Published online Oct 28, 2010. doi: 10.3748/wjg.v16.i40.5070
Revised: June 16, 2010
Accepted: June 23, 2010
Published online: October 28, 2010
AIM: To investigate the outcome of patients with hepatitis C virus (HCV) infection undergoing liver retransplantation.
METHODS: Using the UK National Registry, patients undergoing liver transplantation for HCV-related liver disease were identified. Data on patient and graft characteristics, as well as transplant and graft survival were collected to determine the outcome of HCV patients undergoing retransplantation and in order to identify factors associated with transplant survival.
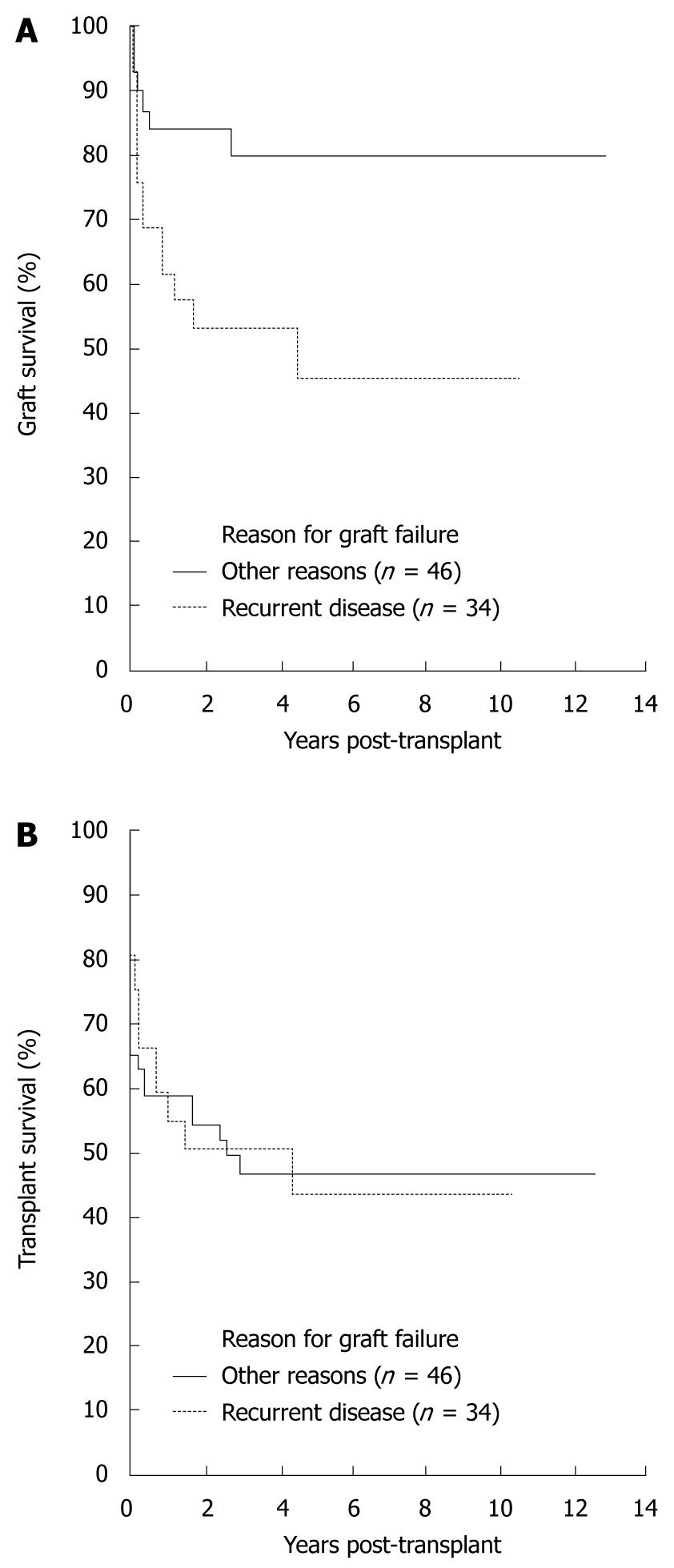
RESULTS: Between March 1994 and December 2007, 944 adult patients were transplanted for HCV-related liver disease. At the end of follow-up, 617 of these patients were alive. In total, 194 (21%) patients had first graft failure and of these, 80 underwent liver retransplantation, including 34 patients where the first graft failed due to recurrent disease. For those transplanted for HCV-related disease, the 5-year graft survival in those retransplanted for recurrent HCV was 45% [95% confidence interval (CI): 24%-64%] compared with 80% (95% CI: 62%-90%) for those retransplanted for other indications (P = 0.01, log-rank test); the 5-year transplant survival after retransplantation was 43% (95% CI: 23%-62%) and 46% (95% CI: 31%-60%), respectively (P = 0.8, log-rank test). In univariate analysis of all patients retransplanted, no factor analyzed was significantly associated with transplant survival.
CONCLUSION: Outcomes for retransplantation in patients with HCV infection approach agreed criteria for minimum transplant benefit. These data support selective liver retransplantation in patients with HCV infection.
- Citation: Rowe IA, Barber KM, Birch R, Curnow E, Neuberger JM. Retransplantation for graft failure in chronic hepatitis C infection: A good use of a scarce resource? World J Gastroenterol 2010; 16(40): 5070-5076
- URL: https://www.wjgnet.com/1007-9327/full/v16/i40/5070.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i40.5070
End-stage liver disease due to chronic hepatitis C virus (HCV) is the most common indication for liver transplantation in Europe and the United States[1,2]. Recurrent viral infection of the allograft is near universal. Ninety percent of all patients transplanted with HCV have evidence of HCV in the allograft within 6 mo[3] and at least 20% of patients transplanted for HCV infection will develop cirrhosis of their allograft[1,4,5]. Allograft cirrhosis is associated with recurrence of disease before 6 mo post-transplantation[6], severe necroinflammation and confluent necrosis at the time of first histological diagnosis, pre-transplant viral load and episodes of treated rejection[7]. Cirrhosis is associated with high rates of graft loss to recurrent disease[8]. Recurrent HCV infection in the setting of immunosuppression rarely follows the more aggressive course of recurrent cholestatic hepatitis which may cause early graft failure.
Current data show that the prognosis for patients with cirrhosis and graft failure from recurrent HCV in their grafts is poor, with only 41% surviving 1 year after the development of decompensation[5]. Antiviral therapy is largely ineffective in this setting[9] and retransplantation is the only therapeutic option. Consideration of retransplantation in the setting of graft failure due to recurrent HCV infection is therefore an increasing clinical problem and results in increasing pressure on an already limited resource. Retransplantation, however, is associated with a worse clinical outcome than for first grafts regardless of the indication[10]. There have been several studies addressing the issue of retransplantation in patients with HCV and results from these studies have yielded discordant results: these are summarized in Table 1[10-19]. Initial studies reported an increased mortality following retransplantation in patients with HCV infection, frequently in the first months after retransplantation[11,13,18]. These studies were all retrospective and largely database-dependent. Indeed the United Network for Organ Sharing (UNOS) data has been re-evaluated on 2 occasions with the predictors of poor outcomes changing with time: the most recent analysis showing no difference between outcomes for patients with and without HCV infection undergoing retransplantation[14]. That said, there have been particular factors [including model for end-stage liver disease (MELD) score and donor age] and subgroups (i.e. those retransplanted between 90 d and 1 year after first liver transplant) identified which increased the risk of retransplant failure. There may be differences amongst those transplanted for HCV infection whose grafts fail due to recurrent disease and those whose grafts fail for other reasons although this, too, is controversial[10,20]. Overall, there is no consensus on the role of retransplantation for recurrent HCV infection.
| Author | Design | Number with HCV infection | Outcome | Predictors |
| Database studies | ||||
| Rosen et al[11] | UNOS database | HCV total 357 | 54% 5-yr survival | HCV associated with mortality (HR 1.3) |
| Watt et al[12] | UNOS database | HCV total 899 | 45% 5-yr survival | MELD > 25 |
| Petellier et al[13] | SRTR database | HCV total 464 | NA | HCV associated with mortality (HR 1.3) |
| Ghabril et al[14] | UNOS database | HCV total 1034 | rOLT 90 d-1 yr: 44% 3-yr survival | MELD > 25 |
| rOLT > 1 yr: 59% 3-yr survival | Donor > 60 | |||
| Donor black | ||||
| WIT > 75 min | ||||
| Rowe et al, current study | UK Transplant database | 34 recurrent HCV | Recurrent HCV rOLT 5-yr graft survival 45% | None |
| 46 HCV | HCV rOLT other reasons HCV 5-yr graft survival 80% | |||
| Center-led studies | ||||
| Roayaie et al[15] | Retrospective single center | HCV total 42 | 52% alive at 6 mo | Donor < 60 |
| PT < 16 s | ||||
| Neff et al[16] | Retrospective single center | HCV total 22 | 50% 1-yr survival | Normal physical activity |
| Carmiel-Haggai et al[17] | Retrospective single center | 47 recurrent HCV | 37% 1-yr mortality | Donor > 60 |
| 62 HCV | Cirrhosis FCH | |||
| McCashland et al[18] | Prospective multicenter | HCV total 43 | 3-yr survival 49% | MELD not predictive |
| Bahra et al[19] | Retrospective single center | 18 recurrent HCV | Recurrent HCV rOLT 5-yr survival 59% | MELD > 25 |
| 11 HCV | HCV rOLT other reasons 5-yr survival 84% | Bilirubin > 15 mg/dL | ||
| Ghabril et al[10] | Retrospective single center | 25 recurrent HCV | 63% 3-yr survival | Donor age > 60 |
| 48 HCV | Recipient > 60 |
In recent years in the United Kingdom (UK) the number of transplants performed has fallen whilst the number of patients waiting has risen by over 90%[20]. Because of the disparity between the numbers of donor organs and potential recipients, rationing must occur and selection criteria for transplant and retransplant are in place in transplant programs around the world. In the UK a meeting of health care professionals, patient representatives, ethicists and the public agreed an expected transplant survival probability of at least 50% at 5 years following liver transplantation as a benchmark of minimum expected survival following liver transplantation[21].
Liver retransplantation in patients with HCV infection is controversial and has been inconsistently associated with transplant survival rates of less than 50% at 5 years. The aim of this current study was therefore to determine overall outcomes after retransplantation in patients with HCV infection in the UK. In addition, we sought to determine whether failure of the first graft due to recurrent HCV-related disease had a significant effect on survival after retransplantation, and whether we could identify factors which predict a poor outcome.
Data were obtained from the National Transplant database. This database is maintained by the Organ Donation and Transplantation Directorate of NHS Blood and Transplant on behalf of transplant services in the UK and the Republic of Ireland. All 944 patients aged 17 years and older undergoing first elective liver transplants for HCV-related liver disease in the UK between 1 March 1994 and 31 December 2007 were included. Patients who were recorded as HCV-positive at time of registration and/or time of transplantation but who did not have an indication for transplantation recorded as HCV were excluded from the analyses. Also excluded were patients receiving grafts from non-heart-beating donors and patients with intestinal failure-related liver disease. Details of the indication were categorized into 4 groups: HCV alone, HCV and alcohol-related liver disease (ALD), HCV and hepatocellular carcinoma (HCC), and HCV and ALD and HCC. In addition, patients undergoing liver retransplantation for reasons other than HCV-related liver disease were identified to act as a comparison group.
Patient, graft and transplant survival were obtained for the 4 HCV groups using the Kaplan Meier estimation method. Survival was compared using the log-rank test. Patient survival was measured from the time of first liver transplant to patient death. Graft survival was defined as time from liver transplant (or retransplant) to graft failure (patient deaths with a functioning graft were censored). Transplant survival was defined as time from transplant (or retransplant) to patient death or graft failure whichever was the earlier (deaths with a functioning graft were included as events).
Graft and transplant survival for the 80 retransplanted patients were obtained using the Kaplan-Meier method. Univariate Cox regression models were used to identify factors associated with liver transplant survival after retransplantation, where the first transplant failed due to disease recurrence. Factors considered were donor age, blood group, gender, height and weight, and recipient age, blood group, gender, height and weight, HCV group for first graft, MELD score[22] at time of second graft, year of first graft, year of second graft, cold ischemia time, hospitalization status, time from first graft to second graft and donor organ appearance. Missing values for donor height, donor weight, recipient height and weight, MELD score and cold ischemia time were replaced with the median value, and missing values for hospitalization status and donor organ appearance were replaced with the modal value.
Of the 944 patients transplanted for HCV-related liver disease during the study period, the majority (n = 521, 55%) were transplanted for HCV alone and for HCV with HCC (n = 261, 28%). In total, 698 (74%) patients were alive at the end of the study period. The 5-year patient survival estimate for patients transplanted for HCV alone was 70% [95% confidence interval (CI): 65%-74%] and for patients transplanted for HCV with HCC the 5-year patient survival was 63% (95% CI: 55%-69%).
Of those transplanted, 617 (65%) first grafts were still functioning at the end of the study period, 133 (14%) patients died with a functioning graft and 194 (21%) grafts failed. In total, the reason for graft failure was indicated as recurrent HCV in 77 patients, and other causes, most commonly acute vascular occlusion and chronic or ductopenic rejection, in 117 patients. Where the first graft failed, 89 patients (45.9% of those with graft failure) were relisted and 80 (41.2%) were retransplanted. Of the 80 patients retransplanted, the reason for failure of the first graft was recorded as recurrent disease in 26 cases, and other reasons in 54 cases. Further analysis of the other reasons for graft failure, as recorded in free text by transplant centers, indicated that graft failure of 8 additional patients was considered to be due to disease recurrence giving a total of 34 patients retransplanted for recurrent disease and 46 patients retransplanted for other reasons. There was no difference in the proportion of patients retransplanted where the first graft failed due to recurrent disease or due to other reasons (χ2 test, P = 0.76).
The clinical information of those patients who underwent retransplantation after first liver transplant for HCV-related liver disease is given in Table 2. The groups were similar in demographic data and severity of liver disease at the time of retransplantation. However, those patients retransplanted for recurrent HCV were less likely to be hospitalized at the time of retransplantation. Those retransplanted for reasons other than recurrent HCV also had a shorter interval between first and second liver transplant and the majority of those patients were retransplanted for acute vascular occlusion (n = 17, 37.0%) and primary graft non-function (n = 11, 23.9%). These 28 patients were transplanted as an emergency and these indications contributed largely to the shortened interval between first and second graft and the increased likelihood of hospitalization seen in this group. The remainder of the patients retransplanted for reasons other than recurrent disease were retransplanted for late vascular complications (6 patients), biliary complications (3 patients), chronic or ductopenic rejection (3 patients), or other reasons (4 patients).
| Characteristic | First graft failed due to | P-value | |
| Recurrent disease | Other reasons | ||
| n | 34 | 46 | |
| Recipient age (yr) | 50.0 ± 8.16 | 53.1 ± 8.14 | 0.090 |
| Recipient blood group | |||
| O | 11 (32.3) | 18 (39.1) | 0.800 |
| A | 16 (47.1) | 18 (39.1) | |
| B | 4 (11.8) | 7 (15.2) | |
| AB | 3 (8.8) | 3 (6.5) | |
| Recipient gender, male | 27 (79.4) | 33 (71.7) | 0.400 |
| Recipient height (cm) | 173.3 ± 9.72 | 169.6 ± 9.94 | 0.090 |
| Recipient weight (kg) | 81.0 ± 13.93 | 77.6 ± 17.48 | 0.400 |
| HCV group for first graft | |||
| HCV alone | 25 (73.5) | 24 (52.2) | |
| HCV + HCC | 3 (8.8) | 16 (34.8) | 0.030 |
| HCV + ALD | 6 (17.6) | 6 (13.0) | |
| MELD score | 19.9 ± 5.08 | 22.1 ± 10.79 | 0.280 |
| Year of first graft | |||
| 1994-2000 | 23 (67.6) | 22 (47.8) | 0.080 |
| 2001-2007 | 11 (32.4) | 24 (52.2) | |
| Year of second graft | |||
| 1994-1998 | 7 (20.6) | 14 (30.4) | 0.060 |
| 1999-2003 | 13 (38.2) | 24 (52.2) | |
| 2004-2007 | 14 (41.2) | 8 (17.4) | |
| Cold ischemia time (h) | 11.9 ± 2.61 | 9.7 ± 3.29 | 0.020 |
| Hospitalization status, Outpatient | 19 (55.9) | 4 (8.7) | < 0.001 |
| Time from first graft to second graft (yr) | 2.8 ± 2.17 | 0.38 ± 1.03 | < 0.001 |
| Donor organ appearance, normal | 28 (82.4) | 40 (87.0) | 0.600 |
Overall graft survival for patients first transplanted for HCV and subsequently retransplanted for recurrent HCV was lower than for those retransplanted for other reasons, as shown in Figure 1A. Five-year graft survival was estimated as 45% (95% CI: 24%-64%) for the recurrent disease group, compared with 80% (95% CI: 62%-90%) for those retransplanted for other reasons (P = 0.01). However, there was no difference in overall transplant survival between these 2 groups, as shown in Figure 1B. Five-year transplant survival in those with recurrent disease was 43% (95% CI: 23%-62%) and 46% (95% CI: 31%-60%) in those retransplanted for other reasons (P = 0.8). The difference between graft and transplant survival between these 2 groups was related to deaths occurring with a functioning graft: one death in the patients retransplanted for recurrent disease and 17 deaths in the patients retransplanted for other reasons. The cause of death in these patients was largely multiple organ failure and infective complications.
Following retransplantation for recurrent HCV, the total number of grafts lost was 16 (47%). The most frequent causes of graft loss were acute vascular occlusion (n = 4), recurrent disease (n = 3) and chronic rejection (n = 2).
Several factors including pre-transplant disease severity and donor factors have previously been identified as predictors of poor outcome after liver retransplantation in patients with HCV infection. These factors, together with other factors considered to impact on retransplant outcome including the timing of liver retransplantation after first liver transplant, were considered in univariate Cox regression analyses in those patients retransplanted for HCV-related liver disease. None of the factors considered in these analyses, including donor age and MELD score at the time of retransplantation, was found to be associated with transplant survival after retransplantation in patients with HCV, as shown in Table 3.
| Variable | Category | n | Hazard ratio (95% CI) | P value |
| Recurrent disease | No | 46 | 1 | |
| Yes | 34 | 0.92 (0.49-1.73) | 0.8 | |
| Donor age (yr) | Linear | 80 | 1.00 (0.98-1.03) | 0.7 |
| Donor blood group | O | 43 | 1 | |
| A, B, AB | 37 | 0.91 (0.49-1.70) | 0.8 | |
| Donor gender | Male | 37 | 1 | |
| Female | 43 | 1.23 (0.66-2.29) | 0.5 | |
| Donor height (cm) | Linear | 80 | 0.98 (0.95-1.01) | 0.3 |
| Donor weight | Linear | 80 | 0.98 (0.96-1.01) | 0.2 |
| Recipient age (yr) | Linear | 80 | 0.99 (0.96-1.03) | 0.6 |
| Recipient blood group | O | 29 | 1 | |
| A, B, AB | 51 | 1.00 (0.52-1.91) | 0.99 | |
| Recipient gender | Male | 60 | 1 | |
| Female | 20 | 1.38 (0.70-2.72) | 0.4 | |
| Recipient height (cm) | Linear | 80 | 0.98 (0.95-1.01) | 0.1 |
| Recipient weight (kg) | Linear | 80 | 0.99 (0.98-1.02) | 0.6 |
| HCV group for first graft | HCV alone | 49 | 1 | |
| HCV + HCC | 19 | 2.15 (1.07-4.30) | 0.03 | |
| HCV + ALD | 12 | 1.13 (0.46-2.81) | 0.8 | |
| MELD score | Linear | 80 | 1.00 (0.96-1.05) | 0.9 |
| Year of first graft | Linear | 80 | 1.04 (0.89-1.21) | 0.6 |
| Year of second graft | Linear | 80 | 0.96 (0.87-1.06) | 0.47 |
| Cold ischemia time (h) | Linear | 80 | 0.99 (0.92-1.06) | 0.74 |
| Hospitalization status | Outpatient | 24 | 1 | |
| Inpatient | 56 | 1.36 (0.66-2.78) | 0.4 | |
| Time from first to second graft (yr) | Linear | 80 | 1.04 (0.89-1.21) | 0.6 |
| Donor organ appearance | Normal | 68 | 1 | |
| Abnormal | 12 | 1.04 (0.44-2.47) | 0.9 |
For those patients developing graft failure, and in particular from recurrent HCV-related liver disease, the outlook is poor and there is no alternative to consideration of liver retransplantation. The outcome of patients retransplanted with chronic HCV infection is relatively poor, and, in the context of organ shortage, use of scarce resources for this indication is, therefore, controversial. As the number of patients being transplanted for HCV is increasing, so is the number of patients with graft failure due to recurrent HCV infection. Previous studies are conflicting, with some suggesting such a poor outcome in these patients that use of a liver graft cannot be justified[16,23]. More recent reports however have stated that patients should not be denied retransplantation merely based on a diagnosis of chronic HCV infection[10,14,18]. Furthermore, repeated analyses of the UNOS database initially demonstrated that HCV infection had a negative impact on survival after liver retransplantation but later studies did not support this finding[14] suggesting that, with increased experience, transplant centers may have improved outcomes for patients with graft failure and HCV infection. It should be noted that there is inconsistent reporting of confidence intervals of survival rates in these studies and these findings have contributed to the controversy regarding the utility of retransplantation in HCV infection.
The shortage of donor organs has focused attention on the optimal use of liver allografts. A consensus meeting of UK surgeons and physicians, health care professionals, ethicists, patients and the public agreed a minimum transplant survival of 50% at 5 years[21]. This is in keeping with the statement from the International Liver Transplantation Society Expert Panel who suggested a 1-year survival rate of at least 60% should be anticipated before listing a patient for retransplantation with recurrent HCV-related disease[24]. This guidance allows for the best use of a scarce resource, and also gives much needed transparency to transplant programs. Importantly, this will however disadvantage some patients who would otherwise have gained some benefit from transplantation.
In this study, representing a highly selected patient population, the 5-year transplant survival for patients with chronic HCV infection who were retransplanted was less than 50%, regardless of the cause of failure of the first graft, although the confidence intervals reported here were wide due to the relatively small numbers of patients included. However, in patients retransplanted for recurrent HCV, 5-year graft survival was 45%. In contrast, the 5-year graft survival was 80% in those transplanted for reasons other than recurrence. This discrepancy between graft and transplant survival in patients retransplanted for reasons other than recurrent HCV is likely to be explained in part by the short interval between first and second liver transplant. Many of these patients are, by definition, not fully recovered from the first transplant, and the proportion of patients dying from multiple organ failure and infective complications likely reflect this. This important observation indicates that, of the patients retransplanted for reasons other than HCV disease recurrence, those who survive the early weeks after transplantation have a relatively good long-term outlook.
In total, 5% of all patients retransplanted with HCV infection lost their second graft to recurrent disease, including 3 of 34 (8.8%) patients retransplanted for recurrent HCV-related disease. This is a clinically relevant proportion of these patients and this calls into question findings of previous studies addressing this. Since transplant failure following retransplantation is greater than after first transplant regardless of indication, factors that further impact on transplant survival after retransplantation are thus important. The timing of recurrent disease in the first liver transplant has been suggested to impact on the prevalence of recurrent disease in the second liver transplant in this group[25], although this too has been questioned[17]. In this study a large proportion of patients were retransplanted between 1 and 3 years after the first liver transplant. The small numbers of patients transplanted at times other than this has meant that we have been unable to reliably investigate this matter.
Several studies have investigated factors associated with graft loss in HCV infection following retransplantation. These have determined negative predictors of mortality in the recipient, including MELD score greater than 25, elevated serum creatinine and bilirubin, and prolonged prothrombin time[7,14]. In addition, donor age greater than 60 years has consistently been associated with negative outcomes in individuals retransplanted with HCV infection. Analyses of these factors in this study did not show any association with transplant survival. This is likely to be related, at least in part, to the relatively low numbers of patients retransplanted with HCV infection, the heterogeneity of this group as well as the skill of the surgeon in matching donor and recipient. At present, in the UK, there are national guidelines for selection of patients but the allocation of donor livers is done on a center-specific basis with the surgeon determining the most appropriate recipient for a liver donated from a heartbeating or non-heartbeating donor. Similarly, there are center-specific protocols regarding the management of recurrent HCV infection after liver transplantation. In this study, the details of these protocols and whether patients being considered for liver retransplantation had received antiviral therapy were not recorded. However, widespread use of combination antiviral therapy has only recently entered clinical practice and although we saw no clear effect of year of first or second liver transplant on transplant outcome, it is likely too soon to assess what effect this strategy may have.
In this national study of transplant outcome after retransplantation for HCV, we have shown that transplant survival rates fall below those normally accepted for survival after transplant, regardless of whether retransplantation was related to HCV recurrence or not. Furthermore, we have not been able to demonstrate any factors associated with increased, or indeed decreased, transplant failure. Although numbers are relatively small, this series is one of the largest conducted.
Whilst there is much work focused on the early identification of individuals with rapid development of fibrosis after transplantation[26], and antiviral treatment outcomes may be improving[27], over the coming years many of those transplanted with chronic HCV infection will develop graft failure and the question of retransplantation will be raised. Previously published studies are conflicting and this study adds to the evidence base supporting selective retransplantation in the setting of chronic HCV infection. Clear and careful consideration must therefore be given when assessing these individuals for retransplantation.
Hepatitis C virus (HCV) infection is common and is a leading indication for liver transplantation. Following transplantation, however, HCV infects the transplanted liver and disease recurrence is rapid and may lead to transplant failure. This inevitably leads to questions regarding the utility of repeat liver transplantation. It is not clear whether liver retransplantation is appropriate in patients with either recurrent HCV or with HCV who require liver retransplantation for other reasons.
There is significant controversy as to whether patients with HCV infection should undergo liver retransplantation, and if so which patients would be most appropriate.
The authors demonstrate that those patients with recurrent HCV infection undergoing liver retransplantation fare worse, particularly with regard to graft survival, than those undergoing liver retransplantation for other reasons. However, at 5 years after liver retransplantation, transplant survival in both groups is at the limit of acceptability (50% survival at 5 years after transplant).
This study adds weight to the evidence supporting selective liver retransplantation in patients with HCV infection.
Graft survival is defined as time from liver transplant (or retransplant) to graft failure. In this case a patient death with a functioning graft is not considered as an event. Transplant survival however is defined as time from transplant (or retransplant) to patient death or graft failure whichever was the earlier.
This is a well-designed and structured manuscript addressing a controversial issue and is worth publication.
Peer reviewers: Giuseppe Orlando, MD, PhD, Department of Health Sciences, Wake Forest Institute for Regenerative Medicine, 391 Technology Way, Winston Salem, NC 27101, United States; Laura Lladó, PhD, Department of Surgery, Liver Transplant Unit, Hospital Universitari de Bellvitge, IDIBELL, 08907 Barcelona, Spain; Norbert Senninger, Professor, Department of General Surgery, University Clinics, Westphalian-Wilhelm’s-University, Waldeyerstrasse 1, D-48149 Muenster, Germany
S- Editor Wang JL L- Editor Cant MR E- Editor Ma WH
| 1. | Féray C, Caccamo L, Alexander GJ, Ducot B, Gugenheim J, Casanovas T, Loinaz C, Gigou M, Burra P, Barkholt L. European collaborative study on factors influencing outcome after liver transplantation for hepatitis C. European Concerted Action on Viral Hepatitis (EUROHEP) Group. Gastroenterology. 1999;117:619-625. |
| 2. | Charlton M. Hepatitis C infection in liver transplantation. Am J Transplant. 2001;1:197-203. |
| 3. | Ballardini G, De Raffele E, Groff P, Bioulac-Sage P, Grassi A, Ghetti S, Susca M, Strazzabosco M, Bellusci R, Iemmolo RM. Timing of reinfection and mechanisms of hepatocellular damage in transplanted hepatitis C virus-reinfected liver. Liver Transpl. 2002;8:10-20. |
| 4. | Gane E. The natural history and outcome of liver transplantation in hepatitis C virus-infected recipients. Liver Transpl. 2003;9:S28-S34. |
| 5. | Berenguer M, Prieto M, Rayón JM, Mora J, Pastor M, Ortiz V, Carrasco D, San Juan F, Burgueño MD, Mir J. Natural history of clinically compensated hepatitis C virus-related graft cirrhosis after liver transplantation. Hepatology. 2000;32:852-858. |
| 6. | Ercolani G, Grazi GL, Ravaioli M, Del Gaudio M, Cescon M, Varotti G, Ramacciato G, Vetrone G, Zanello M, Pinna AD. Histological recurrent hepatitis C after liver transplantation: Outcome and role of retransplantation. Liver Transpl. 2006;12:1104-1111. |
| 7. | Ghobrial RM, Steadman R, Gornbein J, Lassman C, Holt CD, Chen P, Farmer DG, Yersiz H, Danino N, Collisson E. A 10-year experience of liver transplantation for hepatitis C: analysis of factors determining outcome in over 500 patients. Ann Surg. 2001;234:384-393; discussion 393-394. |
| 8. | Rowe IA, Webb K, Gunson BK, Mehta N, Haque S, Neuberger J. The impact of disease recurrence on graft survival following liver transplantation: a single centre experience. Transpl Int. 2008;21:459-465. |
| 9. | Bizollon T, Ahmed SN, Radenne S, Chevallier M, Chevallier P, Parvaz P, Guichard S, Ducerf C, Baulieux J, Zoulim F. Long term histological improvement and clearance of intrahepatic hepatitis C virus RNA following sustained response to interferon-ribavirin combination therapy in liver transplanted patients with hepatitis C virus recurrence. Gut. 2003;52:283-287. |
| 10. | Ghabril M, Dickson RC, Machicao VI, Aranda-Michel J, Keaveny A, Rosser B, Bonatti H, Krishna M, Yataco M, Satyanarayana R. Liver retransplantation of patients with hepatitis C infection is associated with acceptable patient and graft survival. Liver Transpl. 2007;13:1717-1727. |
| 11. | Rosen HR, Martin P. Hepatitis C infection in patients undergoing liver retransplantation. Transplantation. 1998;66:1612-1616. |
| 12. | Watt KD, Lyden ER, McCashland TM. Poor survival after liver retransplantation: is hepatitis C to blame? Liver Transpl. 2003;9:1019-1024. |
| 13. | Pelletier SJ, Schaubel DE, Punch JD, Wolfe RA, Port FK, Merion RM. Hepatitis C is a risk factor for death after liver retransplantation. Liver Transpl. 2005;11:434-440. |
| 14. | Ghabril M, Dickson R, Wiesner R. Improving outcomes of liver retransplantation: an analysis of trends and the impact of Hepatitis C infection. Am J Transplant. 2008;8:404-411. |
| 15. | Roayaie S, Schiano TD, Thung SN, Emre SH, Fishbein TM, Miller CM, Schwartz ME. Results of retransplantation for recurrent hepatitis C. Hepatology. 2003;38:1428-1436. |
| 16. | Neff GW, O'Brien CB, Nery J, Shire NJ, Nishida S, delaGarza J, Montalbano M, Safdar K, Ruiz P, Rideman E. Factors that identify survival after liver retransplantation for allograft failure caused by recurrent hepatitis C infection. Liver Transpl. 2004;10:1497-1503. |
| 17. | Carmiel-Haggai M, Fiel MI, Gaddipati HC, Abittan C, Hossain S, Roayaie S, Schwartz ME, Gondolesi G, Emre S, Schiano TD. Recurrent hepatitis C after retransplantation: factors affecting graft and patient outcome. Liver Transpl. 2005;11:1567-1573. |
| 18. | McCashland T, Watt K, Lyden E, Adams L, Charlton M, Smith AD, McGuire BM, Biggins SW, Neff G, Burton JR Jr. Retransplantation for hepatitis C: results of a U.S. multicenter retransplant study. Liver Transpl. 2007;13:1246-1253. |
| 19. | Bahra M, Neumann UP, Jacob D, Berg T, Neuhaus R, Langrehr JM, Neuhaus P. Outcome after liver re-transplantation in patients with recurrent chronic hepatitis C. Transpl Int. 2007;20:771-778. |
| 20. | van der Meulen JH, Lewsey JD, Dawwas MF, Copley LP. Adult orthotopic liver transplantation in the United Kingdom and Ireland between 1994 and 2005. Transplantation. 2007;84:572-579. |
| 21. | Neuberger J, James O. Guidelines for selection of patients for liver transplantation in the era of donor-organ shortage. Lancet. 1999;354:1636-1639. |
| 22. | Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-470. |
| 23. | McCashland TM. Retransplantation for recurrent hepatitis C: positive aspects. Liver Transpl. 2003;9:S67-S72. |
| 24. | Wiesner RH, Sorrell M, Villamil F. Report of the first International Liver Transplantation Society expert panel consensus conference on liver transplantation and hepatitis C. Liver Transpl. 2003;9:S1-S9. |
| 25. | Berenguer M, Prieto M, Palau A, Rayón JM, Carrasco D, Juan FS, López-Labrador FX, Moreno R, Mir J, Berenguer J. Severe recurrent hepatitis C after liver retransplantation for hepatitis C virus-related graft cirrhosis. Liver Transpl. 2003;9:228-235. |
| 26. | Carrión JA, Torres F, Crespo G, Miquel R, García-Valdecasas JC, Navasa M, Forns X. Liver stiffness identifies two different patterns of fibrosis progression in patients with hepatitis C virus recurrence after liver transplantation. Hepatology. 2010;51:23-34. |
| 27. | Selzner N, Renner EL, Selzner M, Adeyi O, Kashfi A, Therapondos G, Girgrah N, Herath C, Levy GA, Lilly L. Antiviral treatment of recurrent hepatitis C after liver transplantation: predictors of response and long-term outcome. Transplantation. 2009;88:1214-1221. |