Published online Oct 14, 2011. doi: 10.3748/wjg.v17.i38.4334
Revised: November 23, 2010
Accepted: November 30, 2010
Published online: October 14, 2011
AIM: To investigate the role of 64-slice computed tomography (CT) in portal vein cavernous transformation to determine surgical strategy.
METHODS: The site of lesions and extent of collateral circulation in 12 pediatric cases of cavernous transformation of the portal vein with surgical treatment were analyzed.
RESULTS: Eleven of 12 children had esophageal varices and were treated with lower esophageal and gastric devascularization and splenectomy, and the other case was only treated with splenectomy. There were eight cases with spontaneous spleen/stomach-renal shunt, four with Retzius vein opening, which was reserved during surgery. Three cases of lesions involving the intrahepatic portal vein (PV) were treated with living donor liver transplantation. One patient died from PV thrombosis after liver transplantation, and the rest had no significant complications.
CONCLUSION: The PV, its branches and collateral circulation were clearly seen by 64-slice spiral CT angiography, which helped with preoperative surgical planning.
- Citation: Zhang MM, Pu CL, Li YC, Guo CB. Sixty-four-slice computed tomography in surgical strategy of portal vein cavernous transformation. World J Gastroenterol 2011; 17(38): 4334-4338
- URL: https://www.wjgnet.com/1007-9327/full/v17/i38/4334.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i38.4334
Cavernous transformation of the portal vein (CTPV) is a rare disease in children. The location of the cavernous transformation determines the clinical manifestation of the patients and the treatment procedures[1]. Computed tomography (CT) can be utilized for angiography of CTPV and has distinct advantages in locating the position and assessing the severity of the cavernous transformation[2]. Few people have reported using 64-slice CT for the diagnosis of CTPV or its impact on surgical procedures. The current study retrospectively analyzed the angiographic performance of 64-slice CT in 12 cases and evaluated whether it affects surgical procedures by comparing the corresponding surgical results.
Eighteen pediatric cases of CTPV were admitted to our department between June 1999 and December 2007. Among these 12 patients (nine male and three female) received 64-slice CT and surgical treatment after 2004. The patient ages were between 3 and 8 years, with an average of 5 years and 3 mo. The clinical records of the patients were thoroughly analyzed, and the location of the thrombus in the portal vein (PV), the pathology of the hepatic lesions, surgical procedures, findings during surgery, and the corresponding treatment were recorded. The symptoms of CTPV were reviewed and analyzed along with the surgical results.
All the cases in this group were first diagnosed with CTPV and portal hypertension using color Doppler ultrasound. After 2004, they were all further examined with 64-slice CT. The choice of surgical procedures was determined by the range, degree and location of cavernous transformation in the hepatic hilar area, as well as the condition of thrombus in the vein and establishment of collateral circulation in the surrounding tissue.
Infants with little bleeding and no obvious symptoms were subjected to conservative treatment. The surgical procedures were determined based on the clinical manifestation, the location of the cavernous transformation and the condition of the varices. Surgical vascular disconnection was performed in the gastric fundus and the lower esophagus for the children with symptoms of CTPV with little bleeding (less than twice). No significant damage of hepatic function, cavernous transformation outside the liver, or varices in the lower esophagus and gastric fundus was observed. Surgery should completely disconnect the variceal veins. Splenectomy was only performed in children who showed splenomegaly and hypersplenism, but who did not have gastrointestinal bleeding or varices in the lower esophagus and gastric fundus. Living-donor liver transplantation was performed in children with cavernous transformation in intrahepatic veins, which was accompanied by liver dysfunction. Patients in this group were younger and had smaller vein diameters and thinner venous walls, which led to difficulties in anastomosis and risk of obstruction at the anastomosis, therefore, we did not perform shunt surgery on these patients.
Information on clinical, laboratory and imaging examinations, as well as treatment procedures and prognosis, was recorded for all patients. The treatments and their effectiveness were evaluated for each patient. For those patients treated with surgery, the results were considered good if the clinical symptoms disappeared after surgery. The longest follow-up time was 5 years. The follow-up content included the inquiry of the incidence of hematemesis and melena after surgery, as well as liver function examination and type B ultrasound examination.
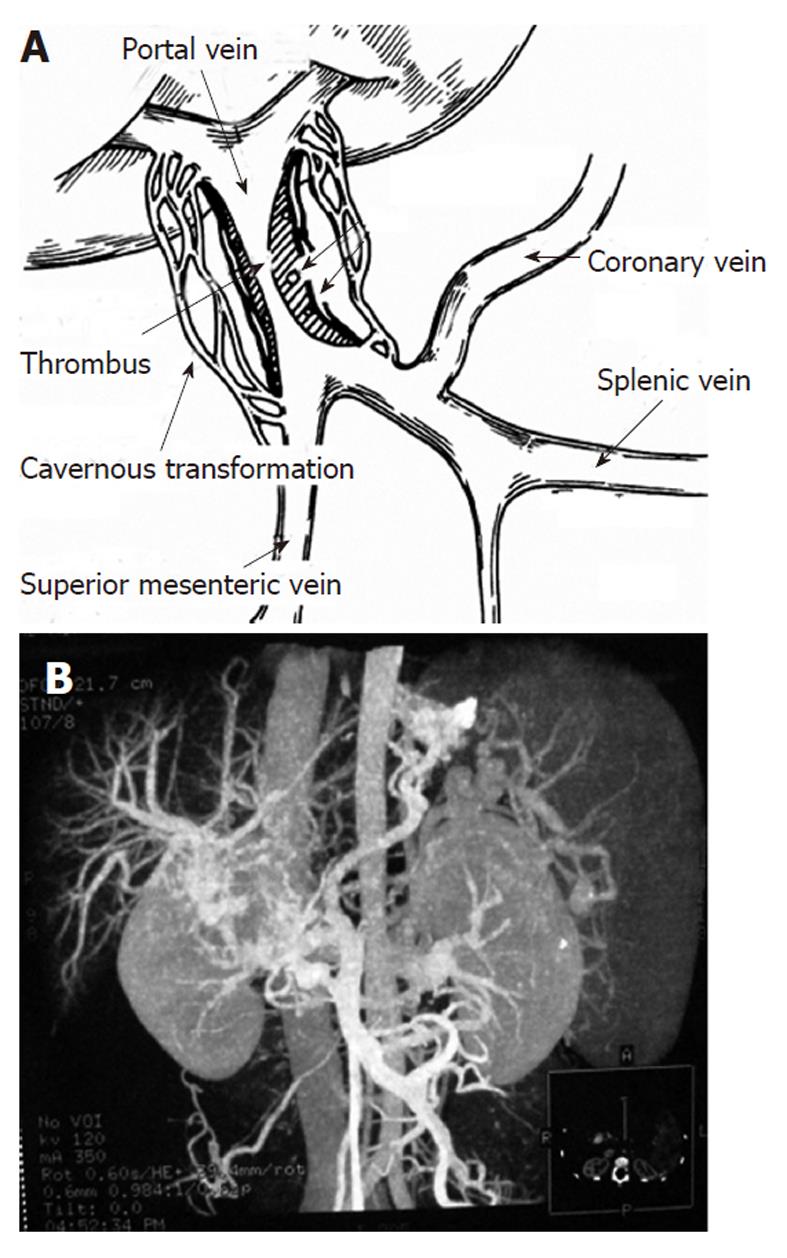
For all 12 cases of CTPV, a large amount of collateral circulation was found around the PV. The normal PV structure disappeared at the hepatic hilar area, and nodular vessels, with anfractuosity, hemangiectasis and different diameters were instead detected on the angiogram and were accompanied by an apparently enhanced venous phase. The patients exhibited typical symptoms of cavernous transformation. Occlusion in the PV trunk was found in nine cases, and complete occlusion was found in three. Four cases had occlusion in the PV trunk, in combination with occlusion of the superior mesenteric vein or proximal splenic vein. Five cases had occlusion of the large part of the superior mesenteric vein and splenic vein (Figure 1). Three cases had liver laceration with obvious narrowing or occlusion, or unclear angiograms in both the left and right branches of the intrahepatic PV. Cavernous transformation in the intrahepatic PV frequently compressed the biliary system and led to occlusion, infection and other complications, resulting in liver dysfunction, which is an indication for liver transplantation.
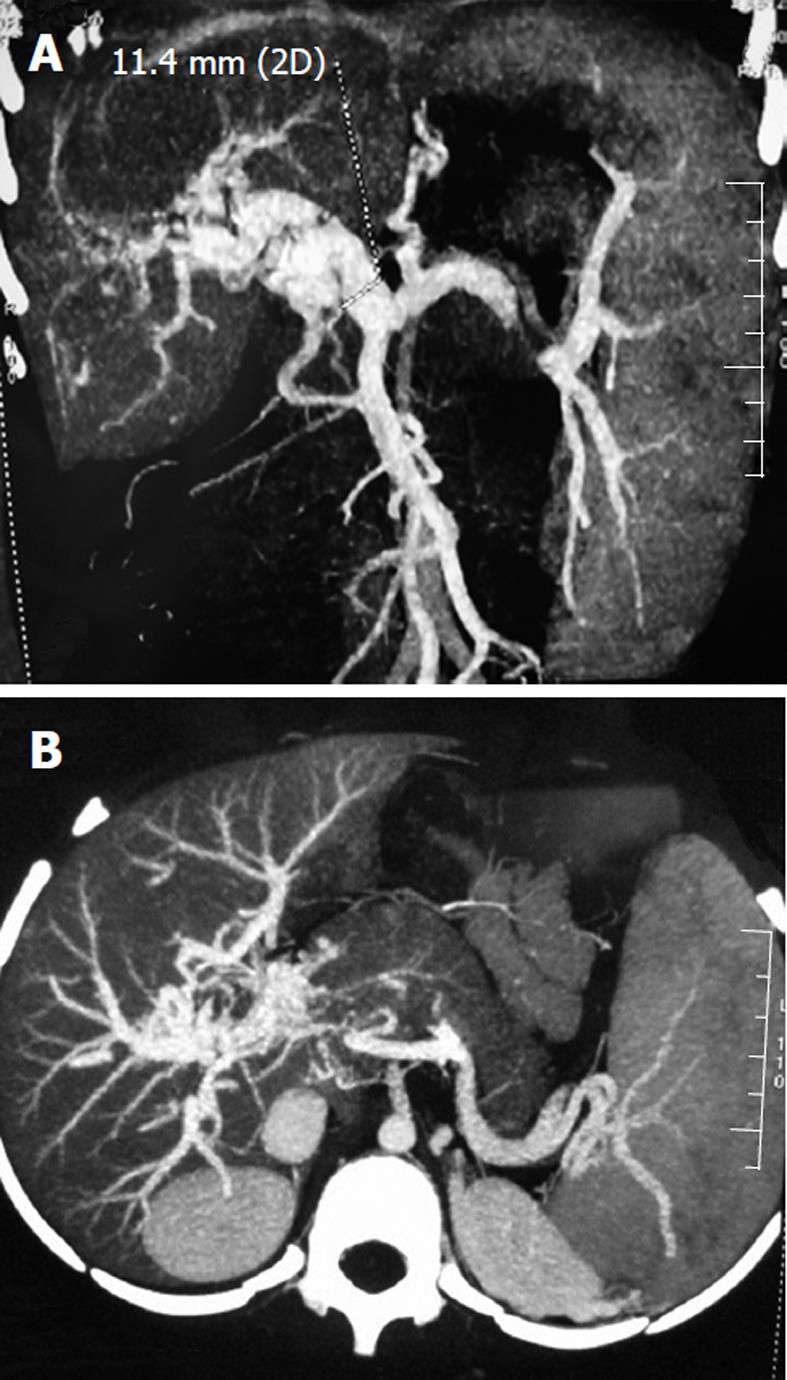
Among the 12 pediatric patients with CTPV, nine had splenomegaly and six had ascites. The major branches of the PV showed different degrees of dilation (Figure 2). Five cases exhibited severe dilation, showing lumpy, tortuous, dilated blood vessels in the lower esophagus and under the gastric fundic mucosa, narrowing of the lumen of the lower esophagus and lumpy protuberance in the gastric cavity (Figure 1). Eight cases had spontaneous splenorenal/gastrorenal shunt, showing highly tortuous, dilated blood vessel structure in disorderly directions. The blood vessels originated from the short gastric vein, posterior gastric vein or blood vessels at the splenic hilum, and connected to the left renal vein through the tortuous, dilated retroperitoneal venous plexus (Figure 3). Seven cases had paraumbilical vein patefaction, showing tortuous dilation with spiral-shaped changes in the ligamentum teres hepatis. The blood vessels were in a radial pattern at the upper and lower end of the structure and connected to chest wall veins as well as the deep and superficial veins of the abdominal wall. Four cases had open retroperitoneal communicating branches (venous plexus of Retzius), showing tortuous disordered retroperitoneal blood vessels, which were dilated in a bundle shape or cirsoid shape or connected to the inferior vena cava in a radial shape. Except for the collateral circulation in the lower esophagus and gastric fundal varices, which can lead to bleeding in the digestive tract, collateral circulation formed at other locations can help to reduce PV pressure and were thus preserved during surgery. When selecting surgical procedures, collateral circulation formation should be considered, which can help estimate prognosis on postoperative recurrence of gastrointestinal bleeding.
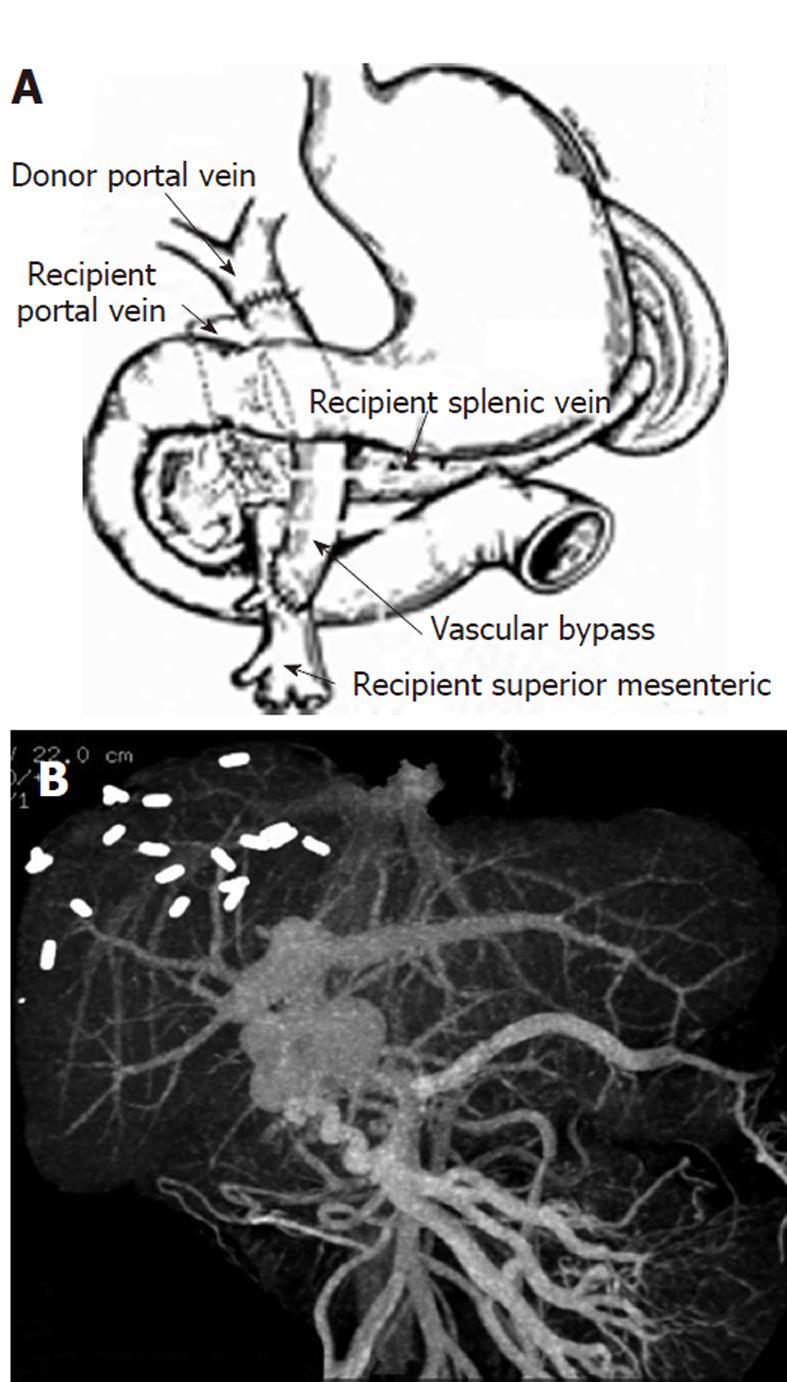
Surgical procedure selection was based on the severity of vascular dilation in the lower esophagus and gastric fundic mucosa, whether CTPV was located inside the liver and the extent of liver dysfunction. Surgical vascular disconnection in the gastric fundus and lower esophagus in combination with splenectomy was performed in 5 cases with severe dilation in the lower esophagus and gastric fundic mucosa. Among them, surgical removal of the thrombus and end-to-end anastomosis of the PV were performed in one case with occlusion of the PV trunk. Splenectomy was performed for four cases without obvious lumpy, tortuous dilation of the veins in the lower esophagus and gastric fundus, but with apparent splenomegaly. Two of these four cases had occlusion of the PV trunk, and surgical removal of the thrombus and end-to-end anastomosis of the PV were performed along with splenectomy. The findings from intraoperative exploration were completely consistent with the results from the preoperative angiography using 64-slice CT. Three children were diagnosed with cavernous transformation involving the inside of the intrahepatic portal vein using 64-slice CT, and all three patients had damaged liver function. Therefore, living-donor liver transplantation was performed on these patients. Due to the lack of collateral vessels, the great saphenous vein of the donor was used as the vascular bypass graft for anastomosis between the PV and the superior mesenteric vein in one case (Figure 4). The findings from the intraoperative exploration were consistent with the preoperative imaging results.
The average follow-up time was 2 years (from 3 mo to 5 years). During the follow-up, no recurrence of severe hematemesis or obvious black tarry feces was observed in the 9 pediatric patients who received gastric fundic and lower esophageal vascular disconnection and splenectomy. Three of the patients had liver transplantation; one of them died of portal thrombosis 5 d after surgery. The other two patients did not experience more hematemesis, melena or lower esophageal stenosis, and their liver function completely recovered. One of the patients was already back in elementary school with good performance, and the other went to kindergarten with normal body development (body weight and height) compared to the average values of the children of the same age. Two wk after surgery, one patient had adhesive ileus, which was cured after another operation. Six months after surgery, barium meal examination showed that esophageal varices disappeared in 10 cases, were relieved in one, and one patient was lost to follow-up.
The degree and size of CTPV have an apparent impact on the difficulty level, operative duration and incidence of postoperative complications. Therefore, preoperative understanding of the condition of the CTPV is very important for the surgical process[3]. Ultrasound is a routine clinical examination for CTPV. However, color Doppler ultrasound cannot provide sufficient information on the formation of collateral circulation. Apart from B-type ultrasound, magnetic resonance angiography and 64-slice CT, portal angiography is the ideal examination method for angiogram. However, the former is limited by breath-holding time and it cannot finish a comprehensive examination for the abdominal wall, paraumbilical area and retroperitoneal varices at one time. Because 64-slice CT can clearly demonstrate the anatomy of the PV system and collateral circulation, sub-millimeter thin-layer volume scan was performed with 64-slice spiral CT for the patients in this study, with 3D reconstitution to display in high resolution the anatomical morphology of the PV system in three dimensions and a clear relationship with the adjacent structures. Sixty-four-slice CT has a positive influence on surgical planning, locating blood vessels and preventing intraoperative injuries. Sixty-four-slice CT can also visualize the veins surrounding and those adjacent to the esophagus. The former are the smaller veins attached to the outer membrane of the esophagus, and the latter are the larger veins that are separated from the outer membrane of the esophagus. Previously, examination of these veins has required left gastric angiography or esophageal ultrasound examination. Collateral vessels in the patients in the present study were mainly located in the lower esophagus and gastric fundus, which was consistent with the clinical symptoms of upper gastrointestinal bleeding such as hematemesis and melena. All five cases were treated with surgical venous disconnection in the gastric fundus and esophagus and did not experience any recurrence during postoperative follow-up. Vascular disconnection was performed for the four cases in this study that did not show obvious gastric fundic and esophageal varices. Only splenectomy was carried out in these patients to reduce PV pressure and relieve reduce esophageal and gastric fundic varices. The findings from intraoperative exploration were completely consistent with the results from the preoperative imaging examination. No gastrointestinal bleeding occurred in these patients for 5 years after surgery.
Angiography of the left gastric vein indicates the existence of coronary venous reflux. Coronary venous reflux is an important pathological symptom of portal hypertension. It is also an indicator of esophageal variceal rupture and bleeding. Measures should be taken to prevent this bleeding[4,5]. In the present study, the patients with the most severe symptoms all had dilated and tortuous left gastric veins in 64-slice CT, showing stiffness and irregularity in the running direction of the blood vessels. In addition, to reduce the pressure of the gastric coronary vein, part of the blood in the PV with hypertension can shunt from the open umbilical vein and splenorenal vein to the superior and inferior vena cava. Upper gastrointestinal bleeding is diagnosed based on analysis of the open extent of RVs using 64-slice spiral CT for PV angiography[6]. In the present study, open RV was found in four cases, and spontaneous portosystemic shunt was found in five, which were all conserved during surgery. None of the patients displayed upper gastrointestinal bleeding after surgery. This is similar to reports from other countries[7]. Cavernous transformation in the intrahepatic PV frequently compresses the biliary system and leads to occlusion, infection and other complications, resulting in damage to liver function, which is an indication for liver transplantation. In the present study, three cases had deformed blood vessels and hemangioma-like symptoms in the intrahepatic portal system, which were accompanied by damaged liver function and hypersplenism. All of these patients were at the late stage of portal hypertension. Studies have shown that intrahepatic CTPV is one of the indications for liver transplantation[8]. Three of our patients received liver transplantation. Due to the difficulties in anastomosis resulting from a large lesioned area, the great saphenous vein of the donor was used as a vascular bypass graft for anastomosis between the PV and superior mesenteric vein in one case. The findings from intraoperative exploration were consistent with the preoperative imaging results. From the follow-up, the symptoms of portal hypertension in the three patients were all remarkably relieved, demonstrating excellent short-term clinical results. However, liver transplantation has not been widely used to treat CTPV. Long-term follow-up is still necessary for the assessment of its long-term therapeutic effects and to compare it with other surgical procedures.
In summary, many changes occur in the portal venous system following CTPV. Sixty-four-slice spiral CT portal angiography and the 3D reconstitution technique can effectively demonstrate the pathological changes in the PV system, clearly showing the major branches of the PV as well as the running direction and distribution of collateral circulation, precisely locating the pathological lesions, demonstrating the space relationship between the lesions and the blood vessels and providing accurate information for clinical assessment and surgery planning. Sixty-four-slice CT is an optimal diagnostic method. However, it requires corresponding equipment and facilities. In addition, its cost is relatively high, which not all young patients can afford.
We wish to express our gratitude to all our transplant coordinators, nursing staff, and administrative personnel, without whom this work would not have been possible. In particular, Lin Mo, Zhi-Mei Ren, Yuan Shi, Lin Bo, Ying-Liang Li, Qi-Lin Li, Yi Tang and Qiao Wang. We would also like to thank our previous and current transplant fellows for their diligent and tireless work: Xiao-Ke Dai, Qiang Xiong, Kai Chen and Xiao-Mei Zhu.
Portal venography by 64-slice computed tomography (CT) can depict the anatomical characteristics of portosystemic collateral vessels in pediatric patients with Cavernous transformation of the portal vein (CTPV). Sixty-four slice CT has been used widely in collateral circulation studies of esophageal and gastric varices. The drainage veins of esophageal varices can be clearly displayed by 64-slice CT.
Diagnosing and treatment of this complicated disease is problematic mostly due to the absence of more accurate data on the position and severity of the disease features in such patients. Recent technical advances offer us increasingly greater imaging clarity of CTPV for its diagnosis. Few people have reported the impact of 64-slice CT on surgical strategy planning. This study focused on the utilization of 64-slice CT to provide referable information for clinical management selection and prognosis evaluation.
Recent reports have highlighted the importance of 64-slice CT in the diagnosis of CTPV or its impact on prognosis evaluation. However, this is the first study to report that 64-slice CT is also valuable in the selection of surgical procedures. This studies suggest that 64-slice CT is a useful method for the assessment of therapeutic effect following treatment of gastric varices. In the majority of cases in the present study, the collateral circulation pattern and the morphological characteristics of CTPV were revealed as a result of the high spatial resolution images of 64-slice CT and the appropriate images post-processing.
Displaying the morphological characteristics of the PV system and collateral circulation, 64-slice CT portal angiography may represent a future strategy for therapeutic management of patients with CTPV. It would seem that 64-slice CT has a valuable role in this situation.
Faster scanning with 64-slice CT, combined with rapid intravenous administration of contrast material, allows visualization of the more distal branches of the portosystemic vessels. CTPV is a relatively rare condition resulting from extrahepatic PV obstruction with recanalization or collateral vein formation to bypass the obstruction. Paraesophageal varices are the varices that exist outside the esophagus. The subphrenic vein is the bilateral vessel that ends up at the inferior vena cava at the diaphragm level.
The authors demonstrated that 64-slice CT portal angiography could provide accurate information for clinical assessment, especially surgical planning. This is a good paper with excellent images. The results are interesting and may represent the optimal selection of clinical therapy and evaluation of prognosis.
Peer reviewer: Dr. Furqan Haider Sherazi, King Edward Medical University, House 975, Street 48, Sector G/11-2, Islamabad 44000, Pakistan
S- Editor Wu X L- Editor Kerr C E- Editor Xiong L
| 1. |
Schettino GC, Fagundes ED, Roquete ML, Ferreira AR, Penna FJ. Portal vein thrombosis in children and adolescents.
J Pediatr |
| 2. | Zhao LQ, He W, Chen G. Characteristics of paraesophageal varices: a study with 64-row multidetector computed tomography portal venography. World J Gastroenterol. 2008;14:5331-5335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Vasilescu C, Stanciulea O, Popa M, Colita A, Arion C. Subtotal laparoscopic splenectomy and esophagogastric devascularization for the thrombocytopenia because of portal cavernoma--case report. J Pediatr Surg. 2008;43:1373-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Ateş O, Hakgüder G, Olguner M, Seçil M, Karaca I, Akgür FM. Mesenterico left portal bypass for variceal bleeding owing to extrahepatic portal hypertension caused by portal vein thrombosis. J Pediatr Surg. 2006;41:1259-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Fagundes ED, Ferreira AR, Roquete ML, Penna FJ, Goulart EM, Figueiredo Filho PP, Bittencourt PF, Carvalho SD, Albuquerque W. Clinical and laboratory predictors of esophageal varices in children and adolescents with portal hypertension syndrome. J Pediatr Gastroenterol Nutr. 2008;46:178-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Cakmak O, Parildar M, Oran I, Sever A, Memis A. Sinistral portal hypertension; imaging findings and endovascular therapy. Abdom Imaging. 2005;30:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Ertuğrul I, Köklü S, Başar O, Yüksel O, Uçar E, Coban S, Ibiş M, Arhan M, Odemiş B, Saşmaz N. Thrombosis of the portal venous system: a prospective study. J Clin Gastroenterol. 2008;42:835-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Zhang M, Guo C, Pu C, Ren Z, Li Y, Kang Q, Jin X, Yan L. Adult to pediatric living donor liver transplantation for portal cavernoma. Hepatol Res. 2009;39:888-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |