Published online Oct 7, 2010. doi: 10.3748/wjg.v16.i37.4751
Revised: July 18, 2010
Accepted: July 25, 2010
Published online: October 7, 2010
Benign stricture is a relatively common complication of colorectal anastomosis after low anterior resection. On occasion, the anastomosis may close completely. A variety of endoscopic techniques have been described, but there is a lack of data from controlled prospective trials as to the optimal approach. Through-the-scope balloon dilatation is well known and easy to perform. Some case reports describe different endoscopic approaches, including endoscopic electrocision with a papillotomy knife or hook knife. We report a case of a colorectal anastomosis web occlusion, treated without electrocision. Gastrografin enema and sigmoidoscopy showed complete obstruction at the anastomotic site due to the presence of an anastomotic occlusive web. In order to avoid thermal injuries, we decided to use a suprapapillary biliary puncture catheter. The Artifon catheter was inserted into the center of the circular staple line at the level of the anastomosis, and fluoroscopic identification of the proximal bowel was obtained with dye injection. A 0.025-inch guidewire was then passed through the catheter into the colon and progressive pneumatic dilatation was performed. The successful destruction of the occlusive web facilitated passage of the colonoscope, allowing evaluation of the entire colon and stoma closure after three months of follow-up. The patient tolerated the procedure well, with no complications. This report highlights an alternative non-electrosurgical approach that uses a new device that proved to be safe and useful.
- Citation: Curcio G, Spada M, Francesco FD, Tarantino I, Barresi L, Burgio G, Traina M. Completely obstructed colorectal anastomosis: A new non-electrosurgical endoscopic approach before balloon dilatation. World J Gastroenterol 2010; 16(37): 4751-4754
- URL: https://www.wjgnet.com/1007-9327/full/v16/i37/4751.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i37.4751
Benign stricture is a relatively common complication of colorectal anastomosis after low anterior resection, occurring in 5.8% to 20% of cases. On occasion, the anastomosis may close completely. Factors promoting development of benign anastomotic strictures are still poorly understood, but include ischemia, dehiscence, and radiation therapy. In the majority of patients, an anastomotic stricture is a serious condition that may require repeated endoscopic treatment or surgery. Direct digital dilatation or transrectal surgical treatment is possible if the anastomosis is located in the lower rectum. Endoscopic balloon dilatation is the best method for all patients in whom these procedures for the lower rectum cannot be done[1-5].
Intervention with the colonoscope is the first treatment option. A variety of endoscopic techniques have been described, but there is a lack of data from controlled prospective trials as to the optimal approach. Through-the-scope (TTS) balloon dilatation is well known and easy to perform. Some cases reported in the literature describe different endoscopic approaches, including endoscopic electrocision with a papillotomy knife or hook knife[6,7].
We report a case of a colorectal anastomosis web occlusion, treated without electrocision by employing an Artifon catheter puncture before balloon dilatation.
In March 2009, a 70-year-old man, diagnosed with rectal cancer, underwent laparoscopy-assisted low anterior resection, with a protective loop ileostomy, at our institute.
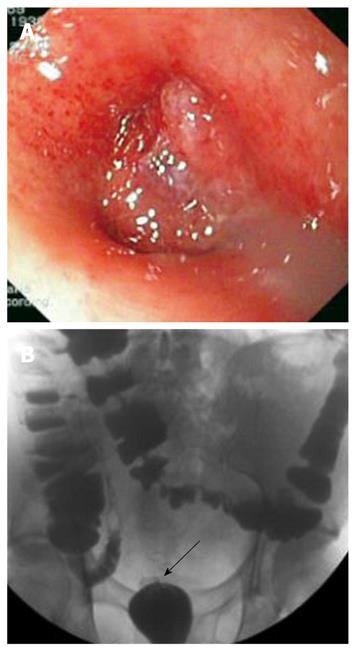
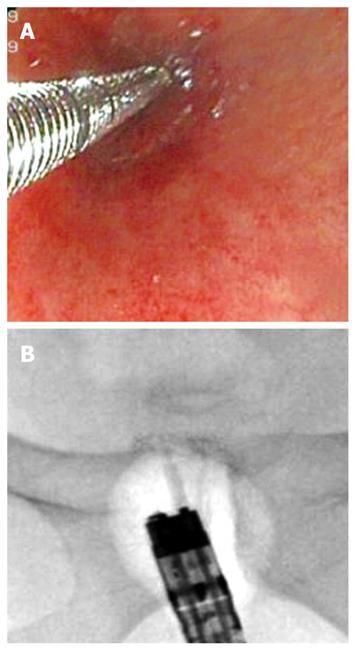
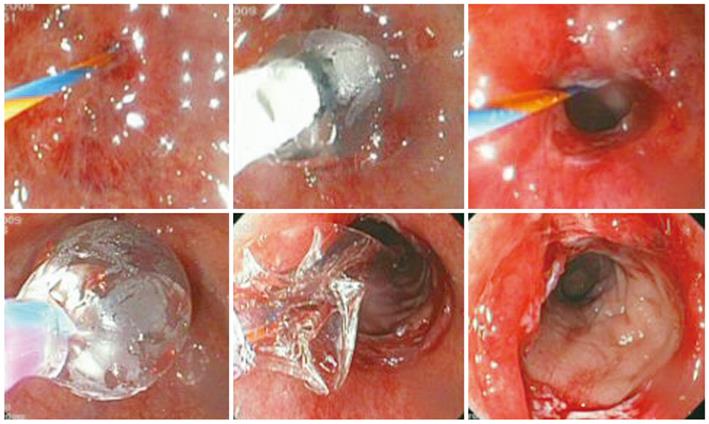
Two months later, the patient developed constipation and abdominal pain. Prior to ileostomy takedown, gastrografin enema through both the ileostomy and anus was performed, showing complete obstruction at the anastomotic site (Figure 1). To better confirm the entity and site of the obstruction, sigmoidoscopy was performed, showing an occlusive web completely obliterating the anastomosis (Figure 1). In order to avoid thermal injuries[8], we decided to use a new puncture catheter (Figure 2). This device is a specially designed polyethylene catheter (Artifon Catheter; SCITECH, Goiania, Brazil) with an 18-gauge needle and a flexible metallic sheath at the distal end, which allows puncture of the bile duct and insertion of a 0.025/0.0018-inch diameter guidewire. Sigmoidoscopy was performed using a therapeutic gastroscope (GIF-1TQ160, Olympus America Corp., Melville, NY, USA). On radiology, the lumen of the distal colon and proximal rectum, made apparent by air contrast, seemed to be continuous but completely separated at the anastomotic level. The Artifon catheter was inserted into the center of the circular staple line at the level of the anastomosis, under endoscopic and fluoroscopic control, and fluoroscopic identification of the proximal bowel was obtained with dye injection (Figure 3). A 0.025-inch guidewire (Tracer Metro, Cook Endoscopy, Winston-Salem, NC) was then passed through the catheter into the colon (Figures 3 and 4). Progressive pneumatic dilatation was performed over the guidewire with a 10 mm × 4 cm biliary balloon dilatation catheter (Hurricane RX 10 × 4, 5.8/180; Microvasive Endoscopy, Boston Scientific Corp. Natick, Mass) and, successively, with a controlled radial expansion balloon dilator (CRE™ Balloon Dilator, Boston Scientific Cork Ltd, Ireland) until a 2 cm diameter dilation was achieved (Figures 3 and 4). The successful destruction of the occlusive web facilitated passage of the colonoscope, allowing evaluation of the entire colon and stoma closure after three months of follow-up. The patient tolerated the procedure well, with no complications.
Benign colorectal anastomotic strictures are a challenging complication. Endoscopic dilatation is a valid and safe treatment, and is the preferred method for managing anastomotic colonic strictures, with surgery reserved for endoscopic failures. Endoscopic techniques center on the use of dilating balloons to disrupt scar tissue. Other techniques for endoscopic management include stricture incision with a needle knife, with or without balloon dilatation. In our report, we identified the proximal lumen by adapting a biliary approach to our aim. We used a suprapapillary biliary puncture catheter (Artifon Catheter®) to inject dye and insert a guidewire on which to perform balloon dilatation, without resorting to electrocision. This report highlights an alternative non-electrosurgical approach that uses a new device that proved to be safe and useful. However, it needs to be stressed that these procedures should be performed only by highly experienced endoscopists familiar with these specialized procedures.
Peer reviewers: Marc Basson, MD, PhD, MBA, Department of Surgery, Michigan State University, 1200 East Michigan Avenue, Suite #655, Lansing, MI 48912, United States; Patrick O’Dwyer, MB, BCh, BAO, FRCS (1), MCh, FRCS (Glasg), University Department of Surgery,Western Infirmary, Glasgow, G11 6NT, United Kingdom
S- Editor Tian L L- Editor OâNeill M E- Editor Ma WH
| 1. | Tuson JR, Everett WG. A retrospective study of colostomies, leaks and strictures after colorectal anastomosis. Int J Colorectal Dis. 1990;5:44-48. |
| 2. | Weinstock LB, Shatz BA. Endoscopic abnormalities of the anastomosis following resection of colonic neoplasm. Gastrointest Endosc. 1994;40:558-561. |
| 3. | Marchena Gómez J, Ruiz de la Cuesta E, Gómez Guerra G, Vallejo Gallego I, García-Anguíano F, Hernández Romero JM. Anastomotic stricture with the EEA-Stapler after colorectal anastomosis. Rev Esp Enferm Dig. 1997;89:835-842. |
| 4. | Di Giorgio P, De Luca L, Rivellini G, Sorrentino E, D’amore E, De Luca B. Endoscopic dilation of benign colorectal anastomotic stricture after low anterior resection: A prospective comparison study of two balloon types. Gastrointest Endosc. 2004;60:347-350. |
| 5. | Araujo SE, Costa AF. Efficacy and safety of endoscopic balloon dilation of benign anastomotic strictures after oncologic anterior rectal resection: report on 24 cases. Surg Laparosc Endosc Percutan Tech. 2008;18:565-568. |
| 6. | Hagiwara A, Sakakura C, Shirasu M, Torii T, Hirata Y, Yamagishi H. Sigmoidofiberscopic incision plus balloon dilatation for anastomotic cicatricial stricture after anterior resection of the rectum. World J Surg. 1999;23:717-720. |
| 7. | Mukai M, Kishima K, Iizuka S, Fukumitsu H, Fukasawa M, Yazawa N, Tajima T, Nakamura M, Makuuchi H. Endoscopic hook knife cutting before balloon dilatation of a severe anastomotic stricture after rectal cancer resection. Endoscopy. 2009;41 Suppl 2:E193-E194. |
| 8. | Morris ML, Tucker RD, Baron TH, Song LM. Electrosurgery in gastrointestinal endoscopy: principles to practice. Am J Gastroenterol. 2009;104:1563-1574. |