Published online Aug 14, 2011. doi: 10.3748/wjg.v17.i30.3554
Revised: December 21, 2010
Accepted: December 28, 2010
Published online: August 14, 2011
Hepatectomy is an effective surgical treatment for multiple bilobar liver metastases from colon cancer; however, one of the primary obstacles to completing surgical resection for these cases is an insufficient volume of the future remnant liver, which may cause postoperative liver failure. To induce atrophy of the unilateral lobe and hypertrophy of the future remnant liver, procedures to occlude the portal vein have been conventionally used prior to major hepatectomy. We report a case of a 50-year-old woman in whom two-stage hepatectomy was performed in combination with intraoperative ligation of the portal vein and the bile duct of the right hepatic lobe. This procedure was designed to promote the atrophic effect on the right hepatic lobe more effectively than the conventional technique, and to the best of our knowledge, it was used for the first time in the present case. Despite successful induction of liver volume shift as well as the following procedure, the patient died of subsequent liver failure after developing recurrent tumors. We discuss the first case in which simultaneous ligation of the portal vein and the biliary system was successfully applied as part of the first step of two-stage hepatectomy.
- Citation: Iida H, Yasui C, Aihara T, Ikuta S, Yoshie H, Yamanaka N. Simultaneous bile duct and portal venous branch ligation in two-stage hepatectomy. World J Gastroenterol 2011; 17(30): 3554-3559
- URL: https://www.wjgnet.com/1007-9327/full/v17/i30/3554.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i30.3554
Hepatectomy has been established as an effective treatment method for liver metastases from colon cancer, but there are some limits to this procedure when indicated in cases of synchronous multiple bilobar liver metastases. One of the reasons that limit resectability for these cases is an insufficient volume of the future remnant liver, which poses a risk of postoperative liver failure. To address this concern and improve the resectability, ligation or embolization of the portal vein is used in clinical settings. In addition, according to several animal experiments, ligation of the bile duct effectively induces atrophy of the ipsilateral liver.
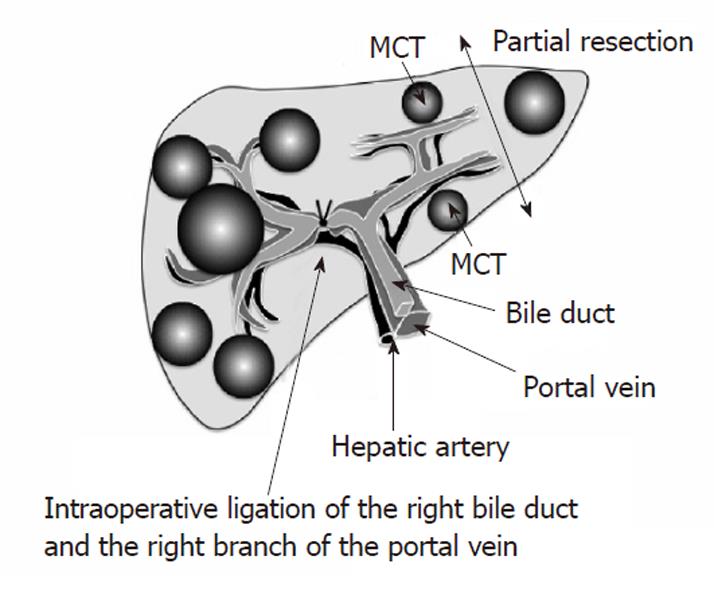
For the present case of synchronous multiple bilobar liver metastases from cecal cancer, we first performed a right hemicolectomy and a segment 3 resection combined with microwave coagulation therapy (MCT) of the metastatic tumors situated in the left hepatic lobe, together with simultaneous ligation of the right portal vein and right-sided bile duct. Second, we performed an extended right hepatic lobectomy. Here, we discuss the effectiveness of intraoperative simultaneous ligation of the unilateral portal vein and bile duct applied to two-stage hepatectomy, as a therapeutic strategy for multiple bilobar liver metastases.
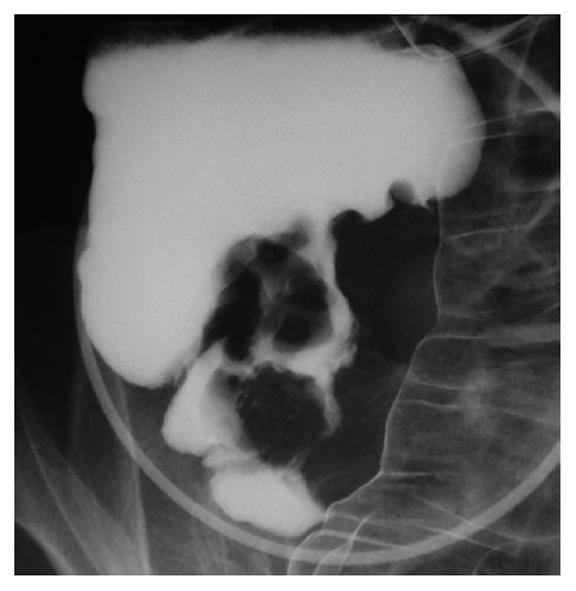
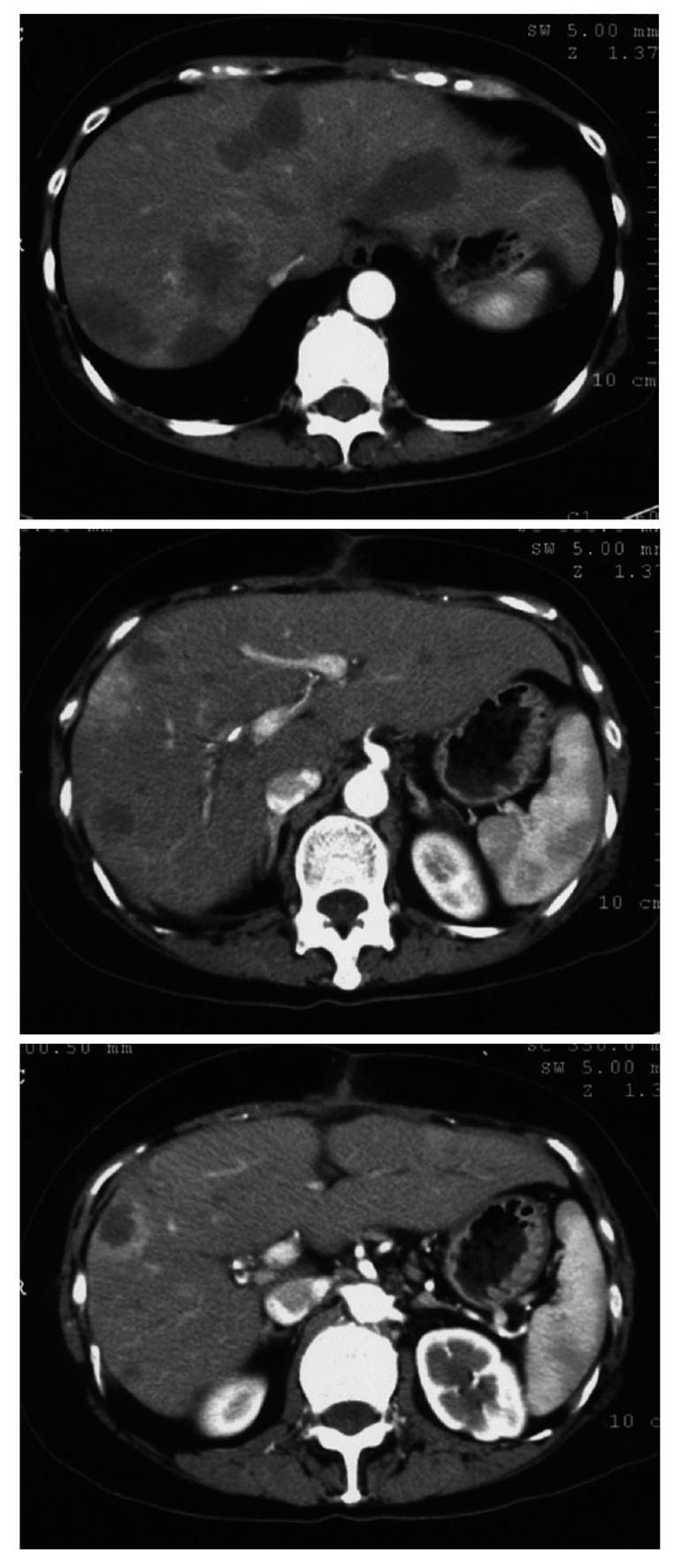
A 50-year-old woman began to have back pain and nausea around December 2004 and was referred to our hospital. Her liver was palpable at three finger widths below the right costal arch. The palpebral conjunctiva was anemic but bulbar conjunctiva was not icteric. Blood tests suggested that she had anemia (hemoglobin and hematocrit levels were 9.7 g/dL and 30.7%, respectively) and liver dysfunction (lactate dehydrogenase, aspartate aminotransferase, alanine aminotransferase, and alkaline phosphatase were 1295 IU/L, 49 IU/L, 47 IU/L and 595 IU/L, respectively). The serum levels of carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9 were 22 120 ng/mL and 16 354 U/mL, respectively (Table 1). Barium enema showed a filling defect in the cecum. The results of biopsy indicated moderately differentiated adenocarcinoma (Figure 1). Contrast-enhanced computer tomography (CT) of the abdomen revealed many metastatic nodules with 2-6 cm diameter in the right hepatic lobe and three nodules with 3-3.5 cm diameter in the left hepatic lobe. A preoperative volume rate of the right hepatic lobe was 56.3% (Figure 2). There were no other metastases. Before implementation of two-stage hepatectomy, preoperative chemotherapy (TS-1: tegafur, gimeracil, and oteracil) was initiated at a starting dose of 80 mg/d. Four weeks later, the liver metastases shrank markedly and the serum levels of CEA and CA 19-9 decreased to 12 680 ng/dL and 8640 U/mL, respectively.
| Laboratory finding | Values |
| Leukocytes | 8300/μL |
| Hemoglobin | 9.7 g/dL |
| Hematocrit | 30.70% |
| Platelets | 408 000/μL |
| Alkaline phosphatase | 595 IU/L |
| Lactate dehydrogenase | 1295 IU/L |
| Aspartate aminotransferase | 49 IU/L |
| Alanine aminotransferase | 47 IU/L |
| Total-bilirubin | 0.4 mg/dL |
| Direct-bilirubin | 0.1 mg/dL |
| CEA | 22 120 ng/dL |
| CA 19-9 | 16 354 U/mL |
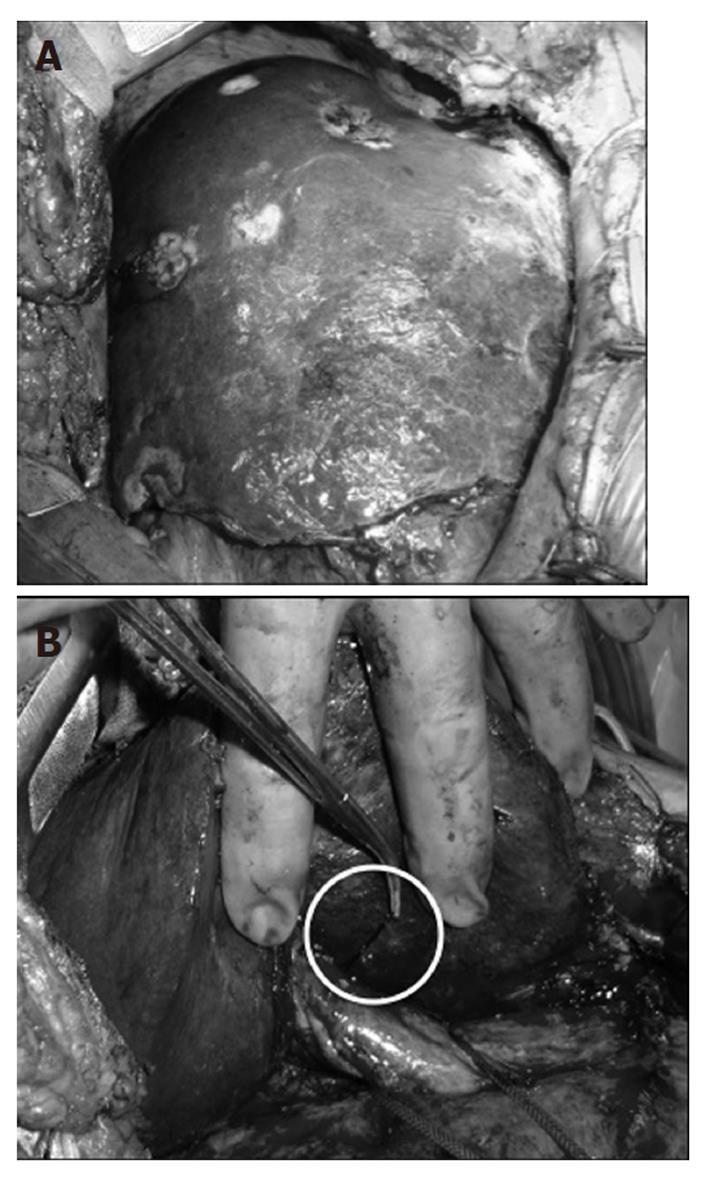
Written informed consent was obtained from the patient and her family prior to the new surgical procedure. In March 2005, a right hemicolectomy was performed. At the same time, the metastatic tumor in segment 3 was resected, and the metastatic tumors in segments 2 and 4 were coagulated using MCT (90 W, 60 s). Furthermore, the right bile duct and right branch of the portal vein were ligated simultaneously (Figure 3). Intraoperative cholangiography was performed after ligation to confirm complete occlusion of the right bile duct and no constriction of the contralateral bile duct. Contrast-enhanced CT of the abdomen performed at 1 wk after surgery showed coagulated areas in the left hepatic lobe and dilation of the right bile duct. Ligation of the right branch of the portal vein resulted in a complementary increase in the right hepatic arterial blood flow. The volume rate of the right hepatic lobe was 55.0%, which was similar to the preoperative rate (Figure 4). However, abdominal CT performed at 1 mo after surgery showed that the volume rate of the right hepatic lobe decreased to 44.3%, along with compensatory hypertrophy of the left hepatic lobe. This liver volume shift was approximately 12% from the right to the left lobe. No viable tumors were observed in the left hepatic lobe (Figure 5).
An extended right hepatic lobectomy was performed in May 2005. There were 10 nodules with 1-4 cm diameter in the right hepatic lobe. The resection was performed using a suture of the right bile duct and the right branch of the portal vein. The weight of the resected specimen was 555 g (Figure 6). There was no complication in the postoperative course. However, in October 2005, two recurrent nodules with 3.2 cm and 1.8 cm diameter were found in the remaining liver. She did not accept repeat resection, therefore, percutaneous radiofrequency ablation was performed.
In November 2005, the biweekly administration of oxaliplatin (80 mg), levofolinate calcium (125 mg), and 5-fluorouracil (1250 mg) was started, leading to some improvement for a while; specifically, a decrease in the serum levels of CEA and CA 19-9 to 36.3 ng/dL and 96 U/mL, respectively. Nevertheless, further recurrence was observed in the remaining liver. At 1 year and 8 mo after the initial operation, the patient developed liver failure and died (Figure 7). There was no other distant metastasis.
Liver metastasis occurs in 40%-70% of patients with colon cancer, and 15-30% of these patients develop multiple liver metastases in both lobes[1]. However, in comparison to other cancers, we can expect long-term survival by using a combined therapy of resection and chemotherapy. In particular, hepatectomy is widely used as the most effective surgical treatment, and the 5-year survival rate after a curative resection is 24%-44%[2]. Even for multiple liver metastases in both lobes previously considered unresectable, complete resection is feasible in some cases by adopting preoperative portal vein embolization in addition to chemotherapy. In 2004, Jaeck et al[3] reported a method called two-stage hepatectomy; applicable to cases of multiple bilobar liver metastases. In the first stage of the operation, they conducted a partial hepatic resection or ablation for the unilateral lobe, and at the same time embolized the portal vein in order to induce hypertrophy of the future remnant lobe. In the second stage of the operation, hepatic lobectomy was performed in the atrophic lobe. They reported that the 1-year survival rate was 70% and the 3-year survival rate was 54.4%[3]. Moreover, for two-stage hepatectomy conducted by Togo et al[4], the 1-year survival rate was 90% and the 3-year survival rate was 45%. The treatment strategy includes combined therapy of systemic chemotherapy, arterial infusion therapy and ablation therapy. Such a multidisciplinary therapy allows resection of marginal or so-called unresectable tumors and contributes to improvement in the prognosis.
Ligation of the portal vein of the unilateral lobe is well-known to induce atrophy of the unilateral hepatic lobe and hypertrophy of the future remnant liver. Honjo et al[5] clinically applied this technique to a case of liver metastasis in 1961. Such a method was adopted for cases of major resection initially considered to have a high risk of postoperative liver failure based on preoperative prognosis[6-9]. Reportedly, at 3-4 mo after occlusion of the right portal vein, 9.5%-14.5% of the liver volume was transferred from the right to the left lobe[10]. In addition, according to a literature review of animal experiments, in 1920, Rous et al[11] reported that atrophy of the ligated lobe and hypertrophy of the future remnant lobe were induced in mice after bile duct ligation. Subsequently, Tanaka et al[12] have reported that the atrophic rate was enhanced after portal vein embolization in a rabbit that had undergone bile duct ligation. It was also pointed out that occlusion of the bile duct and portal vein could reduce biligenesis and occurrence of complications[12].
We applied these findings to the initial surgery in the present case and used simultaneous ligation of the bile duct and portal vein, with an aim of promoting an atrophic effect in the right hepatic lobe. As a result, 12.0% of the liver volume was transferred from the right to the left hepatic lobe at 1 mo after ligation, and the amount of this volume shift could reverse the primary unresectablity. The possible explanation that we consider for the benefit of our simultaneous ligation strategy is that it can overcome several factors that may diminish the atrophic effect of the conventional technique. The bile duct not being ligated may allow the portal blood flow to remain, due to backflow from the hepatic vein and the use of an arterio-portal shunt. In our clinical experience of four cases in which the right portal vein alone was ligated, the volume shift at 1 mo after the procedure was only 5.4% ± 1.6% (Tables 2 and 3), which suggests that ligation of the bile duct made a substantial contribution to inducing atrophy of the ipsilateral liver in the present case.
| Case No. | Age | Sex | Primary disease |
| Case 1 | 55 years | Female | Multiple liver metastasis |
| Case 2 | 61 years | Male | Multiple liver metastasis |
| Case 3 | 61 years | Male | Hepatocellular carcinoma |
| Case 4 | 58 years | Male | Hepatocellular carcinoma |
| Case No. | Preoperative volumerate of RHL | The volume rate of RHL 1 mo after PVL |
| Case 1 | 74.80% | 68.50% |
| Case 2 | 68.30% | 62.50% |
| Case 3 | 58.60% | 55.50% |
| Case 4 | 58.90% | 52.40% |
Regarding the limitations of our simultaneous ligation strategy, it should be noted that this technique should be performed with careful consideration of the risks of obstructive cholangitis and involution of the contralateral bile duct. Intraoperative cholangiography may help avoid these occurrences. With respect to the risks of the aforementioned complications, the safety of our procedure remains to be confirmed in a future study.
To the best of our knowledge, there has not been any reported case in which simultaneous ligation of the portal vein and bile duct has been used in two-stage hepatectomy. There was no postoperative biliary tract infection in our patient. Unfortunately, the patient developed further recurrent tumors after hepatectomy and died of subsequent liver failure. Yet, it can be concluded that the simultaneous ligation strategy could be used to accelerate atrophy of the hemiliver to be resected, and thereby provide us with a further possibility of addressing the primary unresectability of metastatic bilobar liver tumors.
Peer reviewer: Boon-Hun Yong, Department of Anaesthe-siology and 2Adult Intensive Care Unit, Queen Mary Hospital, Hong Kong, China
S- Editor Tian L L- Editor Kerr C E- Editor Zhang DN
| 1. | Adam R, Lucidi V, Bismuth H. Hepatic colorectal metastases: methods of improving resectability. Surg Clin North Am. 2004;84:659-671. [PubMed] [DOI] [Full Text] |
| 2. | Jain S, Sacchi M, Vrachnos P, Lygidakis NJ, Andriopoulou E. Recent advances in the treatment of colorectal liver metastases. Hepatogastroenterology. 2005;52:1567-1584. [PubMed] |
| 3. | Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P. A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg. 2004;240:1037-1049; discussion 1037-149;. [PubMed] [DOI] [Full Text] |
| 4. | Togo S, Nagano Y, Masui H, Tanaka K, Miura Y, Morioka D, Endo I, Sekido H, Ike H, Shimada H. Two-stage hepatectomy for multiple bilobular liver metastases from colorectal cancer. Hepatogastroenterology. 2005;52:913-919. [PubMed] |
| 5. | Honjo I, Suzuki T, Ozawa K, Takasan H, Kitamura O. Ligation of a branch of the portal vein for carcinoma of the liver. Am J Surg. 1975;130:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 88] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Yamanaka N, Okamoto E, Kuwata K, Tanaka N. A multiple regression equation for prediction of posthepatectomy liver failure. Ann Surg. 1984;200:658-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 143] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Yamanaka N, Okamoto E, Oriyama T, Fujimoto J, Furukawa K, Kawamura E, Tanaka T, Tomoda F. A prediction scoring system to select the surgical treatment of liver cancer. Further refinement based on 10 years of use. Ann Surg. 1994;219:342-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 130] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Okamoto E, Kyo A, Yamanaka N, Tanaka N, Kuwata K. Prediction of the safe limits of hepatectomy by combined volumetric and functional measurements in patients with impaired hepatic function. Surgery. 1984;95:586-592. [PubMed] |
| 9. | Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, Yamazaki S, Hasegawa H, Ozaki H. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521-527. [PubMed] |
| 10. | Yamanaka N, Okamoto E, Toyosaka A, Tanaka N, Yabuki K, Kato T, Tomimoto Y, Nakao N. A volumetric study of human liver after intentional occlusion of the unilateral portal vein. J Jpn Surg Assoc. 1985;46:532-538. |
| 11. | Rous P, Larimore LD. RELATION OF THE PORTAL BLOOD TO LIVER MAINTENANCE : A DEMONSTRATION OF LIVER ATROPHY CONDITIONAL ON COMPENSATION. J Exp Med. 1920;31:609-632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 248] [Cited by in RCA: 226] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 12. | Tanaka J, Ishiyama S, Fuse A, Tsukamoto M. Regeneration of liver after transcatheter portal embolization-Especially under the condition with partial cholestasis. Jpn J Gastroenterol Surg. 1996;29:2098-2105. |