secondary, we presume it’s a very realistic simulator to represent the task of gastric polypectomy no matter the size of polyp, techniques or procedures time and it is easily transferable to clinical care. Whether those results will translate into better clinical performance of polypectomy as the year-1 fellows continue on into the second year of training remains to be seen. A number of factors may possibly result in incomplete transfer of simulator-acquired skills to the real world[14], including differences between the training environment and the clinic, anxiety and stress of learners[15]. Conducting such a study on a larger scale with an appropriate sample size and assessment of the clinical data is therefore still necessary.
Our pilot study demonstrates the feasibility of using the ex vivo pig stomach with artificially created polyps to improve the practical skills of gastroenterology fellows learning the techniques of gastric polypectomy. The workshop allowed the year-1 fellows to improve their skills nearly to the level of those acquired by year-2 fellows who were trained clinically. In theory, this should minimize risks to patients, as the fellows can practice the necessary maneuvers on the ex vivo model. We believe this is a simple and cost-effective way to train gastroenterology fellows in endoscopic polypectomy and regard this program as preceding training in more complicated polypectomy once competent in standard removal of small and pediculated lesions.
The authors thank Wang MS, research nurse and colleagues in the Clinical Skills Training Center for the preparing the ex vivo porcine model and providing technical assistance.
Since the mid-1990s, an ex vivo porcine-tissue simulator had been widely used in many hands-on training programs. It has been shown to facilitate skill in a variety of endoscopic procedures.
Endoscopic polypectomy is one such skill that must be acquired, including removal of gastric polyps incidentally discovered during endoscopic evaluations. The authors developed a method to simulate artificial polyps in an ex vivo pig-stomach model for use in their gastroenterology fellowship training program.
The most important advantage of the method the authors devised is the ease with which artificial polyps can be created. Using the multiband esophageal variceal ligator to raise the tissue and band it allows rapid creation of multiple polyps in different locations within the stomach.
Reducing the time required to prepare the model makes it more user-friendly. The entire setup is relatively inexpensive and easily portable.
The authors should be congratulated in their efforts on this manuscript. Though the number of fellows is small, the differences and improvements were profound. The educational experience herein transcends a “simulation experience” because it also involves lectures, student-student interaction, and interaction with a faculty member - all in a non-simulated environment. The topic is timely. It would be a benefit if this improvement could be tied to a clinical parameter to remove doubt that all that occurred was improving performance in a simulation experience.
Peer reviewer: Javier San Martín, Chief, Gastroenterology and Endoscopy, Sanatorio Cantegril, Av. Roosevelt y P 13, Punta del Este 20100, Uruguay
S- Editor Wu X L- Editor O’Neill M E- Editor Xiong L
| 1. | Hochberger J, Matthes K, Maiss J, Koebnick C, Hahn EG, Cohen J. Training with the compactEASIE biologic endoscopy simulator significantly improves hemostatic technical skill of gastroenterology fellows: a randomized controlled comparison with clinical endoscopy training alone. Gastrointest Endosc. 2005;61:204-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Haycock AV, Youd P, Bassett P, Saunders BP, Tekkis P, Thomas-Gibson S. Simulator training improves practical skills in therapeutic GI endoscopy: results from a randomized, blinded, controlled study. Gastrointest Endosc. 2009;70:835-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Hochberger J, Euler K, Naegel A, Hahn EG, Maiss J. The compact Erlangen Active Simulator for Interventional Endoscopy: a prospective comparison in structured team-training courses on "endoscopic hemostasis" for doctors and nurses to the "Endo-Trainer" model. Scand J Gastroenterol. 2004;39:895-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Matthes K, Cohen J, Kochman ML, Cerulli MA, Vora KC, Hochberger J. Efficacy and costs of a one-day hands-on EASIE endoscopy simulator train-the-trainer workshop. Gastrointest Endosc. 2005;62:921-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Chang WH, Shih SC, Wang HY, Chang CW, Chen CJ, Chen MJ. Acquired hyperplastic gastric polyps after treatment of ulcer. J Formos Med Assoc. 2010;109:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 6. | Han AR, Sung CO, Kim KM, Park CK, Min BH, Lee JH, Kim JY, Chang DK, Kim YH, Rhee PL. The clinicopathological features of gastric hyperplastic polyps with neoplastic transformations: a suggestion of indication for endoscopic polypectomy. Gut Liver. 2009;3:271-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Sung HY, Cheung DY, Cho SH, Kim JI, Park SH, Han JY, Park GS, Kim JK, Chung IS. Polyps in the gastrointestinal tract: discrepancy between endoscopic forceps biopsies and resected specimens. Eur J Gastroenterol Hepatol. 2009;21:190-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Carpenter S, Petersen BT, Chuttani R, Croffie J, DiSario J, Liu J, Mishkin D, Shah R, Somogyi L, Tierney W. Polypectomy devices. Gastrointest Endosc. 2007;65:741-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Hochberger J, Maiss J. Currently available simulators: ex vivo models. Gastrointest Endosc Clin N Am. 2006;16:435-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Morais DJ, Yamanaka A, Zeitune JM, Andreollo NA. Gastric polyps: a retrospective analysis of 26,000 digestive endoscopies. Arq Gastroenterol. 2007;44:14-17. [RCA] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Archimandritis A, Spiliadis C, Tzivras M, Vamvakousis B, Davaris P, Manika Z, Scandalis N. Gastric epithelial polyps: a retrospective endoscopic study of 12974 symptomatic patients. Ital J Gastroenterol. 1996;28:387-390. [PubMed] |
| 12. | Schuetz M, Gockel I, Beardi J, Hakman P, Dunschede F, Moenk S, Heinrichs W, Junginger T. Three different types of surgeon-specific stress reactions identified by laparoscopic simulation in a virtual scenario. Surg Endosc. 2008;22:1263-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Chuttani R, Barkun A, Carpenter S, Chotiprasidhi P, Ginsberg GG, Hussain N, Liu J, Silverman W, Taitelbaum G, Petersen B. Endoscopic clip application devices. Gastrointest Endosc. 2006;63:746-750. [PubMed] |
| 14. | Prabhu A, Smith W, Yurko Y, Acker C, Stefanidis D. Increased stress levels may explain the incomplete transfer of simulator-acquired skill to the operating room. Surgery. 2010;147:640-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Andreatta PB, Hillard M, Krain LP. The impact of stress factors in simulation-based laparoscopic training. Surgery. 2010;147:631-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |