Published online Feb 14, 2010. doi: 10.3748/wjg.v16.i6.723
Revised: December 3, 2009
Accepted: December 10, 2009
Published online: February 14, 2010
AIM: To make a retrospective analysis of endoscopy findings and clinicopathologic characteristics of colonic schistosomiasis in order to further improve our understanding of the disease and decrease its misdiagnosis.
METHODS: Endoscopy findings and clinicopathologic characteristics of 46 intestinal schistosomiasis patients were retrospectively analyzed. All the patients underwent colonoscopy and all biopsy specimens stained with hematoxylin and eosin were observed under a light microscope.
RESULTS: Of the 46 colonic schistosomiasis patients, 1 was diagnosed as acute schistosomal colitis, 16 as chronic schistosomal colitis and 29 as chronic active schistosomal colitis according to their endoscopic findings and pathology. Not all patients were suspected of or diagnosed as colonic schistosomiasis. Of the 12 misdiagnosed patients, 4 were misdiagnosed as ulcerative colitis, 1 as Crohn’s disease, and 7 as ischemic colitis. The segments of rectum and sigmoid colon were involved in 29 patients (63.0%). Intact Schistosoma ova were deposited in colonic mucosa accompanying infiltration of eosinocytes, lymphocytes, and plasma cells in acute schistosomal colitis patients. Submucosal fibrosis was found in chronic schistosomal colitis patients. Among the 17 patients with a signal polyp, hyperplastic polyp, canalicular adenoma with a low-grade intraepithelial neoplastic change, tubulovillous adenoma with a high-grade intraepithelial neoplastic change were observed in 10, 5, and 2 patients, respectively. Eight out of the 46 patients were diagnosed as colonic carcinoma.
CONCLUSION: Endoscopy contributes to the diagnosis of colonic schistosomiasis although it is nonspecific. A correct diagnosis of colonic schistosomiasis can be established by endoscopy in combination with its clinicopathologic characteristics.
- Citation: Cao J, Liu WJ, Xu XY, Zou XP. Endoscopic findings and clinicopathologic characteristics of colonic schistosomiasis: A report of 46 cases. World J Gastroenterol 2010; 16(6): 723-727
- URL: https://www.wjgnet.com/1007-9327/full/v16/i6/723.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i6.723
Colonic schistosomiasis is defined as a specific acute or chronic inflammatory reaction of Schistosoma ova that are deposited mainly in colorectal mucosa. The majority of humans are infected with Schistosoma japonicum, hematobium and mansoni. Schistosoma japonicum and mansoni often lead to intestinal disease[1]. Chinese people are commonly infected with Schistosoma japonicum. In the 1950s, schistosomiasis was epidemic at a large scale in regions along the Yangtze River and in more than 400 counties in South China[2-4]. Because of the effective prevention and cure measures taken in China in recent years, schistosomiasis has been eliminated in most epidemic regions. However, its spread is not yet completely controlled and schistosomiasis occurs every year in a small number of people in the epidemic regions of China[3,4]. Since the number of colonic schistosomiasis patients is small, physicians know little about it, thus often misdiagnosing intestinal schistosomiasis. In the present study, we made a retrospective analysis of endoscopy findings and clinicopathologic characteristics of 46 colonic schistosomiasis patients in order to further improve our understanding of the disease and decrease its misdiagnosis.
From May 2005 to May 2009, 46 patients with colonic schistosomiasis were admitted to Endoscopy Center, Affiliated Gulou Hospital of Medical School of Nanjing University (Nanjing, China). Their endoscopy findings and clinicopathologic characteristics were retrospectively analyzed. The patients gave their written informed consent before colonoscopy (Olympus CF-240I or CF-H260AZI, Tokyo, Japan). When a lesion was detected at colonoscopy, tumor tissue samples were taken and fixed in 4% buffered paraformaldehyde, embedded in paraffin, and stained with hematoxylin-eosin. Two pathologists independently examined the tumor tissue sections under a light microscope (Olympus, Tokyo, Japan).
Of the 46 colonic schistosomiasis patients (32 men and 14 women) at the age of 65.4 ± 10.8 years (range 40-80 years), 31 were from the epidemic areas of schistosomiasis and 15 from the non-epidemic areas with a history of contacting water containing Schistosoma ova.
The time from onset of symptoms to visit of a doctor ranged 4 d to 7 years (mean 4.5 years). The common symptoms were repeated fever and hematochezia. Among the symptoms occurred in 46 patients, diarrhea was found in 31 (67.3%), bloody stool in 8 (17.3%), abdominal pain in 35 (76.1%), incomplete intestinal obstruction in 3 (4.7%), turgescent spleen in 6 (8.4%) and hepatosplenic schistosomiasis in 1 patients (1.5%), respectively.
All the patients underwent colonoscopy with a success in 41 patients and a failure in 5 patients. The whole colon, right colon, and left colon were involved in 4 (8.7%), 4 (8.7%), and 38 (82.6%) patients, respectively (Table 1). Among the 38 patients with their left colon involved, only descending colon, descending and transverse colon, only sigmoid colon, sigmoid colon and rectum, and only rectum were involved in 8, 1, 3, 9, and 17 patients, respectively. The lesion was mainly located in rectum and sigmoid colon of 29 patients (63.0%).
| Location of colonic injury | n | Percent |
| Cecum | 2 | 4.3 |
| Whole colon | 4 | 8.7 |
| Ascending + transverse colon | 1 | 2.2 |
| Descending colon | 8 | 17.4 |
| Descending + transverse colon | 1 | 2.2 |
| Hepatic flexure of colon | 1 | 2.2 |
| Sigmoid colon | 3 | 6.5 |
| Sigmoid colon + rectum | 9 | 19.6 |
| Rectum | 17 | 37.0 |
Among the 46 patients, acute submucosal colitis, chronic submucosal colitis, chronic active submucosal colitis were diagnosed in 1, 16, and 29 patients, respectively. Friable or edematous mucosa with more mucus exudates, scattered petechial hemorrhage, invisible submucosal blood vessels, erythema and granularity of mucosa with irregular ulcerations could be observed in acute submucosal colitis patients by colonoscopy. Chronic submucosal colitis was characterized by pale intestinal mucosa, confused vascular net with more flat or elevated yellow nodules, even intestine stricture, single polyp or more polyps. Acute and chronic inflammation reactions occurred simultaneously in the same or different segments of colon, and a clear dividing line emerged between the two types of inflammation in chronic active submucosal colitis patients. Acute inflammation was often observed in the right colon and chronic inflammation usually occurred in the left colon. Acute and chronic inflammation was also observed in the same segment of colon (Figure 1).
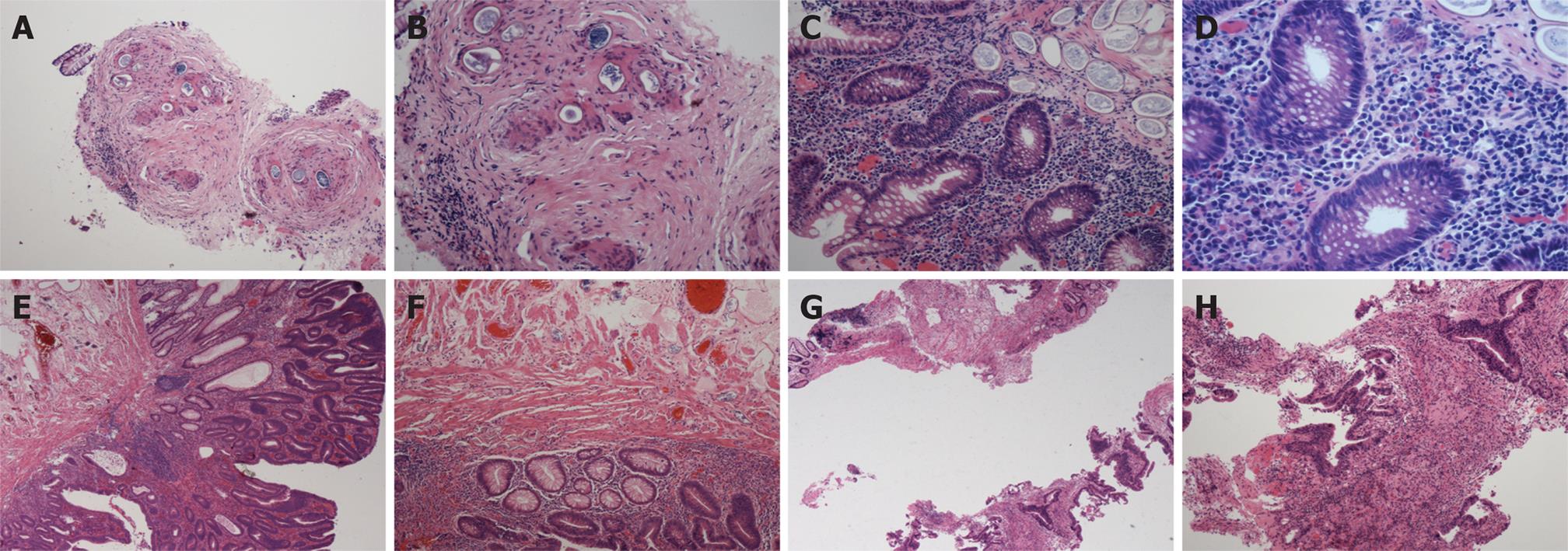
Intact Schistosoma ova were deposited in lamina propria with infiltration of eosinocytes and neutrophilic granulocytes in acute schistosomal colitis patients. Schistosoma ova were calcified and deposited with infiltration of lymphocytes and plasma cells in submucosa, lamina propria in chronic schistosomal colitis patients. Atrophy of intestinal mucosa epithelium, reduction of intestinal glands, submucosal hyperblastosis and different degrees of fibrosis were also observed in chronic schistosomal colitis patients. Two different types of Schistosoma ova were found in chronic and acute schistosomal colitis patients. In addition, Schistosoma oviposition was associated with the clinical and histopathological changes in colonic schistosomiasis (Figure 2).
Colonoscopy showed that a single polyp in 17 out of the 46 patients. Among the 17 patients, hyperplastic polyps, canalicular adenoma with a low-grade intraepithelial neoplastic change and tubulovillous adenoma with a high-grade intraepithelial neoplastic change were detected in 10, 5 and 2 patients, respectively. Of the 46 patients, 8 were diagnosed as colonic carcinoma, including papillary adenocarcinoma in 2, mucinous adenocarcinoma in 1, signet-ring cell carcinoma in 1, and tubular adenocarcinoma in 4 patients, respectively.
High frequency electric snare of colonic polyps was performed under a colonoscope for 17 colonic schistosomiasis patients. Among these patients, colonic carcinoma was radically removed in 8 patients, schistosomiasis was treated with antischistosomiasis drug (praziquantel) in 1 patient and the other patients received symptomatic treatment.
Schistosoma ova are mainly parasitized in the inferior mesenteric and portal vein when one is infected with them. Intestinal schistosomiasis occurs due to deposition of Schistosoma ova in submucosa producing a granulomatous reaction[5]. Mucosal edema, hemorrhage and ulceration may occur in bowel wall at its early stage, while thickened bowel wall, polyps, or enteric cavity stricture, etc, can be detected at its advanced stage[6]. In our study, colonic schistosomiasis was divided into acute schistosomal colitis, chronic schistosomal colitis, and chronic active schistosomal colitis according to the inflammation reaction in colon. In the present study, 46 colonic schistosomiasis patients included 1 acute schistosomal colitis, 16 chronic schistosomal colitis and 29 chronic active schistosomal colitis patients. The difference between acute and chronic schistosomal colitis depends on whether Schistosoma ova are intact. A Schistosoma ovum or several Schistosoma ova are deposited in submucosa and lamina propria in acute schistosomal colitis patients with infiltration of eosinocytes. Schistosoma ova are calcified and deposited in submucosa and lamina propria with infiltration of lymphocytes and epithelioid cells in chronic schistosomal colitis patients. Fibroplasia could be observed in colonic submucosa of chronic schistosomal colitis patients. The deposition sites of Schistosoma ova are sigmoid colon, upper segment of rectum, descending colon, transverse colon, cecum and ascending colon. In our study, the lesion was located in the rectum and sigmoid colon of 29 patients (63.0%) and in the colon segments of 17 patients (37.0%).
Although nonspecific, colonoscopy may provide valuable information for the diagnosis of colonic schistosomiasis. Colonoscopy can show edematous, congestive mucosa and petechial hemorrhage in acute schistosomal colitis patients, and confused vascular net with more close-set flat or elevated yellow nodules, polyps and intestine stricture in chronic schistosomal colitis patients. Acute and chronic inflammation could be observed in colon segments of chronic active schistosomal colitis patients. The most characteristic finding is the gray-yellow or yellowish white schistosomal nodules similar to those of pseudomembranous enterocolitis. In our study, colonoscopy showed schistosomal nodules in only 6 patients (16.2%), which may be the reason why physicians cannot make a correct diagnosis of the disease based only on colonoscopic findings. Schistosomal oviposition is the golden diagnostic standard for colonic schistosomiasis. Schistosoma ova are deposited in lamina propria and/or in submucosa[7] with infiltration of eosinocytes and neutrophilic granulocytes in acute schistosomal colitis patients. Schistosoma ova are calcified or ruptured with infiltration of lymphocytes and plasma cells in submucosa and lamina propria of chronic schistosomal colitis patients. Submucosal hyperblastosis and fibrosis could also be found in chronic schistosomal colitis patients. Two types of Schistosoma ova can be detected in chronic acute schistosomal colitis patients.
In our study, a definite diagnosis was not made only based on endoscopic findings. Four patients were misdiagnosed as ulcerative colitis, 1 as Crohn’s disease, and 7 as ischemic colitis, indicating that physicians know little about the disease.
Colorectal cancer is one of the most common malignant gastrointestinal tumors and its occurrence has increased in recent years. Its pathogenesis remains unclear, thus requiring further study. Schistosoma japonicum infection is considered a significant risk factor for colonic cancer in Asia although it is still controversial[5]. A total of 454 colorectal carcinoma specimens have been studied in China, showing that 289 of them are associated with Schistosoma japonicum infection[8]. Kaw et al[9] studied 1277 colonic carcinoma patients and found that schistosomiasis is often accompanied with rectal carcinoma. Mei et al [10] studied 352 colonic carcinoma patients and found that 14.3% of them have the complication of schistosomiasis. These colonic carcinomas are moderately-differentiated tubular and mucinous adenocarcinomas. In the present study, 8 colonic schistosomiasis patients (17.3%) had complication of colonic carcinoma, and 2 had complications of a high-grade intraepithelial neoplastic change and precancerous lesion. However, the mechanism of Schistosoma japonicum infection leading to carcinoma is unclear, which may be associated with chronic inflammation, ulceration and mucosa repair due to Schistosoma ova. Tumorigenesis may result from gene mutations in epithelial cells of glands due to the long time stimulation of mucosa by Schistosoma ova.
The incidence of colonic schistosomiasis has been greatly declined. However, many complications may occur if it is not early diagnosed and treated. Colonic schistosomiasis should be diagnosed based on its clinical symptoms and signs, coloscopic findings and pathologic characteristics. If Schistosoma ova are found in biopsy, it can be diagnosed. If Schistosoma ova are not observed in biopsy, the near-normal crypts with excess mucus and diffuse or focal infiltration of eosinophilic granulocytes may be highly suggestive of colonic schistosomiasis[11].
Schistosomiasis was epidemic at a large scale in the regions along the Yangtze River and more than 400 counties in South China 50 years ago. Thanks to the effective prevention and cure measures taken in recent years, schistosomiasis has been eliminated in most epidemic regions. However, its spread is not completely controlled in several regions and schistosomiasis still occurs in a small number of people in its endemic region, which threatens their health. Since the number of patients with still suffer from schistosomiasis has greatly declined, physicians know little about it and often misdiagnose it.
Colonic schistosomiasis is seldom reported at present. In this study, the endoscopy findings and clinicopathologic characteristics of 46 colonic schistosomiasis patients were retrospectively analyzed, showing that Schistosoma japonicum infection may be a risk factor for colonic cancer.
The endoscopy findings and clinicopathologic characteristics of 46 colonic schistosomiasis patients were analyzed. The disease was classified into acute schistosomal colitis, chronic schistosomal colitis, and chronic active schistosomal colitis. The results indicate that Schistosoma japonicum infection may be a risk factor for colonic cancer and schistosomal polyps should be removed under an endoscope.
The endoscopy findings and clinicopathologic characteristics of colonic schistosomiasis were described, which may improve our further understanding of the disease and decrease its misdiagnosis.
Colonic schistosomiasis: An acute and chronic specific inflammatory reaction due to Schistosoma ova in colonic and rectal mucosa. Pseudomembranous enterocolitis: An infection of the colon with Clostridium difficile, characterized by diarrhea, fever, vomiting and abdominal pain.
This paper is interesting and should be published. The authors, however, need to highlight the high incidence of cancer in their populations.
Peer reviewer: Patrick O’Dwyer, MB, BCh, BAO, FRCS, MCh, FRCS (Glasg), Professor, University Department of Surgery, Western Infirmary, Glasgow, G11 6NT, United Kingdom
S- Editor Wang JL L- Editor Wang XL E- Editor Yang C
| 2. | Zheng J. Schistosomiasis control and its prospects in China. Zhongguo Xuexichongbing Fangzhi Zazhi. 2003;15:1-2. |
| 3. | Cao ZG, Wang TP. Epidemic situation of urban schistosomiasis and measures for prevention and control in China. Zhongguo Xuexichongbing Fangzhi Zazhi. 2007;19:315-316, 320. |
| 4. | Zheng J. Prevention and control of Chinese schistosomiasis in the 21st century. Zhonghua Liuxingbingxue Zazhi. 2002;23:81-82. |
| 5. | Yosry A. Schistosomiasis and neoplasia. Contrib Microbiol. 2006;13:81-100. |
| 6. | Ohmae H, Sy OS, Chigusa Y, Portillo GP. Imaging diagnosis of schistosomiasis japonica--the use in Japan and application for field study in the present endemic area. Parasitol Int. 2003;52:385-393. |
| 7. | Godyn JJ, Siderits R, Hazra A. Schistosoma mansoni in colon and liver. Arch Pathol Lab Med. 2005;129:544-545. |
| 8. | Ming-Chai C, Chi-Yuan C, Pei-Yu C, Jen-Chun H. Evolution of colorectal cancer in schistsosomiasis: transitional mucosal changes adjacent to large intestinal carcinoma in colectomy specimens. Cancer. 1980;46:1661-1675. |
| 9. | Kaw LL Jr, Punzalan CK, Crisostomo AC, Bowyer MW, Wherry DC. Surgical pathology of colorectal cancer in Filipinos: implications for clinical practice. J Am Coll Surg. 2002;195:188-195. |
| 10. | Mei J, Hong HL, Ding YP, Fang YM. Clinicopathologic characteristics of chronic schistosomiasis complicating carcinoma of large intestine. Zhonghua Xiaohuaneijing Zazhi. 2004;21:49-50. |
| 11. | Radhakrishnan S, Al Nakib B, Shaikh H, Menon NK. The value of colonoscopy in schistosomal, tuberculous, and amebic colitis. Two-year experience. Dis Colon Rectum. 1986;29:891-895. |