INTRODUCTION
Intrathoracic gastric volvulus is an uncommon disease entity characterized by an enlarged esophageal hiatus and weakened gastrosplenic and gastrocolic ligaments[1]. Although gastric volvulus possibly occurs in all ages, it often occurs over the fourth decade of life. If undiagnosed, it can lead to ulceration, perforation, hemorrhage or ischemia of the incarcerated gastrointestinal tract[2]. Two types of gastric volvulus have been recognized: an organoaxial form and a mesenterioaxial form[3,4]. The mesenterioaxial form is characterized by rotation at the transverse axis, extending from the middle of the greater curvature to the porta hepatis.
We recently experienced a case of intrathoracic mesenterioaxial volvulus of the distal portion of the stomach and duodenum, which was successfully treated with laparoscopic repair of the hiatal defect using a polytetrafluoroethylene mesh associated with Toupet fundoplication. The laparoscopic technique employed is described and its therapeutic implications, mesh-related complications, and long-term clinical outcome are discussed.
CASE REPORT
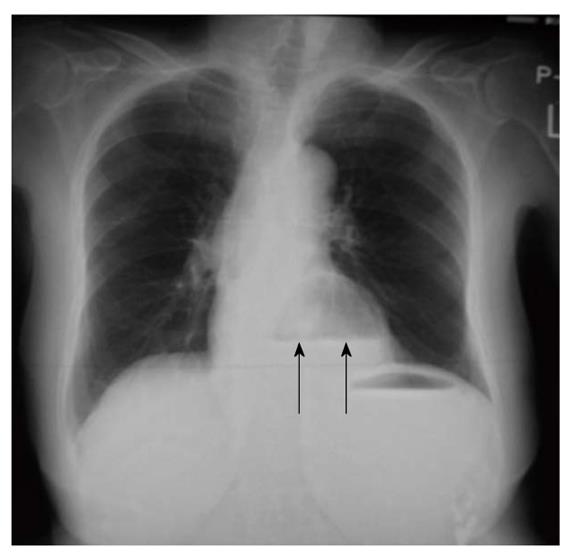
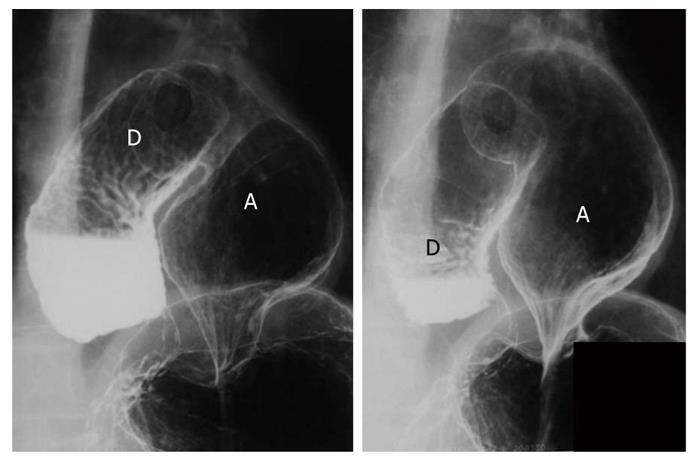
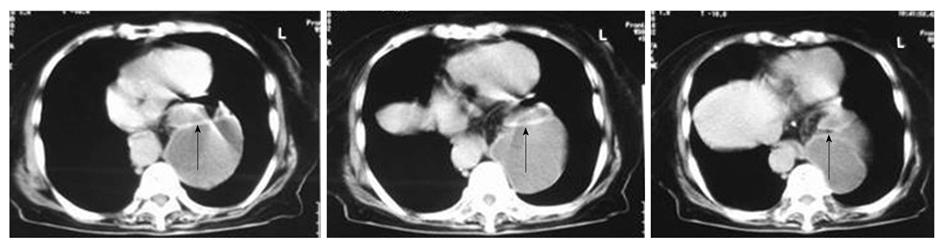
A 70-year-old Japanese woman had been diagnosed with hiatal hernia for several years by her home doctor. Because the patient had complained of no specific symptoms related to the hiatal hernia, no treatment had been undertaken during that period. She had no other past history of any diseases except for a significant kyphosis. She was admitted to our hospital because of the sudden onset of epigastralgia and nausea. Physical examination at admission revealed no abdominal tenderness suggesting diffuse peritonitis. A chest X-ray film showed a large-sized air pocket associated with air-fluid level in the chest, which was likely to be a dilated stomach incarcerated into the intrathoracic cavity (Figure 1). She was dehydrated and vomited during the placement of a nasogastric tube which resulted in aspiration pneumonia. She then presented with acute prerenal failure as a complication, and further treatment was required. Total parenteral nutrition was performed for the management of the intermittent abdominal pain and nausea. The patient responded to intravenous fluid management and the administration of antibiotics. The patient soon recovered from the critically-ill condition and further examinations were performed for precise diagnosis. An upper gastrointestinal series revealed an incarceration of the distal portion of the stomach and the duodenum into the thoracic cavity (Figure 2). An abdominal computed tomography scan also showed an incarcerated upper gastrointestinal tract (Figure 3). These findings were compatible with a mesenterioaxial volvulus of the stomach and duodenum incarcerated into the thoracic cavity through an esophageal hiatus. A laparoscopic approach for the repair of hiatal hernia was selected for complete repair.
Figure 1 A chest X-ray film at admission, revealing air in the dilated stomach associated with air-fluid level (arrows), which was dislocated into the chest.
Figure 2 An upper gastrointestinal series performed preoperatively, revealing dislocated distal portion of the stomach (A) and duodenum (D) into the thoracic cavity rotated in the mesenteric axis, which corresponded to a mesenterioaxial volvulus of the upper gastrointestinal tract.
Figure 3 Abdominal computed tomography scan.
An incarcerated upper gastrointestinal tract in the thoracic cavity (arrows). The gastrointestinal tract dislocated in the thoracic cavity was significantly dilated, where fluid had accumulated.
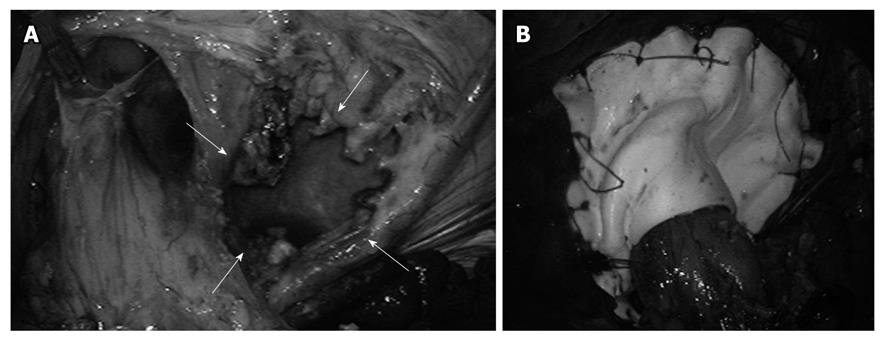
During surgery, pneumoperitoneum was established at an intraabdominal pressure of 12 mmHg. A total of 4 ports were placed, 3 ports of 5 mm diameter in the right and left upper abdomen and left upper abdomen and 1 port of 12 mm diameter in the right middle abdomen. The endoscopic port was placed in the umbilicus. The laparoscopic view during the operation showed a hiatal hernia of the sliding type and also showed that the distal portion of the stomach and the proximal portion of the duodenum were rotated at its transverse axis of the upper gastrointestinal tract, and were incarcerated through the porta of the left crus of the diaphragm. The incarcerated distal stomach and proximal duodenum through the esophageal hiatus was covered with the hernia sac. Because there was no adhesion of the herniated content with the surrounding tissues, the incarcerated stomach and duodenum were deliberately pulled out from the thoracic cavity through a relatively large-sized paraesophageal hiatal defect (Figure 4A). The hernia sac and crus of the diaphragm were then dissected. The lower esophagus was also mobilized. The hiatal defect was closed and was reinforced by using a polytetrafluoroethylene (PTFE) mesh (Figure 4B). Toupet fundoplication was then added to prevent gastroesophageal reflux. The fundic wrap was sutured with the right crus and left-sided diaphragm with interrupted sutures. No intra- and/or postoperative complications were observed. Postoperative upper gastrointestinal series performed 5 d after surgery revealed appropriate arrangement of the upper gastrointestinal tract and no sign of recurrence of the hiatal hernia (Figure 5).
Figure 4 Laparoscopic view after initial reduction of the stomach from the chest into the abdomen.
Sliding hernia and parahiatal hernia. A: A paraesophageal aperture (arrows) was large-sized and was located at the left side of the left crus of the esophageal hiatus; B: Hernia orifice was closed using the mesh reinforcement.
Figure 5 A postoperative upper gastrointestinal series performed at 5 d after surgery, showing the normal intraperitoneal location of the stomach and duodenum.
The postoperative course was uneventful and the patient was discharged from the hospital 15 d after surgery. The patient was in good condition, and complained of no symptoms suggesting the recurrence of hiatal hernia and/or intrathoracic gastric volvulus for 4 years after surgery. The patient has undergone annual check-ups using upper gastrointestinal endoscopic examinations for 4 years after surgery and no recurrence has been found to date.
DISCUSSION
Although hiatal hernia is commonly encountered, hiatal hernia with mesenterioaxial intrathoracic gastric volvulus is extremely uncommon. Two types of gastric volvulus have been recognized: an organoaxial form and a mesenterioaxial form[3,4]. The organoaxial type is a common type of gastric volvulus, in which the stomach rotates on a vertical axis. This type of gastric volvulus is usually caused by eventuation, diaphragmatic hernia, pyloric obstruction, adhesions, or enlarged esophageal hiatus. This is also described as an intrathoracic stomach or upside down stomach. Another type is the mesenterioaxial form. In this form, the stomach rotates on a horizontal axis, which extends from the middle of the greater curvature to the porta hepatis. The rotated stomach is located in the chest from the hiatal defect. Mesenterioaxial volvulus is even more uncommon and represents about 29% of all torsions occur in the stomach. Of mesenterioaxial volvulus, the idiopathic pattern was 37%[3].
In the present case, the patient had gastrointestinal obstruction, dehydration and acute prerenal failure caused by the volvulus of the stomach. Elective surgery was performed after recovering from these complications. In fact, emergency surgery is occasionally required for cases with acute gastric obstruction associated with strangulation due to gastric volvulus[5]. If there is no gastrointestinal ischemia and/or necrosis requiring emergency surgery, placement of a nasogastric tube may be useful for the effective decompression of the stomach, which may allow a reduction of the volvulus and thereby enabling elective surgery.
Treatment of gastric volvulus has classically involved reduction of the stomach, gastropexies in its normal intra-abdominal position, and correction of the associated diaphragmatic defect[4]. The laparoscopic repair of intrathoracic gastric volvulus and large paraesophageal hernias has been proved to be feasible and safe[4,6-9]. Previously published reports have confirmed the significant benefits of the minimally-invasive approach in these often elderly and/or debilitated patients[7]. Therefore, laparoscopic repair of gastric volvulus is best suited as a minimally-invasive approach as long as the precise repair of hiatal aperture and reinforcement are added.
In the present case, Toupet fundoplication was added to prevent gastroesophageal reflux because a simple reduction of the volvulus associated with gastropexy has been shown to be unsatisfactory[10]. A concomitant antireflux procedure has been recommended[8]. The fundoplication is mandatory as it prevents reflux because of the extensive dissection at the hiatus, and provides a good anchor for the repair. This approach is considered to be safe and effective, and it also provides for rapid recovery from the operation.
In the present case, neither mesh-related complications nor recurrence of hiatal hernia was found for 4 years after surgery. It has been reported that primary laparoscopic hiatal hernia for paraesophageal hernia is associated with up to a 42% recurrence rate[11,12]. The most important reason is the absence of strong fascia at the hiatal aperture leading to suture pullout[13]. We decided to use synthetic mesh reinforcement for the crural repair, because direct suturing of the aperture of paraesophageal defect was difficult due to the size and the absence of strong fascia. Although mesh repair improved the recurrence rate[14], the use of mesh for the repair of hiatal hernia has still been controversial because mesh-related complications have frequently reported. Several clinical studies with significant patient numbers have demonstrated the safety and effectiveness of synthetic mesh reinforcement for the repair of hiatal hernia[14,15,16]. An improved recurrence rate has been reported in cases with the use of mesh for the tension free crural repair[17]. However, some surgeons have pointed out the risk of erosion into the esophageal or gastric lumen caused by placing the mesh[15,11,18]. Because several types of nonabsorbable mesh have recently been used for the repair of hiatal hernia[9,19], further evaluation of clinical outcome may be required. Stadlhuber et al[17] analyzed 28 cases of mesh-related complications in patients undergoing laparoscopic or open hiatal closure. They demonstrated that 23 cases required reoperation, and surprisingly 7 patients required esophagectomy. Among the patients who required reoperation, PTFE was used in 12 cases for the hiatal repair. A total of 10 patients had mesh intraluminal erosion, 2 patients had dense hiatal fibrosis. Although there is no apparent relationship between mesh type and configuration with the complications, they suggested that it may be due both to the technical aspects of mesh placement and to the type of mesh material used[17]. Nonetheless, they concluded that complications related to synthetic mesh placement at the esophageal hiatus are more common than previously reported and that further studies are needed to determine the best method and type of mesh for implantation.
In summary, we experienced a case with mesenterioaxial volvulus of the stomach and duodenum associated with hiatal hernia, which was successfully treated with complete laparoscopic repair of the large-sized hiatal defect using a PTPE mesh associated with Toupet fundoplication. These laparoscopic procedures are safe and useful to obtain short-term as well as long-term clinical outcomes of patients with a large-sized hiatal hernia. Further accumulation of cases is required to precisely determine the best method and type of mesh for reinforcement and long-term clinical outcome.