Published online Oct 7, 2011. doi: 10.3748/wjg.v17.i37.4199
Revised: March 4, 2011
Accepted: March 11, 2011
Published online: October 7, 2011
AIM: To prospectively assess the efficacy and safety of stapled trans-anal rectal resection (STARR) compared to standard conservative treatment, and whether preoperative symptoms and findings at defecography and anorectal manometry can predict the outcome of STARR.
METHODS: Thirty patients (Female, 28; age: 51 ± 9 years) with rectocele or rectal intussusception, a defecation disorder, and functional constipation were submitted for STARR. Thirty comparable patients (Female, 30; age 53 ± 13 years), who presented with symptoms of rectocele or rectal intussusception and were treated with macrogol, were assessed. Patients were interviewed with a standardized questionnaire at study enrollment and 38 ± 18 mo after the STARR procedure or during macrogol treatment. A responder was defined as an absence of the Rome III diagnostic criteria for functional constipation. Defecography and rectoanal manometry were performed before and after the STARR procedure in 16 and 12 patients, respectively.
RESULTS: After STARR, 53% of patients were responders; during conservative treatment, 75% were responders. After STARR, 30% of the patients reported the use of laxatives, 17% had intermittent anal pain, 13% had anal leakage, 13% required digital facilitation, 6% experienced defecatory urgency, 6% experienced fecal incontinence, and 6% required re-intervention. During macrogol therapy, 23% of the patients complained of abdominal bloating and 13% of borborygmi, and 3% required digital facilitation.No preoperative symptom, defecographic, or manometric finding predicted the outcome of STARR. Post-operative defecography showed a statistically significant reduction (P < 0.05) of the rectal diameter and rectocele. The post-operative anorectal manometry showed that anal pressure and rectal sensitivity were not significantly modified, and that rectal compliance was reduced (P = 0.01).
CONCLUSION: STARR is not better and is less safe than macrogol in the treatment of defecation disorders. It could be considered as an alternative therapy in patients unresponsive to macrogol.
- Citation: Biviano I, Badiali D, Candeloro L, Habib FI, Mongardini M, Caviglia A, Anzini F, Corazziari ES. Comparative outcome of stapled trans-anal rectal resection and macrogol in the treatment of defecation disorders. World J Gastroenterol 2011; 17(37): 4199-4205
- URL: https://www.wjgnet.com/1007-9327/full/v17/i37/4199.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i37.4199
Functional constipation affects up to 20% of the population, and about 50% of constipated patients consulting a tertiary referral practice complain of difficult evacuation[1,2], such as straining at stools, sensation of incomplete evacuation, or ano-rectal obstruction[3,4], and may require digitation to facilitate defecation. Rectocele and intra-rectal intussusception are frequent findings in patients with functional constipation, and are thought to play a relevant role in defecatory alterations[5]. Surgical repair of the recto pelvic anatomy has been proposed to improve defecation. Recently, an international consensus conference[6] proposed that “the combination of the characteristic history of disordered defecation and the anatomical finding of one or more of the following: rectocele, rectal intussusception, perineal descent, mucosal prolapse may lead a surgeon to offer the stapled trans-anal rectal resection (STARR)[7-9] procedure, provided that the individual has failed medical management”.
The STARR procedure consists of the trans-anal resection of the distal rectum using a double-stapler. Semicircular purse-string sutures are applied on the prolapsed rectal wall, including mucosa, submucosa, and rectal muscle wall, at 2 cm above the hemorrhoidal apex so as to include the rectocele and the internal rectal prolapse.
So far both favorable[10] and unfavorable results[11] of the procedure have been reported. However, no study has assessed the efficacy and safety of the STARR procedure in comparison with evidence based conservative treatment for the management of functional constipation and defecatory disorders.
The main aim of the present study was to assess the efficacy and safety of the STARR procedure in the treatment of patients with chronic constipation complaining of defecatory disorders and with defecographic evidence of rectocele and intra-rectal intussusception. An additional aim of the study was to assess whether preoperative symptoms, and manometric or defecographic findings, can predict the long-term outcome of the STARR procedure.
Consecutive outpatients referred for refractory chronic constipation in a 48-mo period by two surgical and one gastroenterological centers, underwent a diagnostic work up, including anorectal manometry and defecography. Patients with refractory chronic constipation were identified as those who did not respond to the usual conservative treatment and still complained of difficult and/or incomplete evacuation, despite the use of high daily doses of contact laxatives, enemas, or digital evacuation. Inclusion criteria were the following: (1) diagnosis of functional constipation according to the Rome III criteria during the preceding three months, with onset at least 6 mo prior to the diagnosis (in the absence of laxatives and/or enemas) of two or more of the following complaints: less than three bowel movements (BM) per week; straining at defecation and/or sense of incomplete evacuation and/or hard stools and/or sensation of anorectal obstruction/blockage and/or manual maneuvers to facilitate defecation on at least 25% of occasions; (2) difficult evacuation defined as either straining or sensation of obstruction/blockage; (3) age between 18 and 75 years; (4) no previous anorectal surgery; (5) no abnormality at barium enema or colonoscopy; (6) normal laboratory routine tests; (7) evidence of rectocele and/or intra-rectal intussusceptions at defecography; (8) no previous treatment with oral macrogol solution; (9) no pregnancy and efficacious birth control methods; (10) absence of systemic disease; and (11) absence of therapy affecting intestinal function. Chronic anxiolytic and antidepressive treatment were admitted provided the dosage was not modified during the study period. Exclusion criteria were the following: (1) no diagnosis of functional constipation; (2) previous anorectal surgery; (3) age less than 18 and above 75 years; (4) absence of rectocele and intra-rectal intussusception at defecography; (5) abnormality at barium enema or colonoscopy; (6) abnormal laboratory tests; (7) previous treatment with oral macrogol solution; (8) pregnancy and no use of efficacious birth control methods; (9) presence of systemic disease; and (10) presence of therapy affecting intestinal function.
At referral, all patients were interviewed with a standardized questionnaire, and had a physical examination. The questionnaire inquired about bowel habit: frequency of defecation, straining, stool consistency, sensation of incomplete evacuation, sensation of anal obstruction/blockage, digital facilitation to evacuate, anal pain, and anal incontinence.
On a different day, a colonoscopy was performed in patients over 50 years of age who had not had a colonoscopy or a barium enema in the previous five years. Patients were then submitted on different days for defecography and anorectal manometry.
Thirty consecutive patients, reporting an unsatisfactory response to the conservative treatment of constipation with different types of laxatives, were enrolled by the two surgical units; sixteen by AC and fourteen by MM, and were then submitted to the STARR procedure according to a standardized and previously published method[10]. In the same time period, thirty additional and consecutive patients referred to the gastrointestinal center were assigned conservative treatment with oral macrogol solution. These patients were instructed to consume 1 sachet (8.75 g) of macrogol dissolved in 125 mL of water bid., with the option to either reduce the dose to od or increase it up to qid. to obtain evacuation of soft stools.
After the STARR procedure patients, were subjected to a second rectoanal manometry and defecography.
All patients were re-assessed at least 24 mo after the surgical procedure or the medical prescription.
At follow-up, the patients were interviewed, either face to face or by telephone, with the same standardized questionnaire used at referral, which included additional items related to treatment satisfaction and adverse events. Patients were invited to declare whether they were “totally dissatisfied with the treatment”, or “partially satisfied with the treatment” when at least one symptom of constipation and/or side effects were present, or “fully satisfied with the treatment”.
The degree of constipation was evaluated with the Wexner score[12]. The study was approved by the local ethics committee.
A cleansing non-medicated water enema was performed the night before the radiological examination. About 200 milliliters of barium paste were injected into the rectum, through an anal catheter. Continuous injection of the contrast during slow withdrawal of the catheter rendered the anal canal opaque. Patients were then seated on a radiolucent commode. The entire evacuation sequence was recorded on videotape (JVC SR-VS30E Mini DV/S-VHS). Latero-lateral radiograms were taken at rest and during mid-evacuation, as previously reported[13].
After a cleansing enema, rectal sensitivity and anorectal manometry were evaluated using a multilumen polyethylene catheter with four open tips disposed radially, and 0.5 mm apart longitudinally, continuously perfused (0.5 mL/min) with bubble-free distilled water by means of a pneumo-hydraulic infusion system (Arndorfer, Milwaukee, Wisconsin, United States), and connected to Beckman 611 external transducers. A fifth lumen ended in a latex balloon attached to the tip of the catheter. Intraluminal pressure variations were transmitted from the transducers to a polygraph (R612 Dynograph Recorder SensorMedics Italia srl) for recording.
The resting pressure profile of the anal canal was recorded with a pull-through technique. Thereafter, the manometric probe was positioned in the anal canal with the recording holes and the deflated balloon in the rectum. The patient was then asked to squeeze and to strain. Lastly the intra-rectal balloon was intermittently inflated with progressive volumes of air to elicit the recto-anal inhibitory reflex (RAIR). To assess the threshold of rectal sensitivity, patients were instructed to refer the first sensation of rectal distension and/or the urge to defecate during the incremental intrarectal balloon inflations[14].
The primary endpoint of the study was relief of constipation, i.e., when the patient no longer met the Rome III criteria for functional constipation and was considered a responder.
Secondary endpoints were: the assessment of (1) the constipation improvement by means of the Wexner score; and (2) symptoms, defecographic, and manometric findings in predicting the outcome of the STARR procedure.
Analysis of defecographic data: Frame by frame analysis of the sequences recorded on the videotape assessed timing and dynamics of evacuation, rectal emptying, and presence of anatomical alterations of the rectal wall. Anorectal angle (ARA) widening, anal canal opening, pelvic floor (PF) location at rest, and its mobility were assessed on the latero-lateral radiograms. Rectocele was defined as an outpouching of the anterior rectal wall into or across the rectovaginal septum, rectal intussusception was defined as an enfolding of the rectal wall, which may (intra-anal) or may not (intra-rectal) protrude through the anal canal. Pelvic floor dyssynergia was defined as: anorectal angle (ARA) widening < 10° and/or the opening of anal canal < 10 mm, and/or anal canal opening > 10 mm in more than 30 s or interrupted by repetitive squeezing contractions. Contrast rectal residue was assessed by a semi-quantitative evaluation of the rectal residue as small (< 40%), intermediate (40%-70%), and abundant (> 70%).
Analysis of manometric data: Maximal resting and squeezing pressures were identified as the maximal steady value observed for 20 s in basal condition and during maximal voluntary anal contraction. The thresholds of RAIR and rectal sensitivity were defined as the smallest inflated volumes of the intrarectal balloon inducing, respectively, a fall in anal pressure of at least 12 mmHg[14], and the urge to evacuate. Rectal compliance was calculated as the ratio between intrarectal balloon volume inflated with 100 mL of air and intrarectal pressure. During straining, a decrease of anal pressure of more than 20% was considered a normal relaxing pattern; the absence of a decrease of less than 20%, or the increase, of the anal pressure were considered as dyssynergic patterns.
Results are reported as means and standard deviation (mean ± SD). Descriptive statistical techniques were used to compare the two groups of patients. A χ2 test and Fisher’s exact test were used to compare the frequency of symptoms in the different study groups; Student’s t test was used to compare the two groups for continuous variables.
Sixty patients were enrolled: 30 patients underwent STARR, and 30 patients were treated with macrogol. The two study groups were comparable for gender, age, and symptom presentation (Table 1).
| STARR n = 30 (F28) | Macrogol n = 30 (F30) | P value | |
| Mean age (yr) | 51 ± 9 | 53 ± 13 | |
| Duration of | 24 (80) | 26 (87) | 0.7 |
| constipation > 10 yr | |||
| Straining | 28 (93) | 29 (97) | 1 |
| Hard stools | 27 (90) | 29 (97) | 0.6 |
| Incomplete evacuation | 27 (90) | 27 (90) | 0.7 |
| Anal blockage | 27 (90) | 27 (90) | 0.7 |
| Digital facilitation | 11 (37) | 8 (27) | 0.6 |
| < 3 BM/wk | 23 (77) | 26 (87) | 0.5 |
| Laxatives | 27 (90) | 30 (100) | 0.2 |
| Rectal bleeding | 13 (43) | 7 (23) | 0.2 |
| Rectocele > 3 cm | 23 (77) | 15 (50) | 0.06 |
| Rectal intussusception | 15 (50) | 20 (67) | 0.3 |
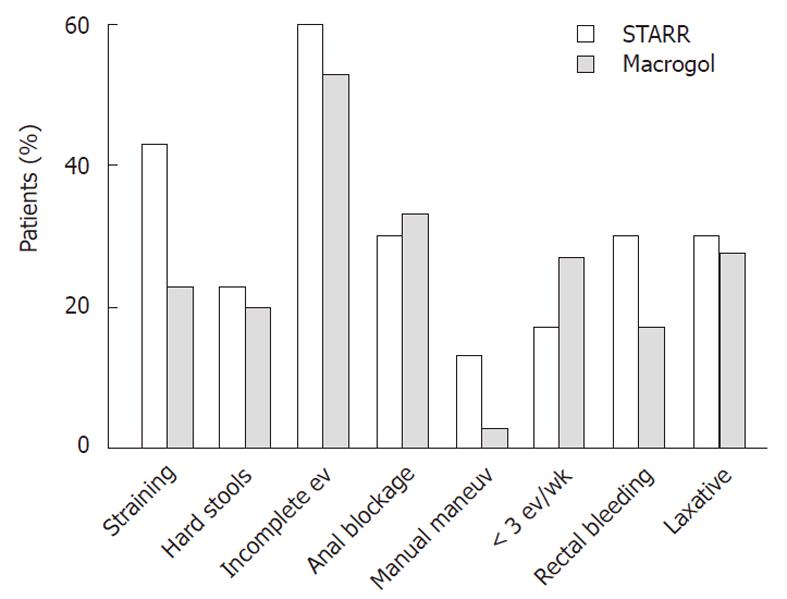
Macrogol group: The follow up period was 44 ± 11 mo. Twenty-two (75%) patients were classified as responders; constipation by the Wexner score decreased significantly (13.9 ± 1.5 vs 5.9 ± 4.5; P < 0.001). Seven patients (27%) had discontinued macrogol and were using either contact or other osmotic laxatives; two patients still required digital facilitation (Figure 1).
STARR group: The follow up period was 38 ± 18 mo. Sixteen (53%) patients were classified as responders. No outcome difference was observed between patients of the two surgical units (responders: 8/16 vs 6/14). Constipation by the Wexner score decreased significantly (13.4 ± 3.2 vs 7.32 ± 5.76; P < 0.001); nine (30%) patients still used laxatives and four (13%) digital facilitation (Figure 1). After the surgical procedure, 14 patients reported at least one side effect and two (6%) required re-intervention; the first for relapse of rectocele and the second for fecal incontinence. The presenting symptoms at referral did not differ between responders and non-responders (Table 2).
| Responders | Non-responders | P value | |
| Straining | 16 (100) | 12 (86) | 0.4 |
| Hard stools | 14 (87) | 13 (93) | 0.9 |
| Incomplete evacuation | 16 (100) | 11(78) | 0.2 |
| Anal blockage | 15 (94) | 12 (86) | 0.9 |
| Digital facilitation | 4 (25) | 7 (50) | 0.3 |
| < 3 BM/wk | 13 (81) | 10 (71) | 0.8 |
| Laxatives | 14 (87) | 13 (93) | 0.9 |
Comparison between the study groups: The two groups did not differ statistically for response to the treatment according to the Rome criteria for functional constipation, for improvement of constipation evaluated by means of the Wexner score, and for degree of satisfaction (Table 3). Bowel symptoms at follow-up were similar in the two study groups (Figure 1).
| Macrogol | STARR | P value | |
| Responders | 22 (73) | 16 (53) | 0.2 |
| Satisfaction | 0.4 | ||
| Total | 18 (60) | 16 (53) | |
| Partial | 5 (17) | 9 (30) | |
| Not satisfied | 7 (23) | 5 (17) | |
| Δ Wexner score, mean ± SD | 8 ± 5 | 6 ± 5.2 | 0.1 |
Adverse events in the STARR procedure group, at the end of follow up, were: staining/leakage (13%), fecal incontinence (6%), urgency (6%), intermittent anal pain (17%), and re-intervention (6%). Adverse effects in the macrogol therapy group were abdominal bloating (23%), and borborygmi (13%).
Defecography was performed at referral and at 7 ± 4 mo after STARR in 16 patients. In comparison to the pre-surgical condition, defecographic variables did not vary after surgery, except for a significant reduction in rectal diameter (7.5 ± 1.2 cm vs 5.6 ± 1.2 cm; P < 0.001), and size of rectocele (3.9 ± 1.3 cm vs 1.4 ± 1.5 cm; P < 0.001). The size of intussusceptions was reduced, but the variation was not statistically significant (3.2 ± 1.7 cm vs 2.4 ± 1.3 cm; ns).
Responders and non-responders did not statistically differ for any defecographic variable assessed before surgery (Table 3). Before the operation, the mean ARA variation during evacuation was not statistically different between non-responders and responders (Table 4). After the operation, it was significantly less in the non-responders compared to the responders (28 ± 16 vs 8 ± 20 degrees; P < 0.05).
| Variables | Before | After | ||
| Non-responders | Responders | Non-responders | Responders | |
| Rectal diameter (cm) | 7.7 ± 1.4 | 7.3 ± 1 | 5.5 ± 0.9 | 5.8 ± 1.5 |
| ∆ ARA evacuation (°) | 16 ± 8 | 25 ± 18 | 8.1 ± 20.3 | 28 ± 16.2a |
| PF at rest (cm) | 5.1 ± 1.5 | 4.8 ± 1.3 | 4.3 ± 1.5 | 4.6 ± 1 |
| PF during sqeezing (cm) | 1.4 ± 0.7 | 1.3 ± 0.9 | 1.8 ± 0.9 | 1.2 ± 0.8 |
| ∆ PF evacuation (cm) | 3.1 ± 1.6 | 3 ± 1.3 | 3.6 ± 1.1 | 3.1 ± 1.5 |
| Rectocele (cm) | 3.8 ± 1.8 | 4.1 ± 0.6 | 1.1 ± 1.6 | 1.7 ± 1.5 |
| Anal diameter (cm) | 1.4 ± 0.6 | 1.4 ± 0.8 | 1.3 ± 0.8 | 1.1 ± 0.4 |
Before STARR, defecographic evidence of pelvic floor dyssynergia was detected in three patients; equally represented in responders (one patient) and non- responders (two patients). After STARR, defecographic evidence of pelvic floor dyssynergia was detected in three patients; equally represented in responders (one patient) and non responders (two patients).
Ano-rectal manometry was performed at referral and 24 ± 4 mo after STARR in 12 patients. After STARR, rectal compliance was significantly reduced (5.4 ± 1.9 vs 3.7 ± 1.2 mL/mmHg; P = 0.01), all other manometric variables did not vary. Responders and non-responders did not differ for any manometric findings before and after the procedure.
Before STARR, manometric evidence of pelvic floor dyssynergia was detected in four patients, equally represented in responders (two patients) and non-responders (two patients). After STARR, manometric evidence of pelvic floor dyssynergia was detected in seven patients, equally represented in responders (four patients) and non-responders (three patients).
No previous study has compared the STARR procedure with conservative pharmacological therapy. This study evaluated, over a long time period, the outcome of STARR treatment for constipation, defined with standardized and validated criteria. The surgical procedure was performed following the standardized and previously published procedure[9] by two experienced coloproctology units that obtained comparable postsurgical outcomes. The patients submitted to the STARR procedure reported an unsatisfactory response to a usual, but not standardized, laxative treatment.
Previous studies have reported the postsurgical outcomes of the STARR procedure or of other modified techniques, but no study has compared the efficacy and safety of STARR procedure versus the standardized conservative treatment.
In the present investigation, we compared the outcome of STARR procedure with the gold standard treatment of constipation based on macrogol in a prospective, parallel group, longitudinal study. This therapy for functional constipation is supported by level 1 evidence and grade A recommendation[15]. This is a high molecular weight (3350 or 4000) non-absorbable, non-metabolized soluble polyethylene, which forms hydrogen bonds with water in the gut; it is used with orthograde whole-gut irrigation in preparing for colon investigation, and in small-volume daily doses (125-250 mL) to treat functional constipation. Macrogol therapy is reported to be effective in about 80% of constipated patients, is well tolerated, and devoid of serious side effects, even in long term treatment[16,17].
All the patients of these study groups met the Rome III criteria for functional constipation and had defecographic evidence of rectocele and or intrarectal intussusception. Patients were evaluated with a standardized questionnaire before and after treatment, with a mean follow-up of 38 mo, which is, to our knowledge, one of the longest reporting STARR outcome[18-31]. Some long-term studies reported sustained improvement of defecation score, but provided conflicting results about side effects, relapse, and complications[32-34].
The present study demonstrated that the surgical tre-atment was less, but not statistically so, efficacious than the conservative one, as indicated by the finding that 75% of the macrogol group and 53% of the STARR group did not present any Rome criteria for functional constipation. In addition, after the STARR operation, about 30% of the patients still consumed laxatives and 13% were using digital manipulation to evacuate.
Of note is that during a mean follow up of three years after the STARR operation, intermittent bleeding was present in 24% of the patients, anal pain in 17%, and anal incontinence of variable severity in 25%. Furthermore, two patients required a re-intervention. The observed prevalence of these complications in the present study is similar to that reported in other studies[11,25]. The European STARR register reports perioperative and postoperative complications in about 36% of the patients, and defecatory urgency in 20% of the cases at one year of follow-up[35]. In our study, a few adverse events of STARR persisted in this long-term follow up with possible detrimental effects on daily living.
The degree of satisfaction expressed by patients parallels that of the improvement of constipation achieved by the two treatments. Only 15% of the patients were not satisfied with the STARR procedure, despite the presence of some persistent symptoms or the previously mentioned complications.
Defecography was performed in all patients before and, in a subgroup of them, after the STARR procedure. No defecographic finding before surgery predicted the outcome of the STARR operation. As expected, after surgery there was a significant reduction of rectal diameter and the size of the rectocele, but such variations were no different between responders and non-responders.
After STARR, the mean value of ARA variation during evacuation in non-responders was significantly reduced in comparison to the preoperative value, and was significantly less than in responders. This finding indicates that the STARR procedure may affect the relaxation pattern of the puborectalis muscle during evacuation. It remains to be established how the STARR procedure induces this effect on the puborectalis. It is reasonable to assume that a reduced ARA variation during defecation may negatively affect evacuation, nonetheless it is not possible to conclude from this study whether it has any role in the poor clinical outcome of non-responders.
According to the STARR consensus conference, the inclusion criteria for surgical treatment are based on clinical presentation of difficult evacuation and/or straining, in the presence of rectocele and/or intussusception. In this study, the inclusion criteria were based on the consensus conference recommendations; however, no presenting symptom was predictive of the outcome of STARR, nor of the procedure adverse events.
In addition, anorectal manometry was not useful in predicting the outcome of STARR. A previous study reported that altered compliance could be predictive of positive outcome[10]. This observation was not confirmed by the present study; the discordance could be due to the small sample in this study or to the different method used to evaluate compliance. In the previous study, compliance was assessed by the ratio between volume and pressure at the threshold of rectal sensitivity, whereas in this study, it was calculated using the fixed volume of 100 mL of air, to avoid possible subjective differences of rectal sensitivity. However, a study designed to investigate whether rectal compliance is altered in females with obstructed defecation, showed that the compliance of the rectal wall is normal[36].
Several structural and functional alterations of the rectum and/or pelvic floor are considered to markedly impair the act of defecation; however, the findings of this study indicate that stool consistency is a major factor in chronic constipation. Indeed, the favorable response to macrogol treatment in the non-surgical group indicated that reducing stool consistency, reported at referral to be hard by more than 90% of the patients, effects resolution of constipation, despite the persistence of the structural and functional alterations. Thus, it seems reasonable to consider a surgical procedure only after the failure of a standardized macrogol treatment.
In conclusion, the results of this prospective study suggest that STARR is not better and is less safe than conservative therapy in the treatment of defecation disorders in functional constipation patients. Preoperatively, no presenting symptom, or defecographic, and manometric variables were useful to indicate STARR and predict its results. Postoperatively, a reduced widening of ARA during evacuation was associated with an unfavorable outcome of the procedure. The STARR procedure could be considered as an alternative treatment in patients with constipation and defecatory disorders who are unresponsive to conservative macrogol treatment.
Constipation is a common problem. It is not clear whether a defecation disorder commonly known as obstructed defecation syndrome (ODS) is due to anatomical abnormalities. However, some surgeons propose a new type of surgery [stapled trans-anal rectal resection (STARR)], which, by correcting the anatomical changes, should solve the constipation. Surgery should be considered for those patients who do not benefit from conservative treatment. The gold standard pharmacological treatment of constipation is based on macrogol, which is also effective in patients with altered defecation.
Ideally, a randomized double blind clinical trial would have more properly assessed the efficacy and safety of the STARR procedure, but the comparison between a non-invasive treatment and an invasive procedure is an objective obstacle to plan a proper protocol, and such studies have not been previously performed. No previous study has so far compared the STARR procedure with conservative pharmacological therapy.
This study evaluated, over a long time period, the outcome of STARR treatment for constipation in comparison with macrogol therapy. The study has shown that STARR is not better, and is less safe, than macrogol therapy. In addition, no preoperative findings could predict the outcome of surgery.
The authors believe that macrogol should be used before considering surgery in cases of lack of response to conservative treatment
Rectocele is a protrusion of part of the rectum into the vagina. Rectal intussusception is a protrusion of the rectal mucous membrane into the lower rectum.
The manuscripts reports the comparative analysis of two strategies in managing functional constipation. The authors have compared outcomes of patients that underwent treatment with a conservative regimen that consisted of macrogol and patients that underwent the STARR procedure. This is a well done study; despite not being randomized it provides useful information and should be published.
Peer reviewer: Imran Hassan, MD, Assistant Professor, Department of Surgery, SIU School of Medicine, 701 North Rutledge, PO Box 19638, Springfield, IL 62794, United States
S- Editor Tian L L- Editor Stewart GJ E- Editor Zhang DN
| 1. | Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of constipation in a tertiary referral gastroenterology practice. Am J Gastroenterol. 1995;90:1471-1475. [PubMed] |
| 2. | Rao SS, Patel RS. How useful are manometric tests of anorectal function in the management of defecation disorders? Am J Gastroenterol. 1997;92:469-475. [PubMed] |
| 3. | Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349:1360-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 515] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 4. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3413] [Cited by in RCA: 3383] [Article Influence: 178.1] [Reference Citation Analysis (1)] |
| 5. | Van Laarhoven CJ, Kamm MA, Bartram CI, Halligan S, Hawley PR, Phillips RK. Relationship between anatomic and symptomatic long-term results after rectocele repair for impaired defecation. Dis Colon Rectum. 1999;42:204-210; discussion 210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Corman ML, Carriero A, Hager T, Herold A, Jayne DG, Lehur PA, Lomanto D, Longo A, Mellgren AF, Nicholls J. Consensus conference on the stapled transanal rectal resection (STARR) for disordered defaecation. Colorectal Dis. 2006;8:98-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Boccasanta P, Venturi M, Stuto A, Bottini C, Caviglia A, Carriero A, Mascagni D, Mauri R, Sofo L, Landolfi V. Stapled transanal rectal resection for outlet obstruction: a prospective, multicenter trial. Dis Colon Rectum. 2004;47:1285-1296; discussion 1285-1296;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 175] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Jayne DG, Finan PJ. Stapled transanal rectal resection for obstructed defaecation and evidence-based practice. Br J Surg. 2005;92:793-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Ommer A, Albrecht K, Wenger F, Walz MK. Stapled transanal rectal resection (STARR): a new option in the treatment of obstructive defecation syndrome. Langenbecks Arch Surg. 2006;391:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Boccasanta P, Venturi M, Salamina G, Cesana BM, Bernasconi F, Roviaro G. New trends in the surgical treatment of outlet obstruction: clinical and functional results of two novel transanal stapled techniques from a randomised controlled trial. Int J Colorectal Dis. 2004;19:359-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Gagliardi G, Pescatori M, Altomare DF, Binda GA, Bottini C, Dodi G, Filingeri V, Milito G, Rinaldi M, Romano G. Results, outcome predictors, and complications after stapled transanal rectal resection for obstructed defecation. Dis Colon Rectum. 2008;51:186-195; discussion 195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 818] [Cited by in RCA: 851] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 13. | Habib FI, Corazziari E, Viscardi A, Badiali D, Torsoli A. Role of body position, gender, and age on pelvic floor location and mobility. Dig Dis Sci. 1992;37:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | De Medici A, Badiali D, Corazziari E, Bausano G, Anzini F. Rectal sensitivity in chronic constipation. Dig Dis Sci. 1989;34:747-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100 Suppl 1:S1-S4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 149] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 16. | Ramkumar D, Rao SS. Efficacy and safety of traditional medical therapies for chronic constipation: systematic review. Am J Gastroenterol. 2005;100:936-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 260] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 17. | Corazziari E, Badiali D, Bazzocchi G, Bassotti G, Roselli P, Mastropaolo G, Lucà MG, Galeazzi R, Peruzzi E. Long term efficacy, safety, and tolerabilitity of low daily doses of isosmotic polyethylene glycol electrolyte balanced solution (PMF-100) in the treatment of functional chronic constipation. Gut. 2000;46:522-526. [PubMed] |
| 18. | Arroyo A, Pérez-Vicente F, Serrano P, Sánchez A, Miranda E, Navarro JM, Candela F, Calpena R. Evaluation of the stapled transanal rectal resection technique with two staplers in the treatment of obstructive defecation syndrome. J Am Coll Surg. 2007;204:56-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Boccasanta P, Venturi M, Calabro G, Maciocco M, Roviaro GC. Stapled transanal rectal resection in solitary rectal ulcer associated with prolapse of the rectum: a prospective study. Dis Colon Rectum. 2008;51:348-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Pechlivanides G, Tsiaoussis J, Athanasakis E, Zervakis N, Gouvas N, Zacharioudakis G, Xynos E. Stapled transanal rectal resection (STARR) to reverse the anatomic disorders of pelvic floor dyssynergia. World J Surg. 2007;31:1329-1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Boccasanta P, Venturi M, Roviaro G. Stapled transanal rectal resection versus stapled anopexy in the cure of hemorrhoids associated with rectal prolapse. A randomized controlled trial. Int J Colorectal Dis. 2007;22:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Ellis CN. Stapled transanal rectal resection (STARR) for rectocele. J Gastrointest Surg. 2007;11:153-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Dindo D, Weishaupt D, Lehmann K, Hetzer FH, Clavien PA, Hahnloser D. Clinical and morphologic correlation after stapled transanal rectal resection for obstructed defecation syndrome. Dis Colon Rectum. 2008;51:1768-1774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Pescatori M, Zbar AP. Reinterventions after complicated or failed STARR procedure. Int J Colorectal Dis. 2009;24:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 25. | Pescatori M, Gagliardi G. Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol. 2008;12:7-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 195] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 26. | Lehur PA, Stuto A, Fantoli M, Villani RD, Queralto M, Lazorthes F, Hershman M, Carriero A, Pigot F, Meurette G. Outcomes of stapled transanal rectal resection vs. biofeedback for the treatment of outlet obstruction associated with rectal intussusception and rectocele: a multicenter, randomized, controlled trial. Dis Colon Rectum. 2008;51:1611-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Ommer A, Albrecht K, Wenger F, Walz MK. Stapled transanal rectal resection (STARR): a new option in the treatment of obstructive defecation syndrome. Langenbecks Arch Surg. 2006;391:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Dodi G, Pietroletti R, Milito G, Binda G, Pescatori M. Bleeding, incontinence, pain and constipation after STARR transanal double stapling rectotomy for obstructed defecation. Tech Coloproctol. 2003;7:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 110] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Isbert C, Jayne D, Germer CT, Boenicke L. Severe mesorectal bleeding after stapled transanal rectal resection (STARR-operation) using the 'Contour Transtar Curved Cutter Stapler'. Colorectal Dis. 2010;12:494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Isbert C, Reibetanz J, Jayne DG, Kim M, Germer CT, Boenicke L. Comparative study of Contour Transtar and STARR procedure for the treatment of obstructed defecation syndrome (ODS)--feasibility, morbidity and early functional results. Colorectal Dis. 2010;12:901-908. [PubMed] |
| 31. | Renzi A, Talento P, Giardiello C, Angelone G, Izzo D, Di Sarno G. Stapled trans-anal rectal resection (STARR) by a new dedicated device for the surgical treatment of obstructed defaecation syndrome caused by rectal intussusception and rectocele: early results of a multicenter prospective study. Int J Colorectal Dis. 2008;23:999-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Ommer A, Rolfs TM, Walz MK. Long-term results of stapled transanal rectal resection (STARR) for obstructive defecation syndrome. Int J Colorectal Dis. 2010;25:1287-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Madbouly KM, Abbas KS, Hussein AM. Disappointing long-term outcomes after stapled transanal rectal resection for obstructed defecation. World J Surg. 2010;34:2191-2196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Schwandner O, Fürst A. Assessing the safety, effectiveness, and quality of life after the STARR procedure for obstructed defecation: results of the German STARR registry. Langenbecks Arch Surg. 2010;395:505-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Jayne DG, Schwandner O, Stuto A. Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR Registry. Dis Colon Rectum. 2009;52:1205-1212; discussion 1212-1214. [PubMed] |
| 36. | Gosselink MJ, Hop WC, Schouten WR. Rectal compliance in females with obstructed defecation. Dis Colon Rectum. 2001;44:971-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |