Published online Mar 21, 2011. doi: 10.3748/wjg.v17.i11.1400
Revised: December 22, 2010
Accepted: December 29, 2010
Published online: March 21, 2011
Nodular regenerative hyperplasia (NRH) is a rare liver condition characterized by a widespread benign transformation of the hepatic parenchyma into small regenerative nodules. NRH may lead to the development of non-cirrhotic portal hypertension. There are no published systematic population studies on NRH and our current knowledge is limited to case reports and case series. NRH may develop via autoimmune, hematological, infectious, neoplastic, or drug-related causes. The disease is usually asymptomatic, slowly or non-progressive unless complications of portal hypertension develop. Accurate diagnosis is made by histopathology, which demonstrates diffuse micronodular transformation without fibrous septa. Lack of perinuclear collagen tissue distinguishes NRH from typical regenerative nodules in the cirrhotic liver. While the initial treatment is to address the underlying disease, ultimately the therapy is directed to the management of portal hypertension. The prognosis of NRH depends on both the severity of the underlying illness and the prevention of secondary complications of portal hypertension. In this review we detail the epidemiology, pathogenesis, diagnosis, management, and prognosis of NRH.
- Citation: Hartleb M, Gutkowski K, Milkiewicz P. Nodular regenerative hyperplasia: Evolving concepts on underdiagnosed cause of portal hypertension. World J Gastroenterol 2011; 17(11): 1400-1409
- URL: https://www.wjgnet.com/1007-9327/full/v17/i11/1400.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i11.1400
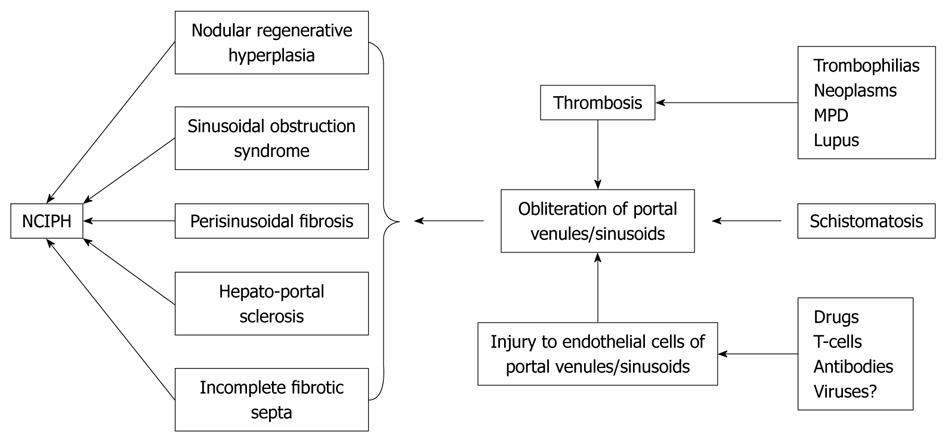
Nodular regenerative hyperplasia (NRH) belongs to the category of liver diseases responsible for non-cirrhotic intrahepatic portal hypertension (NCIPH)[1], which include sinusoidal obstruction syndrome, perisinusoidal fibrosis, hepatoportal sclerosis and incomplete septal cirrhosis (Figure 1). In these conditions, the etiology is ascribed to an intrahepatic hypercoaguable state, possibly secondary to sinusoidal endothelial injury. In many Asian countries, the most frequent cause of NCIPH is schistosomiasis.
NRH was first defined by Steiner[2] in 1959 as a condition characterized by diffuse benign transformation of the hepatic parenchyma into small regenerative nodules distributed evenly throughout the liver with minimal or no fibrosis in the perisinusoidal or periportal areas. This feature distinguishes NRH from other causes of NCIPH[1]. The presence of fibrous septa between the nodules definitively excludes NRH. However, in rare cases, one patient may exhibit histopathologic features of both NRH and other NCIPH disorders. These observations suggest that similar etiological factors may induce various adaptive liver reactions.
Over the last two decades, multiple labels have been applied to describe what we now define as NRH. Terms such as “miliary hepatocellular adenomatosis”, “non-cirrhotic nodulation”, “hepatocellular adenomatosis”, or “adenomatous hyperplasia” have been previously used. Although our current knowledge is limited to single case reports and case series, the number of patients being given the diagnosis of NRH has dramatically increased in recent years. Up to the year 2000 approximately 200 patients had been reported, whereas in the last decade more than 260 new cases of NRH were reported worldwide.
As stated previously, our understanding of the epidemiology of NRH is based upon case reports rather than systematic population studies. In the United States National Library of Medicine/National Library of Medicine (PubMed) database (http://www.ncbi.nlm.nih.gov) 375 case reports have been published since 1975, however, not all cases meet the strict histopathologic criteria for NRH. For example, earlier publications used the term “nodular regenerative hyperplasia” as a misnomer for large regenerative nodules (LRN), associated with postsinusoidal obstructive conditions such as congestive cardiomyopathy or Budd-Chiari syndrome.
NRH comprises 27% of all cases of non-cirrhotic portal hypertension in Europe and about 14% in Japan[3-5]. Autopsy studies indicate an overall incidence ranging between 0.72% and 2.6%[6-8]. Timely clinical diagnosis of NRH is challenging, because the majority of patients do not present with symptoms of portal hypertension. In cases where the etiology of portal hypertension was unclear the histology disclosed NRH in less than 1%[9,10]. While NRH is rare in comparison to other causes of portal hypertension, its presence is being increasingly recognized.
In the case reports we reviewed, the majority of patients were between 25 and 60 years old at diagnosis, with rare cases in children and even fetuses[1]. According to autopsy studies, the risk of development of NRH and its potential complications increases with age. In 2500 autopsies the incidence of NRH after 80 years of age was 6%, seven times greater than in people under 60 years of age[6]. One case series reported the prevalence of NRH in six siblings distributed in three unrelated families indicating the possibility of a family distribution of this disease[11]. Sex and ethnicity seem to play no role in development of NRH.
NRH appears to be a result of an adaptive hyperplastic reaction of hepatocytes. Normally, the mitotic activity of hepatocytes is very low; hyperplasia is considered to be a physiological response to injury. Increased oxygen and nutrient demand, chronic inflammation, hormone-mediated dysfunction or compensation for damage or disease elsewhere play an important role in this process.
The pathogenesis of NRH seems to be related to abnormalities of portal hepatic blood flow akin to the “atrophy-hypertrophy complex”. Hemodynamic disturbances at the level of the hepatic microvasculature occur either secondary to a mechanical obstruction or functional blood flow alterations. One hypothesis is that local portal venous hypoperfusion leads to apoptosis and hepatocyte atrophy, coexisting with maintained or increased blood supply to adjacent acini cells. Local hyperperfusion leads, in turn, to elevated levels of cell growth activators which act as autocrine or paracrine peptides. This hypothesis has been supported by both histopathologic examinations of liver biopsies as well as animal experiments, which showed microvascular changes involving either portal vein radicles or less frequently, arterial or hepatic vein branches. Wanless coined a “portal obliterative venopathy” phenomenon of recurrent embolization of the portal venules by platelet aggregates or thrombi originating in the portal venous system or in the spleen. The ensuing vascular inflammation and fibrosis results in reduced luminal patency of portal vein radicles and local reduction in blood supply to the liver, confirmed in 64 autopsies[6]. Nakanuma et al[5] also provided evidence of obliterated portal venules in 107 liver biopsies of patients with NRH. There are few case reports of NRH without vasculopathy[12], e.g. diffuse carcinoid tumor, where multifocal liver ischemia is due to a functional and not an organic cause[13].
NRH is commonly found in patients with Abernathy’s Syndrome a condition that includes the rare anomaly of congenital absence of the portal vein. The intestinal and splenic veins drain directly into the inferior vena cava, bypassing the liver entirely. It is an extreme model of vascular pathology, where the entire liver relies upon high-pressure arterial perfusion. Rare cases of NRH were also reported in patients with thrombosis of portal vein trunk[14,15].
Immunosuppressive medications may induce NRH by damaging endothelial cells of small hepatic veins. There are several reports of NRH developing in response to prolonged treatment with thiopurines, including azathioprine (AZA), 6-mercaptopurine and 6-thioguanine (6-TG). NRH was found in a single case among 30 patients treated with thiopurines for Crohn’s disease. Accumulation of toxic metabolites may be a factor, as NRH was found more frequently in post-transplant patients with impaired metabolism of AZA due to the thiopurine-methyltransferase mutation[16]. In another study NRH was found on liver biopsy in three patients treated with AZA for inflammatory bowel disease for more than 1 year, who presented with elevated liver enzymes[17]. Gane et al[18] demonstrated histological regression of NRH with normalization of liver enzymes in four patients after withdrawal of AZA, after being used for an average of 64 mo. While the etiology of this remains to be elucidated, it has been stated that 6-TG, used in treatment of AZA-resistant forms of inflammatory bowel disease, may have a higher potential to induce NRH than other thiopurines[19].
Other authors reported NRH in 8% of a human immunodeficiency virus (HIV)-positive cohort receiving highly active antiretroviral therapy (HAART)[20]. Didanozine, a HAART drug responsible for liver injury and pulmonary hypertension, appears to induce NRH[21].
An analysis of 334 liver biopsies from patients with metastatic colorectal cancer demonstrated that vascular pathology (as compared to chemotherapy-associated steatohepatitis) is a predominant histopathologic finding in chemotherapy-induced liver injury[22]. There are numerous reports on NRH developing in patients with disseminated cancer after use of cytostatic drugs. Older reports associate NRH with use of busulphan, thioguanine or cyclophosphamide and, in more recent reports, with oxaliplatin-based therapies. Among 274 patients treated with oxaliplatin, sinusoidal obstruction syndrome and NRH were found in the histopathological study in 54% and 24.5% of patients, respectively. Peliosis and perisinusoidal or perivenular fibrosis were other vasculopathy-related liver diseases[23]. Overall, about 70 cases of oxaliplatin-related NRH were reported in the literature (Table 1).
| Disease | No. of cases | Ref. |
| Pulmonary hypertension | 32 | [11,24-44] |
| Rheumatoid arthritis/Felty’s syndrome | 30 | [31,41,44-55] |
| Human immunodeficiency virus infection | 20 | [21,56-64] |
| Lupus erythematosus | 12 | [27,40,65-70] |
| Crohn’s disease/ulcerative colitis | 13 | [17,28,56,71-76] |
| Celiac disease | 9 | [76-80] |
| Scleroderma/CREST | 7 | [25,32,81-85] |
| Antiphospholipid syndrome | 11 | [78,79,86-89] |
| Sarcoidosis | 9 | [90] |
| Post-transplant | 18 | [16,37,91-99] |
| Extrahepatic cancers | 26 | [26,59,100-104] |
| Lymphomas | 12 | [29,53,81,105-113] |
| Macroglobulinemia | 5 | [114,115] |
| Mixed cryoglobulinemia | 3 | [25,116,117] |
| ITP/aplastic anemia | 4 | [3,12,118,119] |
| Primary biliary cirrhosis | 6 | [25,82,120-122] |
| Krabbe disease | 4 | [123,124] |
| Congenital absence of portal vein | 4 | [15,125,126] |
| Portal vein thrombosis | 2 | [14,127] |
| Familial pulmonary fibrosis | 4 | [128] |
| Chronic glomerulonephritis | 5 | [51,117,129-131] |
| Cystinosis | 2 | [24] |
| Myasthenia | 2 | [132,133] |
| Polyarteritis nodosa | 2 | [134,135] |
| Common variable immunodeficiency syndrome | 2 | [136,137] |
| Turner’s syndrome | 2 | [138,139] |
| Castleman’s disease | 2 | [78,140] |
| Idiopathic eosinophilic syndrome | 2 | [141,142] |
NRH may develop as a result of underlying disease of autoimmune, inflammatory, neoplastic, or idiopathic origin (Table 1)[143]. In patients with systemic lupus erythematosis (SLE), rheumatoid arthritis, and a host of other autoimmune diseases (including sarcoidosis or other granulomatous liver diseases)[90], antibody reaction to the endothelial cells of small hepatic vessels combined with local hypercoagulation[144] may predispose to NRH. Ziol et al[145] found intrasinusoidal infiltrate composed of cytotoxic CD8+ T-lymphocytes in 32% of 44 patients with NRH. These T-cells were located near atrophic liver cell plates and were adjacent to endothelial cells exhibiting evidence of apoptosis. Moreover, in patients with SLE, anticardiolipin antibodies could be incriminated for portal vasculopathy leading to NRH[78,79,86], although this is not a universal finding in SLE[68].
NRH has also been associated with hematologic disorders, especially myeloproliferative diseases and congenital thrombophilias, where the hypercoaguable state may induce a progressive splenic and portal vein thrombosis and subsequent portal hypertension[2].
One should consider a diagnosis of NRH in all patients with clinical symptoms of portal hypertension (splenomegaly, esophageal varices, ascites) but with normal transaminases and no manifestations of cirrhosis (gynecomastia, palmar erythema, spider nevi). There are mildly increased liver enzymes, usually alkaline phosphatase, in 11%-25% of patients[4,127,146]. It is estimated that NRH is complicated by clinically overt portal hypertension in at least 50% of cases, with an augmented hepatic venous pressure gradient confirming sinusoidal obstruction[147,148]. Close surveillance of patients with predisposing conditions is important for early diagnosis, especially in situations where drug toxicity may play a role. In patients on AZA for autoimmune hepatitis, the occurrence of splenomegaly should alert the clinician to the development of portal hypertension secondary to NRH.
In all cases of NCIPH, more common treatable causes (viruses, alcohol, metabolic and autoimmune disorders) should be eliminated first, followed by an assessment of the usual exposures (acetaminophen, vitamin A, copper sulfate, vinyl chloride, arsenic salt). Portal and hepatic venous thrombosis may be excluded on radiographic imaging.
Imaging methods have poor sensitivity and specificity for NRH. A diffusely heterogeneous hepatic parenchyma may be the only imaging abnormality. On ultrasound, regenerative nodules are usually not visible due to a small size or isoechogenicity. The presence of well-delineated hypoechoic or isoechoic tiny lesions with a sonoluscent rim are indistinguishable from metastases[149]. Hyperechoic nodules have been reported in very rare cases of NRH[150]. On computed tomography (CT), regenerative nodules remain isodense or hypodense in both arterial and portal venous phases, distinguishing NRH from focal nodular hyperplasia and adenomas[3].
The significance of magnetic resonance imaging in the diagnosis of NRH is still controversial, although because of its inherent propensity to resolve soft tissue details it may be superior to CT in visualization of regenerative nodules. NRH lesions appear hyperintense on T1-weighted images and iso- or hypointense on T2-weighted images[67,151], with a sensitivity and specificity of 70%-80% when using gadolinium contrast[152]; others found more disappointing results[153].
Grossly, NRH presents as diffuse fine nodularity of the liver with 1-3 mm diameter nodules. Granularity of the hepatic surface may resemble micronodular cirrhosis[77,144]. Rarely, nodules are larger[7,144], and may coalesce into a large tumor[154,155]. NRH nodules appear paler than the surrounding normal hepatic tissue. Mild hepatomegaly may be present.
The diagnosis of NRH is secured by histopathology demonstrating regenerative nodules without parietal thickening of portal venules, and no or minimal perisinusoidal and portal fibrosis on reticulin staining. Hepatocytes commonly show feathery degeneration of cytoplasm suggesting impairments of bile production or transport. Two morphologically distinct populations of hepatocytes coexist within the nodules: hypertrophied hepatocytes centrally surrounded by atrophic hepatocytes peripherally. Hypertrophic cells may compress terminal hepatic venules, which frequently appear shrunken and may be undetectable. Heterogeneity may be explained by uneven perfusion. Dilated sinusoids and thrombosed portal vein radicles are occasionally present[24,156,157].
If a dominant large regenerative nodule is sampled, adenoma-like features with discrete cytoplasmatic and/or nuclear atypia can be seen. Therefore, sampling a single nodule may yield an incorrect diagnosis and multiple liver sampling becomes necessary. Dysplastic large hepatocytes were seen in 42% of NRH samples, without high-degree dysplasia[9]. NRH should also be distinguished from LRN occurring in livers with disturbed hepatic venous outflow (e.g. Budd-Chiari syndrome, veno oclusive disease, or congestive pericarditis) but well developed compensatory arterialization and preserved hepatic venous collaterals.
It should be kept in mind that in small biopsy samples histologic features of NRH may be lacking or incomplete[158]. The diagnosis can be made after careful examination by the experienced hematopathologist with a high index of suspicion. In justified cases a laparoscopy with open wedge biopsy should be done.
Overlap syndromes, involving both NRH and portal or pericentral fibrosis due to hepatitis C viral infection, alcoholic, or non-alcoholic liver disease, can occur and in such cases the diagnosis of NRH may be easily overlooked[24,77,156]. Fibroscan or fibrotest panels may rule out cirrhosis, but have limited clinical value[153].
Treatment of NRH therapy is directed towards elimination of the causative factor, once established. Concomitant diseases should be treated appropriately and with attention to minimizing drug toxicity. Long-term anticoagulation treatment is usually indicated in the thrombophilias. Anticoagulation therapy was found to be beneficial in early stages of NRH induced by HAART in HIV-infected patients[57].
In patients with NRH, the mainstay of management is directed primarily to prevention and treatment of complications related to portal hypertension, i.e. variceal bleeding, the main source of mortality. Treatment of portal hypertension is standard: low sodium diet, diuretics, and endoscopic banding of esophageal varices. Splenectomy is not indicated. A portosystemic surgical shunt or transjugular intrahepatic portosystemic shunt may offer a significant therapeutic benefit, especially in the case of severe recurrent esophageal variceal hemorrhage[56]. Liver transplantation is rarely necessary and is reserved for patients with hepatic failure[159-162].
Generally, the prognosis of NRH is better than that of chronic liver disease and is related to the complications of portal hypertension and the severity of the associated diseases, if present. In most cases the disease is slowly progressive, although the rate of nodular growth may be accelerated for unknown reasons[163]. The long-term prognosis is uncertain and considers the level of underlying myeloproliferative, thrombophilic, or autoimmune processes. There are several case reports demonstrating the presence of both NRH and hepatocellular carcinoma without underlying cirrhosis, although a neoplastic process has yet to be proven[163-167].
NRH is a rare condition of NCIPH liver diseases. Our understanding of the epidemiology of NRH is based upon case reports rather than systematic population studies. Timely diagnosis is challenging, because the majority of patients do not present with overt signs of portal hypertension. The pathogenesis of NRH is not well established, but an adaptive hyperplastic reaction of hepatocytes appears to be related to abnormalities of hepatic venous perfusion. Immunosuppressive medications may induce NRH by damaging endothelial cells of small hepatic veins. NRH may also develop as a result of underlying autoimmune, inflammatory, neoplastic, or idiopathic disease.
The knowledge on tumorigenesis in NRH is virtually non-existent as compared with hepatocellular carcinoma, adenoma and even cirrhotic regeneration. Genetic studies indicate that RASSF1A, a gene acting in the proapoptotic pathway, is increasingly methylated in hepatocellular hyperplastic hepatocytes[168]. Moreover, in ceramide synthase 2 null mice that are unable to synthesize very long acyl chain ceramides, an extensive hepatocellular anisocytosis with widespread formation of regenerative nodules composed of hyperplastic hepatocytes was found[169]. This finding emphasizes the role of ceramide synthase 2 activity and altered hepatic sphingolipid profile for liver proliferative homeostasis.
Common causes of extrahepatic and intrahepatic portal hypertension should be excluded before making a diagnosis of NRH. Imaging may be helpful during the initial clinical encounter with liver biopsy as the gold standard for diagnosis. An accurate diagnosis can only be made on histopathology, which shows diffuse micronodular transformation without fibrous septa. Management is directed primarily for prevention and treatment of complications related to portal hypertension. Outcome and prognosis is related to the severity of both portal hypertensive complications and the underlying associated diseases. Further studies may be helpful to elucidate a molecular mechanism for the vasculopathy that appears to play a central role in the adaptive hyperplastic reaction universally seen in NRH.
Peer reviewer: Qin Su, Professor, Department of Pathology, Cancer Hospital and Cancer Institute, Chinese Academy of Medical Sciences and Peking Medical College, PO Box 2258, Beijing 100021, China
S- Editor Tian L L- Editor Cant MR E- Editor Zheng XM
| 1. | Hillaire S, Bonte E, Denninger MH, Casadevall N, Cadranel JF, Lebrec D, Valla D, Degott C. Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patients. Gut. 2002;51:275-280. |
| 2. | Steiner PE. Nodular regenerative hyperplasia of the liver. Am J Pathol. 1959;35:943-953. |
| 3. | Mahamid J, Miselevich I, Attias D, Laor R, Zuckerman E, Shaoul R. Nodular regenerative hyperplasia associated with idiopathic thrombocytopenic purpura in a young girl: a case report and review of the literature. J Pediatr Gastroenterol Nutr. 2005;41:251-255. |
| 4. | Naber AH, Van Haelst U, Yap SH. Nodular regenerative hyperplasia of the liver: an important cause of portal hypertension in non-cirrhotic patients. J Hepatol. 1991;12:94-99. |
| 5. | Nakanuma Y, Hoso M, Sasaki M, Terada T, Katayanagi K, Nonomura A, Kurumaya H, Harada A, Obata H. Histopathology of the liver in non-cirrhotic portal hypertension of unknown aetiology. Histopathology. 1996;28:195-204. |
| 6. | Wanless IR. Micronodular transformation (nodular regenerative hyperplasia) of the liver: a report of 64 cases among 2,500 autopsies and a new classification of benign hepatocellular nodules. Hepatology. 1990;11:787-797. |
| 7. | Reshamwala PA, Kleiner DE, Heller T. Nodular regenerative hyperplasia: not all nodules are created equal. Hepatology. 2006;44:7-14. |
| 8. | Nakanuma Y. Nodular regenerative hyperplasia of the liver: retrospective survey in autopsy series. J Clin Gastroenterol. 1990;12:460-465. |
| 9. | Colina F, Alberti N, Solis JA, Martinez-Tello FJ. Diffuse nodular regenerative hyperplasia of the liver (DNRH). A clinicopathologic study of 24 cases. Liver. 1989;9:253-265. |
| 10. | Elariny HA, Mizrahi SS, Hayes DH, Boudreaux JP, Hussey JL, Farr GH Jr. Nodular regenerative hyperplasia: a controversial indication for orthotopic liver transplantation. Transpl Int. 1994;7:309-313. |
| 11. | Dumortier J, Boillot O, Chevallier M, Berger F, Potier P, Valette PJ, Paliard P, Scoazec JY. Familial occurrence of nodular regenerative hyperplasia of the liver: a report on three families. Gut. 1999;45:289-294. |
| 12. | González-Huezo MS, Villela LM, Zepeda-Florencio Mdel C, Carrillo-Ponce CS, Mondragón-Sánchez RJ. Nodular regenerative hyperplasia associated to aplastic anemia: a case report and literature review. Ann Hepatol. 2006;5:166-169. |
| 13. | Al-Hamoudi WK, Pasieka JL, Urbanski SJ, Lee SS. Hepatic nodular regenerative hyperplasia in a patient with advanced carcinoid tumor. Eur J Gastroenterol Hepatol. 2009;21:1083-1085. |
| 14. | Fukai T, Ishibashi H, Noda T, Dohmen K, Kudo J, Nagafuchi S, Sueishi K, Yamasaki T, Sameshima H. Nodular regenerative hyperplasia of the liver with portal vein thrombosis and hyperplasia of the adrenal gland. Gastroenterol Jpn. 1992;27:108-114. |
| 15. | McDonald JA, Painter DM, Gallagher ND, McCaughan GW. Nodular regenerative hyperplasia mimicking cirrhosis of the liver. Gut. 1990;31:725-727. |
| 16. | Buster EH, van Vuuren HJ, Zondervan PE, Metselaar HJ, Tilanus HW, de Man RA. Thiopurine-methyltransferase and inosine triphosphate pyrophosphatase polymorphism in a liver transplant recipient developing nodular regenerative hyperplasia on low-dose azathioprine. Eur J Gastroenterol Hepatol. 2008;20:68-72. |
| 17. | Shastri S, Dubinsky MC, Fred Poordad F, Vasiliauskas EA, Geller SA. Early nodular hyperplasia of the liver occurring with inflammatory bowel diseases in association with thioguanine therapy. Arch Pathol Lab Med. 2004;128:49-53. |
| 18. | Gane E, Portmann B, Saxena R, Wong P, Ramage J, Williams R. Nodular regenerative hyperplasia of the liver graft after liver transplantation. Hepatology. 1994;20:88-94. |
| 19. | Teml A, Schwab M, Hommes DW, Almer S, Lukas M, Feichtenschlager T, Florin T, Seiderer J, Petritsch W, Bokemeyer B. A systematic survey evaluating 6-thioguanine-related hepatotoxicity in patients with inflammatory bowel disease. Wien Klin Wochenschr. 2007;119:519-526. |
| 20. | Mallet V, Blanchard P, Verkarre V, Vallet-Pichard A, Fontaine H, Lascoux-Combe C, Pol S. Nodular regenerative hyperplasia is a new cause of chronic liver disease in HIV-infected patients. AIDS. 2007;21:187-192. |
| 21. | Vispo E, Moreno A, Maida I, Barreiro P, Cuevas A, Albertos S, Soriano V. Noncirrhotic portal hypertension in HIV-infected patients: unique clinical and pathological findings. AIDS. 2010;24:1171-1176. |
| 22. | Ryan P, Nanji S, Pollett A, Moore M, Moulton CA, Gallinger S, Guindi M. Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol. 2010;34:784-791. |
| 23. | Rubbia-Brandt L, Lauwers GY, Wang H, Majno PE, Tanabe K, Zhu AX, Brezault C, Soubrane O, Abdalla EK, Vauthey JN. Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasis. Histopathology. 2010;56:430-439. |
| 24. | O'Brien K, Hussain N, Warady BA, Kleiner DE, Kleta R, Bernardini I, Heller T, Gahl WA. Nodular regenerative hyperplasia and severe portal hypertension in cystinosis. Clin Gastroenterol Hepatol. 2006;4:387-394. |
| 25. | Riviere E, Vergniol J, Reffet A, Lippa N, Le Bail B, de Ledinghen V. Gastric variceal bleeding uncovering a rare association of CREST syndrome, primary biliary cirrhosis, nodular regenerative hyperplasia and pulmonary hypertension. Eur J Gastroenterol Hepatol. 2010;22:1145-1148. |
| 26. | Arotçarena R, Calès V, Berthelémy P, Parent Y, Malet M, Etcharry F, Ferrari S, Pariente A. Severe sinusoidal lesions: a serious and overlooked complication of oxaliplatin-containing chemotherapy? Gastroenterol Clin Biol. 2006;30:1313-1316. |
| 27. | Colmegna I, deBoisblanc BP, Gimenez CR, Espinoza LR. Slow development of massive splenomegaly, portal and pulmonary hypertension in systematic lupus erythematosus: can nodular regenerative hyperplasia of the liver explain all these findings? Lupus. 2005;14:976-978. |
| 28. | Daniel F, Cadranel JF, Seksik P, Cazier A, Duong Van Huyen JP, Ziol M, Coutarel P, Loison P, Jian R, Marteau P. Azathioprine induced nodular regenerative hyperplasia in IBD patients. Gastroenterol Clin Biol. 2005;29:600-603. |
| 29. | González-Alegre MT, Guerra-Vales JM, Martínez-González , Gutiérrez A, Guillen V. Nodular regenerative hyperplasia of the liver and Hodgkin's disease: a case report. Acta Gastroenterol Belg. 2004;67:358-360. |
| 30. | Jawaid Q, Saeed ZA, Di Bisceglie AM, Brunt EM, Ramrakhiani S, Varma CR, Solomon H. Biliary-venous fistula complicating transjugular intrahepatic portosystemic shunt presenting with recurrent bacteremia, jaundice, anemia and fever. Am J Transplant. 2003;3:1604-1607. |
| 31. | Gento Peña E, Martín Lorente JL, Echevarría Iturbe C, Pérez Alvarez JC, Sáez-Royuela F, López Morante A, Ojeda Giménez C. [Sinusoidal portal hypertension secondary to nodular regenerative hyperplasia of the liver]. Gastroenterol Hepatol. 1999;22:183-185. |
| 32. | Kaburaki J, Kuramochi S, Fujii T, Kuwana M, Tojo T, Ikeda Y, Hosada Y. Nodular regenerative hyperplasia of the liver in a patient with systemic sclerosis. Clin Rheumatol. 1996;15:613-616. |
| 33. | Henkel M, Paquet KJ, Rühl U. [Correlation between pulmonary hypertension and portal hypertension--2 case reports of different forms of pre-sinusoidal portal hypertension]. Leber Magen Darm. 1994;24:10-14. |
| 34. | Calès P, Voigt JJ, Payen JL, Bloom E, Berg P, Vinel JP, Pradère B, Broussy P, Pascal JP. Diffuse vascular ectasia of the antrum, duodenum, and jejunum in a patient with nodular regenerative hyperplasia. Lack of response to portosystemic shunt or gastrectomy. Gut. 1993;34:558-561. |
| 35. | Portmann B, Stewart S, Higenbottam TW, Clayton PT, Lloyd JK, Williams R. Nodular transformation of the liver associated with portal and pulmonary arterial hypertension. Gastroenterology. 1993;104:616-621. |
| 36. | Trauner M, Stepan KM, Resch M, Ebner F, Pristautz H, Klimpfinger M. Diagnostic problems in nodular regenerative hyperplasia (nodular transformation) of the liver. Review of the literature and report of two cases. Z Gastroenterol. 1992;30:187-194. |
| 37. | Duvoux C, Kracht M, Lang P, Vernant JP, Zafrani ES, Dhumeaux D. [Nodular regenerative hyperplasia of the liver associated with azathioprine therapy]. Gastroenterol Clin Biol. 1991;15:968-973. |
| 38. | Bedossa P, Ngendayo L, Hervé P, Rain B, Poynard T, Simonneau G. [Nodular regenerative hyperplasia and pulmonary arterial hypertension]. Gastroenterol Clin Biol. 1990;14:881-884. |
| 39. | Yutani C, Imakita M, Ishibashi-Ueda H, Okubo S, Naito M, Kunieda T. Nodular regenerative hyperplasia of the liver associated with primary pulmonary hypertension. Hum Pathol. 1988;19:726-731. |
| 40. | Kuramochi S, Tashiro Y, Torikata C, Watanabe Y. Systemic lupus erythematosus associated with multiple nodular hyperplasia of the liver. Acta Pathol Jpn. 1982;32:547-560. |
| 41. | Qizilbash AH, Castelli M. Nodular regenerative hyperplasia of the liver: diagnosis by liver biopsy. Can Med Assoc J. 1980;122:1151-1154. |
| 42. | Lebrec D, Capron JP, Dhumeaux D, Benhamou JP. Pulmonary hypertension complicating portal hypertension. Am Rev Respir Dis. 1979;120:849-856. |
| 43. | Shorey J, Weinberg MN, Frenkel EP, Fallis BD. Nodular regenerative hyperplasia of the liver in a case of myelofibrosis with extramedullary hematopoiesis and secondary portal venous hypertension. Am J Clin Pathol. 1979;72:122-125. |
| 44. | Wechsler J, Belaiche J, Vesin P, Cattan D, Pinaudeau Y. [Anatomo-clinical study of a case of regenerative nodular hyperplasia of the liver with Felty's syndrome and portal hypertension]. Ann Anat Pathol (Paris). 1979;24:325-336. |
| 45. | Riesco Díaz M, Manzano Gómez F, Tirado Domínguez M, Suárez García E, Pujol de la Llave E. [Rheumatoid arthritis and hepatic nodular regenerative hyperplasia]. Rev Clin Esp. 1994;194:70. |
| 46. | Bills LJ, Seibert D, Brick JE. Liver disease, erroneously attributed to methotrexate, in a patient with rheumatoid arthritis. J Rheumatol. 1992;19:1963-1965. |
| 47. | Young ID, Segura J, Ford PM, Ford SE. The pathogenesis of nodular regenerative hyperplasia of the liver associated with rheumatoid vasculitis. J Clin Gastroenterol. 1992;14:127-131. |
| 48. | Perez Ruiz F, Orte Martinez FJ, Zea Mendoza AC, Ruiz del Arbol L, Moreno Caparros A. Nodular regenerative hyperplasia of the liver in rheumatic diseases: report of seven cases and review of the literature. Semin Arthritis Rheum. 1991;21:47-54. |
| 49. | Forbes GM, Shilkin KB, Reed WD. Nodular regenerative hyperplasia of the liver: the importance of combined macroscopic and microscopic findings. Med J Aust. 1991;154:415-417. |
| 50. | Nakad A, Moens P, Najm S, Haot J, Janssen J, Geubel AP. Nodular regenerative hyperplasia of the liver and esophageal varices in Felty's syndrome: a clinicopathologic case report with review of the literature. Acta Clin Belg. 1988;43:45-50. |
| 51. | Reynolds WJ, Wanless IR. Nodular regenerative hyperplasia of the liver in a patient with rheumatoid vasculitis: a morphometric study suggesting a role for hepatic arteritis in the pathogenesis. J Rheumatol. 1984;11:838-842. |
| 52. | Cohen MD, Ginsburg WW, Allen GL. Nodular regenerative hyperplasia of the liver and bleeding esophageal varices in Felty's syndrome: a case report and literature review. J Rheumatol. 1982;9:716-718. |
| 53. | Wanless IR, Godwin TA, Allen F, Feder A. Nodular regenerative hyperplasia of the liver in hematologic disorders: a possible response to obliterative portal venopathy. A morphometric study of nine cases with an hypothesis on the pathogenesis. Medicine (Baltimore). 1980;59:367-379. |
| 54. | Belaiche J, Vesin P, Fischer D, Wechsler J, Franco D, Bismuth H, Cattan D. [Nodular regenerative hyperplasia of the liver with portal hypertension associated with Felty's syndrome. Report of a case (author's transl)]. Gastroenterol Clin Biol. 1978;2:63-70. |
| 55. | Reisman T, Levi JU, Zeppa R, Clark R, Morton R, Schiff ER. Noncirrhotic portal hypertension in Felty's syndrome. Am J Dig Dis. 1977;22:145-148. |
| 56. | Schouten JN, Verheij J, Janssen HL. [Non-cirrhotic portal hypertension: rare cause of upper gastrointestinal bleeding]. Ned Tijdschr Geneeskd. 2010;154:A1276. |
| 57. | Bihl F, Janssens F, Boehlen F, Rubbia-Brandt L, Hadengue A, Spahr L. Anticoagulant therapy for nodular regenerative hyperplasia in a HIV-infected patient. BMC Gastroenterol. 2010;10:6. |
| 58. | Mendizabal M, Craviotto S, Chen T, Silva MO, Reddy KR. Noncirrhotic portal hypertension: another cause of liver disease in HIV patients. Ann Hepatol. 2009;8:390-395. |
| 59. | Kochin I, Magid M, Arnon R, Glasscock A, Kerkar N, Miloh T. Variceal bleeding in an adolescent with HIV diagnosed with hepatoportal sclerosis and nodular regenerative hyperplasia. J Pediatr Gastroenterol Nutr. 2010;50:340-343. |
| 60. | Dinh MH, Stosor V, Rao SM, Miller FH, Green RM. Cryptogenic liver disease in HIV-seropositive men. HIV Med. 2009;10:447-453. |
| 61. | Ding A, Lee A, Callender M, Loughrey M, Quah SP, Dinsmore WW. Hepatic encephalopathy as an unusual late complication of transjugular intrahepatic portosystemic shunt insertion for non-cirrhotic portal hypertension caused by nodular regenerative hyperplasia in an HIV-positive patient on highly active antiretroviral therapy. Int J STD AIDS. 2010;21:71-72. |
| 62. | Tateo M, Sebagh M, Bralet MP, Teicher E, Azoulay D, Mallet V, Pol S, Castaing D, Samuel D, Duclos-Vallée JC. A new indication for liver transplantation: nodular regenerative hyperplasia in human immunodeficiency virus-infected patients. Liver Transpl. 2008;14:1194-1198. |
| 63. | Podevin P, Spiridon G, Terris B, Chauvelot-Moachon L, Guillevin L, Chaussade S, Sogni P, Salmon-Ceron D. Nodular regenerative hyperplasia of the liver after IL-2 therapy in an HIV-infected patient. AIDS. 2006;20:313-315. |
| 64. | Fernandez-Miranda C, Colina F, Delgado JM, Lopez-Carreira M. Diffuse nodular regenerative hyperplasia of the liver associated with human immunodeficiency virus and visceral leishmaniasis. Am J Gastroenterol. 1993;88:433-435. |
| 65. | Leung VK, Loke TK, Luk IS, Ng WL, Chau TN, Law ST, Chan JC. Nodular regenerative hyperplasia of the liver associated with systemic lupus erythematosus: three cases. Hong Kong Med J. 2009;15:139-142. |
| 66. | Leung VK, Ng WL, Luk IS, Chau TN, Chan WH, Kei SK, Loke TK. Unique hepatic imaging features in a patient with nodular regenerative hyperplasia of the liver associating with systemic lupus erythematosus. Lupus. 2007;16:205-208. |
| 67. | Horita T, Tsutsumi A, Takeda T, Yasuda S, Takeuchi R, Amasaki Y, Ichikawa K, Atsumi T, Koike T. Significance of magnetic resonance imaging in the diagnosis of nodular regenerative hyperplasia of the liver complicated with systemic lupus erythematosus: a case report and review of the literature. Lupus. 2002;11:193-196. |
| 68. | Sekiya M, Sekigawa I, Hishikawa T, Iida N, Hashimoto H, Hirose S. Nodular regenerative hyperplasia of the liver in systemic lupus erythematosus. The relationship with anticardiolipin antibody and lupus anticoagulant. Scand J Rheumatol. 1997;26:215-217. |
| 69. | Guitton P, Touchard G, Beauchant M. [Diffuse nodular regenerative hyperplasia of the liver and disseminated lupus erythematosus]. Gastroenterol Clin Biol. 1987;11:102-103. |
| 70. | Klemp P, Timme AH, Sayers GM. Systemic lupus erythematosus and nodular regenerative hyperplasia of the liver. Ann Rheum Dis. 1986;45:167-170. |
| 71. | Bryant DL, Miles CJ, Gearry RB. Nodular regenerative hyperplasia of the liver secondary to azathioprine in a patient with inflammatory bowel disease. N Z Med J. 2010;123:74-76. |
| 72. | Schumann M, Preiss JC, Loddenkemper C, Günther U, Somasundaram R, Siegmund B, Zeitz M. [Nodular regenerative hyperplasia as a side effect of azathioprine in a patient with Crohn's disease]. Dtsch Med Wochenschr. 2008;133:1897-1900. |
| 73. | Ansari A, Elliott T, Fong F, Arenas-Hernandez M, Rottenberg G, Portmann B, Lucas S, Marinaki A, Sanderson J. Further experience with the use of 6-thioguanine in patients with Crohn's disease. Inflamm Bowel Dis. 2008;14:1399-1405. |
| 74. | Ehmsen L, Marko C, Breidert M. [Portal vein hypertension during azathioprine therapy in patients with Crohn's disease--a frequent phenomenon?]. Dtsch Med Wochenschr. 2008;133:950-953. |
| 75. | Arnott ID, Ghosh S. Portal hypertension in the presence of minimal liver damage in Crohn's disease on long-term azathioprine: possible endothelial cell injury. Eur J Gastroenterol Hepatol. 2000;12:569-573. |
| 76. | Tinsa F, Brini I, El May A, Bousnina D, Boussetta K, Bousnina S. Nodular regenerative hyperplasia of the liver, celiac disease and Sjogren's syndrome in a child. Gastroenterol Clin Biol. 2010;34:40-42. |
| 77. | Biecker E, Trebicka J, Fischer HP, Sauerbruch T, Lammert F. Portal hypertension and nodular regenerative hyperplasia in a patient with celiac disease. Z Gastroenterol. 2006;44:395-398. |
| 78. | Cancado EL, Medeiros DM, Deguti MM, Dos Santos MS, de Mello ES, Vendramini MB, Carrilho FJ. Celiac disease associated with nodular regenerative hyperplasia, pulmonary abnormalities, and IgA anticardiolipin antibodies. J Clin Gastroenterol. 2006;40:135-139. |
| 79. | Austin A, Campbell E, Lane P, Elias E. Nodular regenerative hyperplasia of the liver and coeliac disease: potential role of IgA anticardiolipin antibody. Gut. 2004;53:1032-1034. |
| 80. | Riestra S, Domínguez F, Rodrigo L. Nodular regenerative hyperplasia of the liver in a patient with celiac disease. J Clin Gastroenterol. 2001;33:323-326. |
| 81. | Agard C, Ponge T, Mahé B, Barrier J. [Lymphocytic lymphoma and regenerative liver nodular hyperplasia in systemic scleroderma]. Rev Med Interne. 2000;21:301-303. |
| 82. | McMahon RF, Babbs C, Warnes TW. Nodular regenerative hyperplasia of the liver, CREST syndrome and primary biliary cirrhosis: an overlap syndrome? Gut. 1989;30:1430-1433. |
| 83. | García Díaz JD, Praga Terente M, Colina Ruizdelgado F, Lizasoaín Hernández M, Mesa Latorre J. [Nodular regenerative hyperplasia of the liver associated with a CREST syndrome with multiorgan involvement]. An Med Interna. 1989;6:203-206. |
| 84. | Cadranel JF, Grippon P, Wechsler B, Bidegaray E, Karkouche B, Opolon P. [The CRST syndrome and nodular regenerative hyperplasia of the liver. A case]. Presse Med. 1987;16:1656. |
| 85. | Friguet JL, Deugnier Y, Messner M, Lauvin R, Launois B, Brissot P, Ferrand B, Bourel M. [Regenerative nodular hyperplasia in scleroderma : a new case]. Gastroenterol Clin Biol. 1984;8:979. |
| 86. | Gaya DR, Oien KA, Stanley AJ, Morris AJ. Bleeding gastric varices and antiphospholipid syndrome. Nat Clin Pract Gastroenterol Hepatol. 2005;2:156-159; quiz 1 p following 159. |
| 87. | Morlà RM, Ramos-Casals M, García-Carrasco M, Cervera R, Font J, Bruguera M, Rojas-Rodríguez J, Ingelmo M. Nodular regenerative hyperplasia of the liver and antiphospholipid antibodies: report of two cases and review of the literature. Lupus. 1999;8:160-163. |
| 88. | Cadranel JF, Demontis R, Guettier C, Bouraya D, Dautreaux M, Ghazali A, Poux JM, Coutarel P, Devergie B, Fievet P. [Nodular regenerative hyperplasia associated with primary antiphospholipid syndrome]. Gastroenterol Clin Biol. 1996;20:901-904. |
| 89. | Keegan AD, Brooks LT, Painter DM. Hepatic infarction and nodular regenerative hyperplasia of the liver with associated anticardiolipin antibodies in a young woman. J Clin Gastroenterol. 1994;18:309-313. |
| 90. | Devaney K, Goodman ZD, Epstein MS, Zimmerman HJ, Ishak KG. Hepatic sarcoidosis. Clinicopathologic features in 100 patients. Am J Surg Pathol. 1993;17:1272-1280. |
| 91. | Toso C, Isse K, Demetris AJ, Dinyari P, Koh A, Imes S, Kin T, Emamaullee J, Senior P, Shapiro AM. Histologic graft assessment after clinical islet transplantation. Transplantation. 2009;88:1286-1293. |
| 92. | Pezzullo L, Muretto P, De Rosa G, Picardi M, Lucania A, Rotoli B. Liver nodular regenerative hyperplasia after bone marrow transplant. Haematologica. 2000;85:669-670. |
| 93. | Ichikawa Y, Kyo M, Hanafusa T, Kohro T, Kishikawa H, Fukunishi T, Nagano S, Shinji Y. A 20-year case study of a kidney transplant recipient with chronic active hepatitis C: clinical course and successful treatment for late acute rejection induced by interferon therapy. Transplantation. 1998;65:134-138. |
| 94. | Sebagh M, Farges O, Samuel D, Bismuth H, Reynès M. Nodular regenerative hyperplasia of the liver following orthotopic liver transplantation. Transplant Proc. 1995;27:2510-2511. |
| 95. | Xerri L, Payan MJ, Choux R, Gros N, Hassoun J, Chamlian A, Blin D, Monties JR. An exceptional 18-year follow-up after cardiac transplantation. How can malignancies occur during immunosuppressive therapy? Cancer. 1989;63:1697-1699. |
| 96. | Jones MC, Best PV, Catto GR. Is nodular regenerative hyperplasia of the liver associated with azathioprine therapy after renal transplantation? Nephrol Dial Transplant. 1988;3:331-333. |
| 97. | Buffet C, Cantarovitch M, Pelletier G, Fabre M, Martin E, Charpentier B, Etienne JP, Fries D. Three cases of nodular regenerative hyperplasia of the liver following renal transplantation. Nephrol Dial Transplant. 1988;3:327-330. |
| 98. | Morales JM, Prieto C, Colina F, Mestre MJ, Lopez I, Perez-Sola A, Solis Herruzo JA, Ruilope LM, Rodicio JL. Nodular regenerative hyperplasia of the liver in renal transplantation. Transplant Proc. 1987;19:3694-3696. |
| 99. | Bredfeldt JE, Havey AL. Nodular regenerative hyperplasia of the liver following renal transplantation. Dig Dis Sci. 1981;26:271-274. |
| 100. | van den Broek MA, Olde Damink SW, Driessen A, Dejong CH, Bemelmans MH. Nodular regenerative hyperplasia secondary to neoadjuvant chemotherapy for colorectal liver metastases. Case Report Med. 2009;2009:457975. |
| 101. | Citak EC, Karadeniz C, Oguz A, Boyunaga O, Ekinci O, Okur V. Nodular regenerative hyperplasia and focal nodular hyperplasia of the liver mimicking hepatic metastasis in children with solid tumors and a review of literature. Pediatr Hematol Oncol. 2007;24:281-289. |
| 102. | Chu WC, Roebuck DJ. Nodular regenerative hyperplasia of the liver simulating metastases following treatment for bilateral Wilms tumor. Med Pediatr Oncol. 2003;41:85-87. |
| 103. | Minato H, Nakanuma Y. Nodular regenerative hyperplasia of the liver associated with metastases of pancreatic endocrine tumour: report of two autopsy cases. Virchows Arch A Pathol Anat Histopathol. 1992;421:171-174. |
| 104. | Cervera R, Abós J, Bruguera M, Grau JM. [Regenerative nodular hepatic hyperplasia and gastric carcinoma]. Rev Clin Esp. 1987;181:341-342. |
| 105. | Kataoka TR, Tsukamoto Y, Kanazawa N, Izumi T, Awata N, Nishizawa Y, Ohsawa M, Ishiguro S. Concomitant hepatocellular carcinoma and non-Hodgkin's lymphoma in a patient with nodular regenerative hyperplasia. Pathol Int. 2006;56:279-282. |
| 106. | Kiyuna A, Sunagawa T, Hokama A, Touyama M, Tomiyama R, Sakugawa H, Kinjo F, Saito A. Nodular regenerative hyperplasia of the liver and Castleman's disease: potential role of interleukin-6. Dig Dis Sci. 2005;50:314-316. |
| 107. | Iwabe C, Hashimoto E, Aoka K, Watanabe U, Hayashi N. [A case of non-Hodgkin's lymphoma with portal hypertension and nodular regenerative hyperplasia]. Nippon Shokakibyo Gakkai Zasshi. 1994;91:2239-2243. |
| 108. | Feng WJ, Takayasu K, Konda C, Yamazaki S, Sakamoto M, Hirohashi S, Takenaka T. CT of nodular hyperplasia of the liver in non-Hodgkin lymphoma. J Comput Assist Tomogr. 1991;15:1031-1034. |
| 109. | Mesa Latorre J, de Dios García Díaz J, Larregla Garraus S, Ortiz Conde MC. [Nodular regenerative hyperplasia of the liver and acute lymphoblastic leukemia]. Rev Clin Esp. 1990;186:192-193. |
| 110. | Zuber M, Gherardi R, Defer G, Gaulard P, Divine M, Zafrani ES. Peripheral neuropathy, coagulopathy and nodular regenerative hyperplasia of the liver in a patient with multiple serologic auto-antibody activities and IgM B-cell lymphoma. J Intern Med. 1989;226:291-295. |
| 111. | Ramos Soria F, Puig Pujol X, Vida Mombiela F, Badal Alter JM. [Hemoperitoneum as the first manifestation of hepatic regenerative nodular hyperplasia associated with Hodgkin's lymphoma]. Rev Clin Esp. 1989;184:333. |
| 112. | Rozman M, Montserrat E, Bruguera M, Grau JM, Terés J, Rozman C. [Chronic lymphatic leukemia and portal hypertension: a causal association?]. Med Clin (Barc). 1989;92:26-28. |
| 113. | Kitazono M, Saito Y, Kinoshita M, Nakashima T, Kojiro M, Tanaka H. Nodular regenerative hyperplasia of the liver in a patient with multiple myeloma and systemic amyloidosis. Acta Pathol Jpn. 1985;35:961-967. |
| 114. | Voinchet O, Degott C, Scoazec JY, Feldmann G, Benhamou JP. Peliosis hepatis, nodular regenerative hyperplasia of the liver, and light-chain deposition in a patient with Waldenström's macroglobulinemia. Gastroenterology. 1988;95:482-486. |
| 115. | Wanless IR, Solt LC, Kortan P, Deck JH, Gardiner GW, Prokipchuk EJ. Nodular regenerative hyperplasia of the liver associated with macroglobulinemia. A clue to the pathogenesis. Am J Med. 1981;70:1203-1209. |
| 116. | García Buey L, García Sánchez A, Moreno Otero R, González Estecha A, Pozo A, Pajares JM. [Hepatic nodular regenerative hyperplasia associated with essential mixed cryoglobulinemia]. Rev Clin Esp. 1987;181:285-287. |
| 117. | Mignon F, Ronco P, Verroust P, Poupon R, Prud'homme de Saint-Maur P, Morel-Maroger L. [Nephropathy and nodular regenerative hyperplasia of the liver (author's transl)]. Nephrologie. 1980;1:23-26. |
| 118. | Carbone J, Escudero A, Mayayo M, Ballesteros M, Perez-Corral A, Sanchez-Ramon S, Sarmiento E, Micheloud D, Fernandez-Cruz E. Partial response to anti-CD20 monoclonal antibody treatment of severe immune thrombocytopenic purpura in a patient with common variable immunodeficiency. Ann N Y Acad Sci. 2005;1051:666-671. |
| 119. | Hilario Rodríguez E, Velasco Oses A, Coma y del Corral MJ, Sáenz García JA. [Diffuse nodular regenerative hyperplasia of the liver associated with autoimmune hemolytic anemia. Presentation of a case and review of the literature]. Rev Esp Enferm Apar Dig. 1983;63:45-51. |
| 120. | Castellano G, Colina F, Moreno D, Pinedo F, Canga F, Solís Herruzo JA. [Nodular regenerative hepatic hyperplasia associated with primary biliary cirrhosis]. Rev Clin Esp. 1992;191:433-434. |
| 121. | Buffet C, Sinico M, Adda G, Fabre M, Roge J, Pelletier G, Martin E, Etienne JP. [Nodular regenerative hyperplasia and primary biliary cirrhosis]. Gastroenterol Clin Biol. 1991;15:856-858. |
| 122. | Chazouillères O, Andreani T, Legendre C, Poupon R, Darnis F. [Nodular regenerative hyperplasia of the liver and primary biliary cirrhosis. A fortuitous association?]. Gastroenterol Clin Biol. 1986;10:764-766. |
| 123. | Mones JM, Saldana MJ, Albores-Saavedra J. Nodular regenerative hyperplasia of the liver. Report of three cases and review of the literature. Arch Pathol Lab Med. 1984;108:741-743. |
| 124. | Mones JM, Saldana MJ. Nodular regenerative hyperplasia of the liver in a 4-month-old infant. Am J Dis Child. 1984;138:79-81. |
| 125. | Grazioli L, Alberti D, Olivetti L, Rigamonti W, Codazzi F, Matricardi L, Fugazzola C, Chiesa A. Congenital absence of portal vein with nodular regenerative hyperplasia of the liver. Eur Radiol. 2000;10:820-825. |
| 126. | Arana E, Martí-Bonmatí L, Martínez V, Hoyos M, Montes H. Portal vein absence and nodular regenerative hyperplasia of the liver with giant inferior mesenteric vein. Abdom Imaging. 1997;22:506-508. |
| 127. | Buchel O, Roskams T, Van Damme B, Nevens F, Pirenne J, Fevery J. Nodular regenerative hyperplasia, portal vein thrombosis, and avascular hip necrosis due to hyperhomocysteinaemia. Gut. 2005;54:1021-1023. |
| 128. | Talbot-Smith A, Syn WK, MacQuillan G, Neil D, Elias E, Ryan P. Familial idiopathic pulmonary fibrosis in association with bone marrow hypoplasia and hepatic nodular regenerative hyperplasia: a new "trimorphic" syndrome. Thorax. 2009;64:440-443. |
| 129. | Haboubi NY, Smith VJ, Coyne JD, Ackrill P. Nodular regenerative hyperplasia of the liver in a non-treated patient with mesangiocapillary glomerulonephritis. Histopathology. 1991;18:367-368. |
| 130. | Haratake J, Horie A, Takasugi M, Hiroshige K. Nodular regenerative hyperplasia of the liver associated with idiopathic membranous glomerulonephritis. Am J Gastroenterol. 1987;82:677-680. |
| 131. | McCulloch AJ, Morley AR, Wilkinson R, Lesna M. Nodular regenerative hyperplasia of the liver with membranous glomerulonephritis. Postgrad Med J. 1981;57:402-403. |
| 132. | Fonseca V, Havard CW. Portal hypertension secondary to azathioprine in myasthenia gravis. Postgrad Med J. 1988;64:950-952. |
| 133. | Eliakim R, Ligumsky M, Jurim O, Shouval D. Nodular regenerative hyperplasia with portal hypertension in a patient with myasthenia gravis. Am J Gastroenterol. 1987;82:674-676. |
| 134. | Goritsas CP, Repanti M, Papadaki E, Lazarou N, Andonopoulos AP. Intrahepatic bile duct injury and nodular regenerative hyperplasia of the liver in a patient with polyarteritis nodosa. J Hepatol. 1997;26:727-730. |
| 135. | Nakanuma Y, Ohta G, Sasaki K. Nodular regenerative hyperplasia of the liver associated with polyarteritis nodosa. Arch Pathol Lab Med. 1984;108:133-135. |
| 136. | Sasaki M, Hodo Y, Nakanuma Y. Hepatocellular carcinoma arising in primary biliary cirrhosis presenting with nodular regenerative hyperplasia: report of an autopsy case. J Gastroenterol Hepatol. 2006;21:1866-1868. |
| 137. | Ravindran J, Gillis D, Rowland R, Heddle R. Common variable immunodeficiency associated with nodular regenerative hyperplasia of the liver. Aust N Z J Med. 1995;25:741. |
| 138. | Thevenot T, Dhote R, Tulliez M, Baverel F, Permal S, Rabineau D, Christoforov B. [Turner syndrome and nodular regenerative hyperplasia of the liver]. Ann Med Interne (Paris). 1998;149:295-296. |
| 139. | de Lédinghen V, Levillain P, Besson I, Palazzo L, Fabre M, Silvain C, Morichau-Beauchant M. [Nodular regenerative hyperplasia of the liver and Turner syndrome]. Gastroenterol Clin Biol. 1994;18:898-899. |
| 140. | Molina T, Delmer A, Le Tourneau A, Texier P, Degott C, Audoin J, Zittoun R, Diebold J. Hepatic lesions of vascular origin in multicentric Castleman's disease, plasma cell type: report of one case with peliosis hepatis and another with perisinusoidal fibrosis and nodular regenerative hyperplasia. Pathol Res Pract. 1995;191:1159-1164. |
| 141. | Nakamura Y, Takeuchi T, Kanaoka H, Okanoue T, Kashima K. [A case of nodular regenerative hyperplasia of liver with idiopathic hypereosinophilic syndrome]. Nippon Shokakibyo Gakkai Zasshi. 1997;94:44-48. |
| 142. | Baker BL, Axiotis C, Hurwitz ES, Leavitt R, Di Bisceglie AM. Nodular regenerative hyperplasia of the liver in idiopathic hypereosinophilic syndrome. J Clin Gastroenterol. 1991;13:452-456. |
| 143. | Morris JM, Oien KA, McMahon M, Forrest EH, Morris J, Stanley AJ, Campbell S. Nodular regenerative hyperplasia of the liver: survival and associated features in a UK case series. Eur J Gastroenterol Hepatol. 2010;22:1001-1005. |
| 144. | Wang HM, Lo GH, Hsu PI, Lin CK, Chan HH, Chen WC, Lai KH, Wang BW, Lin SL. Nodular regenerative hyperplasia of the liver. J Chin Med Assoc. 2008;71:523-527. |
| 145. | Ziol M, Poirel H, Kountchou GN, Boyer O, Mohand D, Mouthon L, Tepper M, Guillet JG, Guettier C, Raphael M. Intrasinusoidal cytotoxic CD8+ T cells in nodular regenerative hyperplasia of the liver. Hum Pathol. 2004;35:1241-1251. |
| 146. | Al-Mukhaizeem KA, Rosenberg A, Sherker AH. Nodular regenerative hyperplasia of the liver: an under-recognized cause of portal hypertension in hematological disorders. Am J Hematol. 2004;75:225-230. |
| 147. | Ferlitsch A, Teml A, Reinisch W, Ulbrich G, Wrba F, Homoncik M, Gangl A, Peck-Radosavljevic M, Vogelsang H. 6-thioguanine associated nodular regenerative hyperplasia in patients with inflammatory bowel disease may induce portal hypertension. Am J Gastroenterol. 2007;102:2495-2503. |
| 148. | Ueno S, Tanabe G, Sueyoshi K, Yoshinaka H, Yamamoto S, Kurita K, Yoshidome S, Nuruki K, Aikou T. Hepatic hemodynamics in a patient with nodular regenerative hyperplasia. Am J Gastroenterol. 1996;91:1012-1015. |
| 149. | Clouet M, Boulay I, Boudiaf M, Soyer P, Nemeth J, Kiselman R, Rymer R. Imaging features of nodular regenerative hyperplasia of the liver mimicking hepatic metastases. Abdom Imaging. 1999;24:258-261. |
| 150. | Casillas C, Martí-Bonmatí L, Galant J. Pseudotumoral presentation of nodular regenerative hyperplasia of the liver: imaging in five patients including MR imaging. Eur Radiol. 1997;7:654-658. |
| 151. | Rha SE, Lee MG, Lee YS, Kang GH, Ha HK, Kim PN, Auh YH. Nodular regenerative hyperplasia of the liver in Budd-Chiari syndrome: CT and MR features. Abdom Imaging. 2000;25:255-258. |
| 152. | Zech CJ, Seiderer J, Reinisch W, Ochsenkuhn T, Schima W, Diebold J, Wrba F, Reiser MF, Schoenberg SO. Thioguanin-induced nodular regenerative hyperplasia of the liver-ROC analysis of different MR techniques. Eur Radiol. 2007;17:1898-1905. |
| 153. | Laharie D, Vergniol J, Bioulac-Sage P, Diris B, Poli J, Foucher J, Couzigou P, Drouillard J, de Lédinghen V. Usefulness of noninvasive tests in nodular regenerative hyperplasia of the liver. Eur J Gastroenterol Hepatol. 2010;22:487-493. |
| 154. | Ames JT, Federle MP, Chopra K. Distinguishing clinical and imaging features of nodular regenerative hyperplasia and large regenerative nodules of the liver. Clin Radiol. 2009;64:1190-1195. |
| 155. | Dachman AH, Ros PR, Goodman ZD, Olmsted WW, Ishak KG. Nodular regenerative hyperplasia of the liver: clinical and radiologic observations. AJR Am J Roentgenol. 1987;148:717-722. |
| 156. | Ibarrola C, Colina F. Clinicopathological features of nine cases of non-cirrhotic portal hypertension: current definitions and criteria are inadequate. Histopathology. 2003;42:251-264. |
| 157. | Arvanitaki M, Adler M. Nodular regenerative hyperplasia of the liver. A review of 14 cases. Hepatogastroenterology. 2001;48:1425-1429. |
| 158. | Seiderer J, Zech CJ, Diebold J, Schoenberg SO, Brand S, Tillack C, Göke B, Ochsenkühn T. Nodular regenerative hyperplasia: a reversible entity associated with azathioprine therapy. Eur J Gastroenterol Hepatol. 2006;18:553-555. |
| 159. | Krishna M, Keaveny AP, Genco PV, Rosser BG, Dickson RC, Nguyen JH, Steers JL, Nakhleh RE. Clinicopathological review of 18 cases of liver allografts lost due to bile duct necrosis. Transplant Proc. 2005;37:2221-2223. |
| 160. | Radomski JS, Chojnacki KA, Moritz MJ, Rubin R, Armenti VT, Wilson GA, Herrine S, Conn M. Results of liver transplantation for nodular regenerative hyperplasia. Am Surg. 2000;66:1067-1070. |
| 161. | Loinaz C, Colina F, Musella M, Lopez-Rios F, Gomez R, Jimenez C, Gonzalez Pinto I, Garcia I, Moreno Gonzalez E. Orthotopic liver transplantation in 4 patients with portal hypertension and non-cirrhotic nodular liver. Hepatogastroenterology. 1998;45:1787-1794. |
| 162. | Dumortier J, Bizollon T, Scoazec JY, Chevallier M, Bancel B, Berger F, Ducerf C, Claudel-Bonvoisin S, Paliard P, Boillot O. Orthotopic liver transplantation for idiopathic portal hypertension: indications and outcome. Scand J Gastroenterol. 2001;36:417-422. |
| 163. | Nzeako UC, Goodman ZD, Ishak KG. Hepatocellular carcinoma and nodular regenerative hyperplasia: possible pathogenetic relationship. Am J Gastroenterol. 1996;91:879-884. |
| 164. | Kobayashi S, Saito K, Nakanuma Y. Nodular regenerative hyperplasia of the liver in hepatocellular carcinoma. An autopsy study. J Clin Gastroenterol. 1993;16:155-159. |
| 165. | Stromeyer FW, Ishak KG. Nodular transformation (nodular "regenerative" hyperplasia) of the liver. A clinicopathologic study of 30 cases. Hum Pathol. 1981;12:60-71. |
| 166. | Russmann S, Zimmermann A, Krähenbühl S, Kern B, Reichen J. Veno-occlusive disease, nodular regenerative hyperplasia and hepatocellular carcinoma after azathioprine treatment in a patient with ulcerative colitis. Eur J Gastroenterol Hepatol. 2001;13:287-290. |
| 167. | Thung SN, Gerber MA. Enzyme pattern and marker antigens in nodular "regenerative" hyperplasia of the liver. Cancer. 1981;47:1796-1799. |
| 168. | Di Gioia S, Bianchi P, Destro A, Grizzi F, Malesci A, Laghi L, Levrero M, Morabito A, Roncalli M. Quantitative evaluation of RASSF1A methylation in the non-lesional, regenerative and neoplastic liver. BMC Cancer. 2006;6:89. |
| 169. | Pewzner-Jung Y, Brenner O, Braun S, Laviad EL, Ben-Dor S, Feldmesser E, Horn-Saban S, Amann-Zalcenstein D, Raanan C, Berkutzki T. A critical role for ceramide synthase 2 in liver homeostasis: II. insights into molecular changes leading to hepatopathy. J Biol Chem. 2010;285:10911-10923. |