Published online Jul 28, 2010. doi: 10.3748/wjg.v16.i28.3601
Revised: May 27, 2010
Accepted: June 4, 2010
Published online: July 28, 2010
Cholelithiasis and choledocholithiasis occur frequently in pregnancy and their management can be complicated. Traditional endoscopic retrograde cholangiopancreatography (ERCP) is the first line treatment for choledocholithiasis, but in addition to its baseline risks, fluoroscopy poses an additional radiation risk to the fetus. Endoscopic ultrasound (EUS) is an accurate modality for detecting common bile duct stones, but its role has not been defined in pregnancy. We describe an alternative management strategy to conventional ERCP in a pregnant patient with choledocholithiasis and cholangitis detected using EUS and choledochoscopy.
- Citation: Girotra M, Jani N. Role of endoscopic ultrasound/SpyScope in diagnosis and treatment of choledocholithiasis in pregnancy. World J Gastroenterol 2010; 16(28): 3601-3602
- URL: https://www.wjgnet.com/1007-9327/full/v16/i28/3601.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i28.3601
We read with great interest the experiences of Fishman et al[1] in managing choledocholithiasis with choledochoscopy. Endoscopic ultrasound (EUS) is an accurate modality for detecting common bile duct (CBD) stones, but its role has not been defined in pregnancy. We describe an alternative management strategy to conventional endoscopic retrograde cholangiopancreatography (ERCP) in a pregnant patient with choledocholithiasis and cholangitis detected using EUS and choledochoscopy.
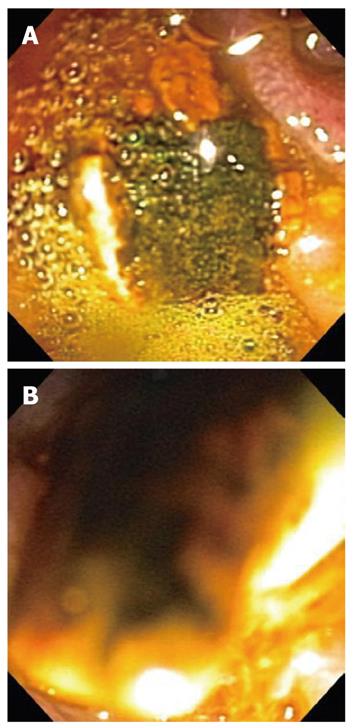
A 26-year old pregnant female at 28-wk gestation presented with right upper quadrant pain, progressive jaundice, and low-grade fever. Her past medical history was significant for sickle cell disease, preeclampsia and choledocholithiasis. She underwent a previous ERCP for stone removal after her last pregnancy. Upon presentation to the hospital, her total bilirubin was 6.8 mg/dL, aspartate transaminase 139 U/L, alanine transaminase 113 U/L, alkaline phosphatase 128 U/L and white blood cells count was 16 500/mm3. Transabdominal ultrasound revealed a 9-mm common bile duct with a possible filling defect. In order to avoid radiation exposure to fetus by fluoroscopy, EUS and choledochoscopy were used to examine the bile duct and achieve its complete clearance. The linear echoendoscope revealed multiple hyperechoic well-rounded stones throughout the common bile duct (Figure 1A). A prior sphincterotomy was performed, so deep cannulation of the bile duct using the SpyGlass choledochoscope (Boston Scientific) was easily achieved. The SpyScope was useful in determining the exact location of the stones. A guidewire was advanced through the SpyScope into the left intrahepatic system. A 10-mm extraction balloon was used to extract multiple yellow pigment stones from the CBD. The SpyScope was then reinserted and complete clearance of the CBD was confirmed (Figure 1B). A 10-Fr 5-cm plastic biliary stent was placed to ensure drainage and prevent recurrent cholangitis during the remainder of her pregnancy. The linear echoendoscope was used to confirm adequate placement of the biliary stent. Subsequently, the patient had complete resolution of symptoms and improvement in her liver enzymes.
The incidence of gallstones during pregnancy is estimated to be 3%-12%[2]. Symptomatic gallstone disease is the second most common abdominal emergency in pregnant women and may require surgical intervention. In addition to the baseline risks of ERCP, fluoroscopy poses an additional radiation risk to the fetus. Various publications have been reported on using ERCP during pregnancy without fluoroscopy by using bile aspiration for confirmation of CBD cannulation, sphincterotomy and balloon extraction of stones[3,4]. All these approaches are not perfect with regard to ensuring complete CBD clearance. This case highlights how choledochoscopy and endoscopic ultrasound are safe alternatives to fluoroscopy for the evaluation of biliary disorders during pregnancy. If choledochoscopy is not available, an alternative approach is to use EUS-guided extraction balloon sweeps to achieve clearance of ductal stones.
Peer reviewer: Dr. Ralf Jakobs, Professor, Director of the Department of Medicine C (Gastroenterology), Klinikum Ludwigshafen, Bremserstrasse 79, 67063 Ludwigshafen, Germany
S- Editor Tian L L- Editor Wang XL E- Editor Lin YP
| 1. | Fishman DS, Tarnasky PR, Patel SN, Raijman I. Management of pancreaticobiliary disease using a new intra-ductal endoscope: the Texas experience. World J Gastroenterol. 2009;15:1353-1358. |
| 2. | Ko CW, Beresford SA, Schulte SJ, Matsumoto AM, Lee SP. Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy. Hepatology. 2005;41:359-365. |
| 3. | Jamidar PA, Beck GJ, Hoffman BJ, Lehman GA, Hawes RH, Agrawal RM, Ashok PS, Ravi TJ, Cunningham JT, Troiano F. Endoscopic retrograde cholangiopancreatography in pregnancy. Am J Gastroenterol. 1995;90:1263-1267. |
| 4. | Simmons DC, Tarnasky PR, Rivera-Alsina ME, Lopez JF, Edman CD. Endoscopic retrograde cholangiopancreatography (ERCP) in pregnancy without the use of radiation. Am J Obstet Gynecol. 2004;190:1467-1469. |