Published online Feb 28, 2010. doi: 10.3748/wjg.v16.i8.1003
Revised: October 26, 2009
Accepted: November 2, 2009
Published online: February 28, 2010
AIM: To study characteristics of collateral circulation of gastric varices (GVs) with 64-row multidetector computer tomography portal venography (MDCTPV).
METHODS: 64-row MDCTPV with a slice thickness of 0.625 mm and a scanning field from 2 cm above the tracheal bifurcation to the lower edge of the kidney was performed in 86 patients with GVS diagnosed by endoscopy. The computed tomography protocol included unenhanced, arterial and portal vein phases. The MDCTPV was performed on an AW4.3 workstation. GVs were classified into three types according to Sarin’s Classification. The afferent and efferent veins of each type of GV were observed.
RESULTS: The afferent venous drainage originated mostly from the left gastric vein alone (LGV) (28/86, 32.59%), or the LGV more than the posterior gastric vein/short gastric vein [LGV > posterior gastric vein/short gastric vein (PGV/SGV)] (22/86, 25.58%), as seen by MDCTPV. The most common efferent venous drainage was via the azygos vein to the superior vena cava (53/86, 61.63%), or via the gastric/splenorenal shunt (37/86, 43.02%) or inferior phrenic vein (8/86, 9.30%) to the inferior vena cava. In patients with gastroesophageal varices type 1, the afferent venous drainage of GV mainly originated from the LGV or LGV > PGV/SGV (43/48, 89.58%), and the efferent venous drainage was mainly via the azygos vein to the super vena cava (43/48, 89.58%), as well as via the gastric/splenorenal shunt (8/48, 16.67%) or inferior phrenic vein (3/48, 6.25%) to the inferior vena cava. In patients with gastroesophageal varices type 2, the afferent venous drainage of the GV mostly came from the PGV/SGV more than the LGV (PGV/SGV > LGV) (8/16, 50%), and the efferent venous drainage was via the azygos vein (10/16, 62.50%) and gastric/splenorenal shunt (9/16, 56.25%). In patients with isolated gastric varices, the main afferent venous drainage was via the PGV/SGV alone (16/22, 72.73%), and the efferent venous drainage was mainly via the gastric/splenorenal shunt (20/22, 90.91%), as well as the inferior phrenic vein (3/23) to the inferior vena cava.
CONCLUSION: MDCTPV can clearly display the afferent and efferent veins of all types of GV, and it could provide useful reference information for the clinical management of GV bleeding.
- Citation: Zhao LQ, He W, Ji M, Liu P, Li P. 64-row multidetector computed tomography portal venography of gastric variceal collateral circulation. World J Gastroenterol 2010; 16(8): 1003-1007
- URL: https://www.wjgnet.com/1007-9327/full/v16/i8/1003.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i8.1003
Liver cirrhosis can result in portal hypertension. Gastric fundic and/or esophageal varices are one of the severe complications. It may cause massive hemorrhage of the upper gastrointestinal tract[1]. The clinical management of gastric varices (GV) is related to their hemodynamics and locations. GV were classified into three types according to Sarin’s Classification that is based on varices location by endoscopy[2]. It is essential to identify the hemodynamics of different types of GV before treatment. The conventional portal vein catheterization provides useful information regarding portal hemodynamics including GV, but it is an invasive method[3]. As an almost atraumatic method, computed tomography angiography has been adopted widely to display the portal vein system[4-7]. Multidetector computer tomography portal venography (MDCTPV) can display esophageal varices (EV), GV and related bypass circuits more specifically because of the thinner slice and better spatial resolution of the computed tomography scanner[8,9]. In our study, 86 GV patients diagnosed by endoscopy were selected and classified into three types according to Sarin’s Classification[2], and the afferent and efferent veins of different types of GV were studied by MDCTPV.
Eighty-six consecutive patients with portal hypertension confirmed by endoscopy were enrolled in this study from April 2007 to December 2008, including 52 men and 34 women, aged 38-76 years (mean: 62.6 years). The etiology of portal hypertension for these 86 patients was post-hepatitic cirrhosis (n = 45), alcoholic cirrhosis (n = 23), primary biliary cirrhosis (n = 7), autoimmune hepatic cirrhosis (n = 3), cryptogenic cirrhosis (n = 1), pancreatic carcinoma (n = 4) and chronic pancreatitis (n = 3). There were 35 patients with a coexistent diagnosis of hepatoma. According to Child-Pugh grading, 15 cases were grade A, 50 grade B and 21 grade C.
A GE 64-row MDCT scanner was applied to perform non-enhanced, arterial and portal vein phase vein enhanced scans in all patients. The scanning range was from 2 cm above the tracheal bifurcation to the lower edge of the kidney. One hundred milliliters of non-ionic contrast medium (Omnipaque 350, Nycomed Inc., Princeton, NJ, USA) was injected with a power injector at a rate of 4.0 mL/s. The arterial phase scanning started about 20-30 s after the beginning of injection, and portal phase scanning was initiated 25 s after the beginning of the arterial phase. The reconstitution thickness was set at 0.625 mm.
Fujinon EG 485 (Fujinon, Saitama, Japan) and OlymPus CV240 electronic endoscope (Olympus Optical Co. Ltd., Tokyo, Japan) were used for the observation of EV and GV. The location of the varices was recorded according to endoscopic reports and imaging data.
CTPV images were processed on a GE AW4.3 workstation (GE Medical Systems, Milwaukee, WI, USA). GV and collateral circulation in all cases were analyzed using maximum-intensity projection (MIP) and multi-planner reformation (MPR) techniques. All images were reviewed by three independent experienced radiologists, who were blind to the patients’ clinical data. A consecutive conclusion was obtained if their dignosis was different.
According to the varices location under endoscopy[2], GVs were classified into three types: (1) gastroesophageal varices type 1 (GEV1): EV combined with lesser curve GV; (2) gastroesophageal varices type 2 (GEV2): EV combined with GV that extend to the greater curvature; and (3) isolated gastric varices (IGV): varices located on the body and fundus of the stomach, without EV.
Based on CTPV, the afferent venous drainage of GV could be divided into four types[10,11]: left gastric vein (LGV) alone; posterior gastric vein/short gastric vein (PGV/SGV) alone; LGV dominant (LGV > PGV/SGV; drainage from both the LGV and PGV/SGV, with the former predominating); and PGV/SGV dominant (PGV/SGV > LGV; drainage from both the LGV and PGV/SGV, with the latter predominating).
According to endoscopy, we found 48 cases of GEV1 (55.8%), 16 of GEV2 (18.6%) and 22 of IGV (25.6%) (Table 1).
| GEV1 | GEV2 | IGV | Total | |
| Afferent vein of GV | ||||
| LGV | 27 | 1 | 0 | 28 |
| LGV > PGV/SGV | 16 | 3 | 1 | 22 |
| PGV/SGV > LGV | 3 | 8 | 5 | 16 |
| PGV/SGV | 2 | 4 | 16 | 20 |
| Efferent vein of GV | ||||
| Azygos vein | 43 | 10 | 0 | 53 |
| Inferior phrenic vein | 3 | 2 | 3 | 8 |
| Gastric/splenorenal shunt | 8 | 9 | 20 | 37 |
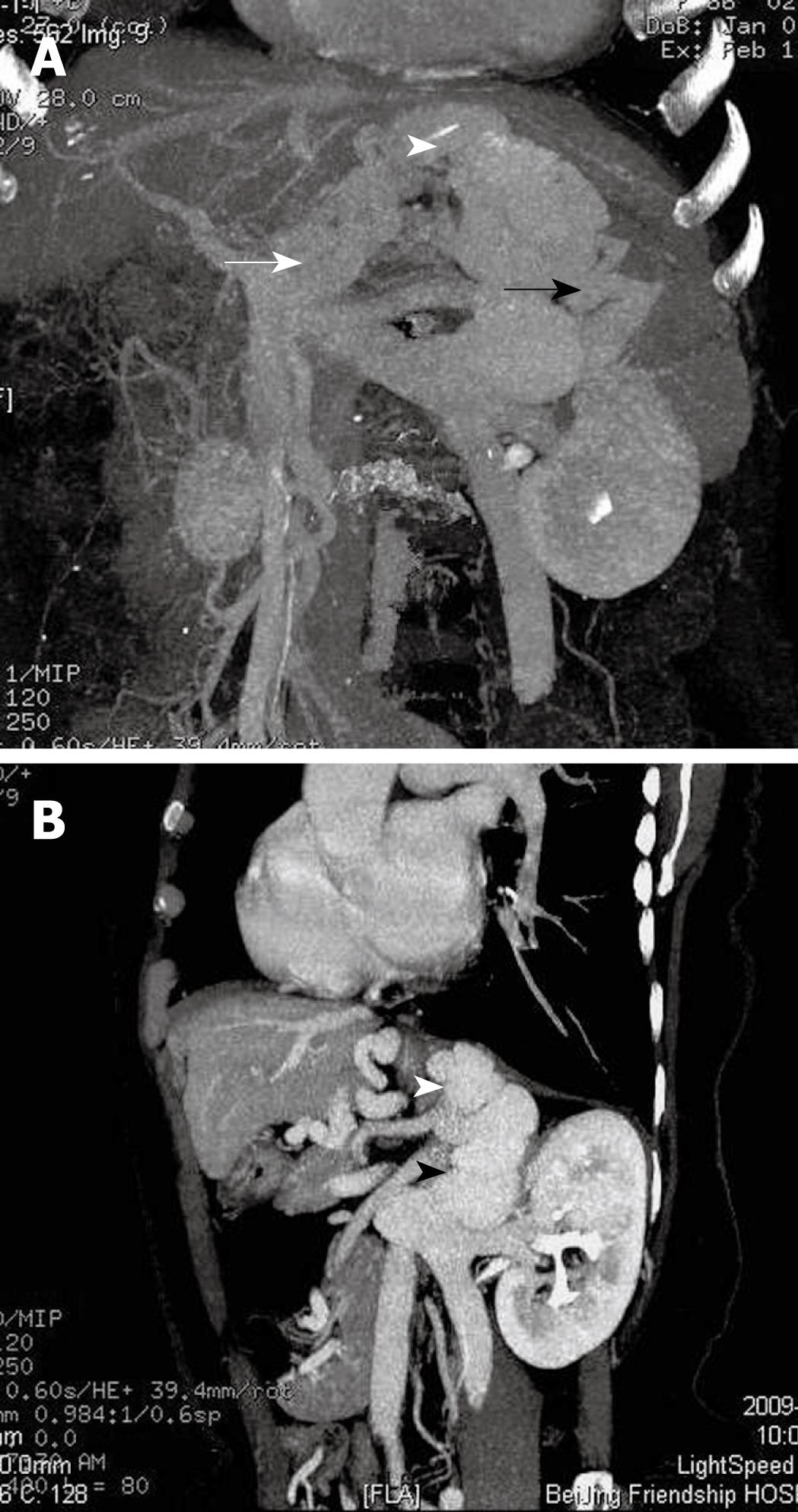
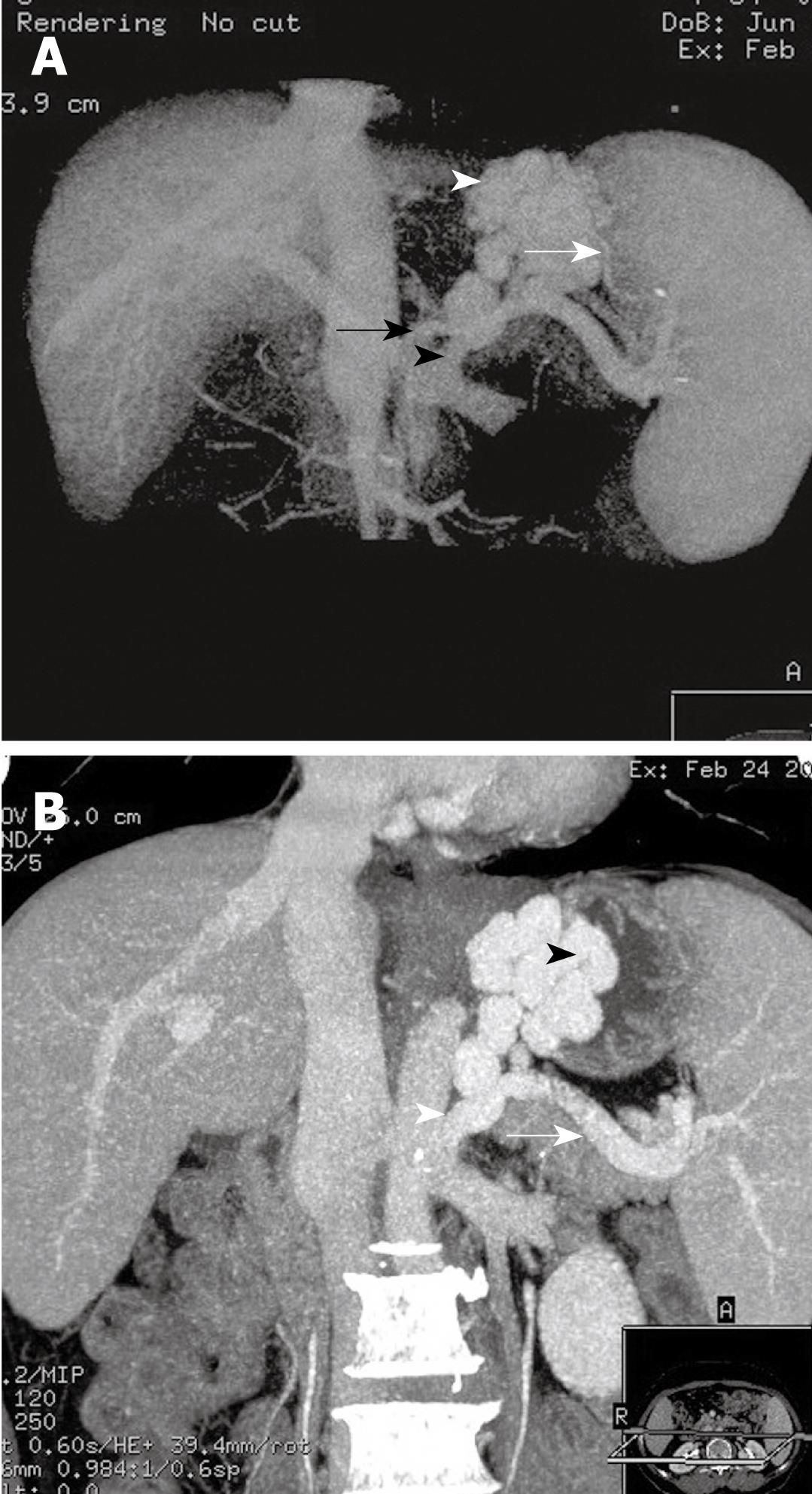
MDCTPV showed that the afferent venous drainage of GV (Table 1) originated from LGV (28/86, 32. 59%), PGV/SGV > LGV (22/86, 25.58%), followed by PGV/SGV (20/86, 23.26%) and PGV/SGV > LGV (16/86, 18.60%). Among the GEV1 type, the afferent vein of the GV mostly originated from the LGV (27/48, 56.25%) (Figure 1A) or LGV > PGV/SGV (16/48, 33.33%). Most cases of GEV2 type originated from PGV/SGV > LGV (8/16, 50%) (Figure 2A) or PGV/SGV (4/16, 25.00%), and then LGV > PGV/SGV (3/16, 18.75%). Most IGV cases originated from PGV/SGV (16/22, 72.73%) (Figure 3A and B) or PGV/SGV > LGV (5/22, 22.73%).
The efferent venous drainage of GV differed between patients, and several drainage veins might be observed in one patient as well (Table 1). In 53 cases, the efferent venous drainage was from the azygos vein to the superior vena cava (53/86, 61.63%); eight cases from the inferior phrenic vein to the inferior vena cava (8/86, 9.30%); and 37 cases from the gastric/splenorenal shunt to the inferior vena cava (G/S-R) (37/86, 43.02%). The main efferent venous drainage of GEV1 was via the azygos vein into the superior vena cava (43/48, 89.58%) (Figure 1B), whereas the efferent drainage of GEV2 was mostly via the azygos vein (10/16, 62.5%) to the superior vena cava, and via the gastric/splenorenal shunt to the inferior vena cava (9/16, 56.25%) (Figure 2B). The efferent venous drainage of IGV was mainly via the gastric/splenorenal shunt to the inferior vena cava (20/22, 90.91%) ( Figure 3A and B).
GV are an ominous consequence of portal hypertension[9]. Sarin and Ryan have reported that GV are detected in 20% of portal hypertension patients[12,13]. Compared to endoscopic findings reported by Sarin et al[12], our study with CTPV revealed that the IGV type was more common (25.6%), GEV1 was less common (55.8%) and GEV2 was similar to that report. It was probably because there were more cases of pancreas disease in our study[14].
The afferent venous drainage of GV was mainly from three blood supplies: LGV, PGV and SGV. We showed that the afferent venous drainage of GV in GEV1 mostly originated from the LGV or LGV > PGV/SGV. In GEV2, LGV and PGV/SGV participated in the blood supply of GV. As for type IGV, the afferent venous drainage was mainly from the PGV/SGV. Our study revealed that PGV/SGV participated in the blood supply of the three types of GV, which was more than in the former study[10]. This may be because more cases of pancreatic cancer and pancreatitis were involved in this study. The latter was called left-sided portal hypertension, because the pancreas diseases involved the splenic vein, which showed PGV/SGV leading to GV, and often not accompanied by EV[15,16].
The blood supply pattern of GV is related closely to the anatomy of the LGV, PGV and SGV. The LGV originates from the portal vein, splenic vein and portosplenic angle. The stem of the LGV gives off anterior and posterior branches above the body of stomach. The anterior branch enters the wall of the fundus and forms the varices, which are continuous with the peri-esophageal varices in the esophagogastric junction. The posterior branch, from which the paraesophageal varices are formed directly, collects blood from the lesser curvature, cardia and lower segment of the esophagus[17]. As a result, when the LGV is predominant (GEV1), the location of GV is closer to the cardia, and generally accompanied by EV. The PGV is not present in normal conditions; it only emerges when portal hypertension occurs. It originates from the splenic vein and collects blood from the greater gastric curvature. As a result, in GEV2 and IGV patients, the PGV is one of the main blood vessels. This is the same as reported by Watanabe et al[3] through portal vein catheterization. In GEV1, the PGV is part of the GV blood supply. The SGV originates from the splenic vein and mainly drains blood from the fundus and greater curvature, thus contributing mainly to the fundus varices.
The para-esophageal varices may connect with the peri-esophageal varices, or join the superior vena cava via the azygos vein system, or via the inferior phrenic vein to the inferior vena cava[18]. Therefore, venous drainage of GEV1 is mostly via the azygos vein to the superior vena cava. EV can also exist in GEV2, but the GV blood supply seldom comes from the LGV, thus, in GEV2, only a small part of the GV drainage goes via the azygos vein to the superior vena cava or via the inferior phrenic vein to the inferior vena cava.
The gastric/splenorenal shunt is the spontaneous portosystemic shunt that runs from the branches of the PGV/SGV via the left adrenal vein, retroperitoneal veins and other branches of the left renal vein[8,19]. Thus it is likely to be found in GEV2 and IGV, as indicated in our study.
The CTPV view of the blood supply and drainage of GV could provide clinicians with a valuable reference for the endoscopic treatment of GV bleeding[20,21]. GV collateral vessels should be given special attention during treatment. GEV2 and IGV are supplied by multiple vessels, therefore, the simple treatment of endoscopic variceal ligation is not ideal, and has a high rate of recurrence and postoperative hemorrhage. With regard to the gastric/splenorenal shunt that is commonly found with IGV, more attention should be paid to the dosage and injection rate of sclerosant during endoscopic sclerotherapy, so as to prevent the sclerosant from flowing into the systemtic circulation via the shunt[22]. In some GEV1 cases, the incidence of secondary GV increases after treatment of EV[11]. On the other hand, after treatment of GV, EV are aggravated because of the special drainage pattern, which can be displayed clearly on CTPV[18]. Therefore, CTPV has its value in the follow-up after endoscopic sclerotherapy.
The collateral circulation, location, and hemodynamics of gastric varices (GV) can affect the treatment of GV bleeding.
Computed tomography angiography has been used widely to visualize the portal vein system, and it can reveal esophageal varices, GV and related bypass circuits.
In this study, the afferent and efferent veins of different types of GV, which were classified according to their location, were revealed by the high spatial resolution imaging of multidetector computed tomography (MDCT) and the appropriate post-processing methods.
As a noninvasive method, MDCT portal venography could provide clinicians with a valuable reference in the endoscopic and surgical treatment of GV bleeding.
This seems a very interesting new semiological approach to GV.
Peer reviewer: Heitor Rosa, Professor, Department of Gastroenterology and Hepatology, Federal University School of Medicine, Rua 126 n.21, Goiania - GO 74093-080, Brazil
S- Editor Cheng JX L- Editor Kerr C E- Editor Lin YP
| 1. | Bhasin DK, Malhi NJ. Variceal bleeding and portal hypertension: much to learn, much to explore. Endoscopy. 2002;34:119-128. |
| 2. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. |
| 3. | Watanabe K, Kimura K, Matsutani S, Ohto M, Okuda K. Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988;95:434-440. |
| 4. | Matsumoto A, Sugano Y, Yasuda M, Takimoto K. Role of multi-detector row CT angiography in the management of gastric fundal varices. Gut. 2004;53:467; author reply 467. |
| 5. | Zhu H, Shi B, Upadhyaya M, Wu Z, Lin X, Wu Y, Chen K. Therapeutic endoscopy of localized gastric varices: pretherapy screening and posttreatment evaluation with MDCT portography. Abdom Imaging. 2010;35:15-22. |
| 6. | Willmann JK, Weishaupt D, Böhm T, Pfammatter T, Seifert B, Marincek B, Bauerfeind P. Detection of submucosal gastric fundal varices with multi-detector row CT angiography. Gut. 2003;52:886-892. |
| 7. | Ishikawa T, Ushiki T, Mizuno K, Togashi T, Watanabe K, Seki K, Ohta H, Yoshida T, Takeda K, Kamimura T. CT-maximum intensity projection is a clinically useful modality for the detection of gastric varices. World J Gastroenterol. 2005;11:7515-7519. |
| 8. | Agarwal A, Jain M. Multidetector CT portal venography in evaluation of portosystemic collateral vessels. J Med Imaging Radiat Oncol. 2008;52:4-9. |
| 9. | Chen TW, Yang ZG, Li X, Wang QL, Qian LL, Wang RR. Evaluation of entire gastric fundic and esophageal varices secondary to posthepatitic cirrhosis: portal venography using 64-row MDCT. Abdom Imaging. 2010;35:1-7. |
| 10. | Zhao LQ, He W, Zhao H, Yu YZ. The value of CTportal venography in the diagnosis of collateral veins in patients with gastric varices. Zhonghua Fangshexue Zazhi. 2006;40:1175-1178. |
| 11. | Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc. 1990;36:276-280. |
| 12. | Sarin SK, Lahoti D. Management of gastric varices. Baillieres Clin Gastroenterol. 1992;6:527-548. |
| 13. | Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175-1189. |
| 14. | Liu QD, Zhou NX, Zhang WZ, Wang MQ. Diagnosis and management of regional portal hypertension. Chin J Dig Dis. 2005;6:87-92. |
| 15. | Heider TR, Azeem S, Galanko JA, Behrns KE. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239:876-880; discussion 880-882. |
| 16. | Weber SM, Rikkers LF. Splenic vein thrombosis and gastrointestinal bleeding in chronic pancreatitis. World J Surg. 2003;27:1271-1274. |
| 17. | Hino S, Kakutani H, Ikeda K, Uchiyama Y, Sumiyama K, Kuramochi A, Kitamura Y, Matsuda K, Arakawa H, Kawamura M. Hemodynamic assessment of the left gastric vein in patients with esophageal varices with color Doppler EUS: factors affecting development of esophageal varices. Gastrointest Endosc. 2002;55:512-517. |
| 18. | Zhao LQ, He W, Chen G. Characteristics of paraesophageal varices: a study with 64-row multidetector computed tomography portal venography. World J Gastroenterol. 2008;14:5331-5335. |
| 19. | Henseler KP, Pozniak MA, Lee FT Jr, Winter TC 3rd. Three-dimensional CT angiography of spontaneous portosystemic shunts. Radiographics. 2001;21:691-704. |
| 20. | Matsumoto A, Kitamoto M, Imamura M, Nakanishi T, Ono C, Ito K, Kajiyama G. Three-dimensional portography using multislice helical CT is clinically useful for management of gastric fundic varices. AJR Am J Roentgenol. 2001;176:899-905. |
| 21. | Shi B, Wu W, Zhu H, Wu YL. Successful endoscopic sclerotherapy for bleeding gastric varices with combined cyanoacrylate and aethoxysklerol. World J Gastroenterol. 2008;14:3598-3601. |
| 22. | Zhao H, Yu YZ, Zhao LQ, He W, Yu ZL. Clinical and hemodynamic features of gastric varices. Zhonghua Xiaohua Neijing Zazhi. 2006;23:241-244. |