Published online Jul 14, 2010. doi: 10.3748/wjg.v16.i26.3343
Revised: March 18, 2010
Accepted: March 25, 2010
Published online: July 14, 2010
We report a male patient with prolonged post-prandial abdominal distension and a sudden onset of epigastric pain initially diagnosed as acute abdomen. The patient had no history of surgery. Physical examination revealed peritonitis and abdominal computed tomography scan showed upper abdominal mesentery intorsion. The patient then underwent surgical intervention. It was found that the descending mesocolon dorsal root was connected to the ascending colon and formed a membrane encapsulating the small intestine. The membrane also formed an orifice in the ileal pars caeca, from which a 30 cm herniated ileum formed a “C”-shaped loop which was strangulated by the orifice. An abdominal separation was diagnosed after surgery. We liberated the membranous peritoneum which incarcerated the intestinal canal from the root of ileocecal junction to Treitz ligament, and reduced the small intestinal malrotation. The patient had an uneventful recovery after operation with his abdominal distention disappeared during the follow-up. Abdominal separation is a rare situation, which may be related with embryo development. Surgery is a choice of treatment for it.
- Citation: Liu BL, Chen Y, Liu SQ, Zhang XB, Cui DX, Dai XW. Abdominal separation in an adult male patient with acute abdominal pain. World J Gastroenterol 2010; 16(26): 3343-3346
- URL: https://www.wjgnet.com/1007-9327/full/v16/i26/3343.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i26.3343
Acute abdominal pain, a common chief complaint encountered in emergency department, accounts for about 5% of all emergency department visits[1] and can be caused by a variety of conditions[2]. Many factors can result in acute abdominal pain, such as appendicitis, bowel obstruction, and cholecystitis[3]. This report describes a rare case of abdominal separation in an adult male patient with strangulated internal hernia of the terminal ileum complicating malrotation of intestine, which has not been reported in the literature.
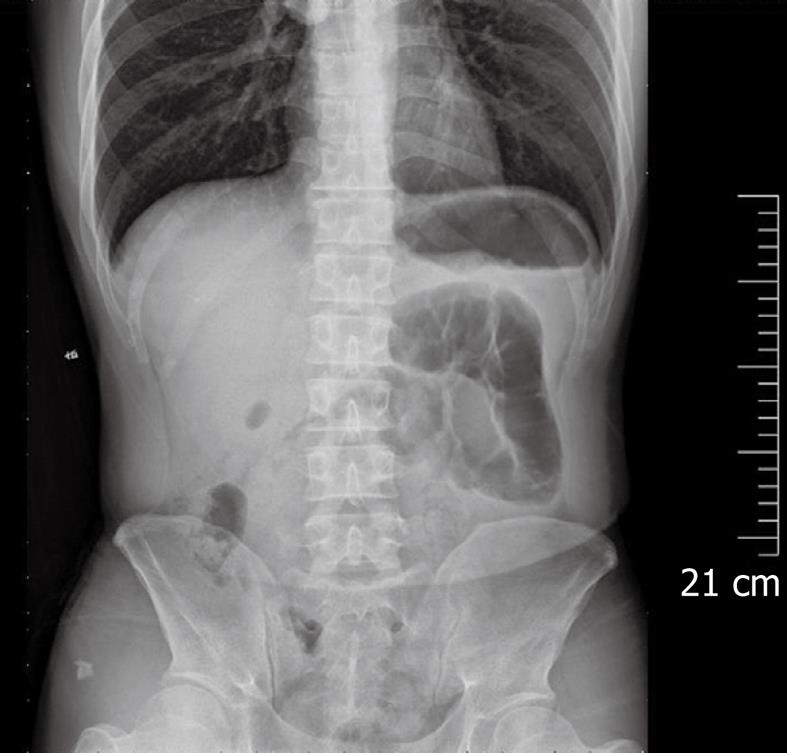
A 43-year-old man visited the emergency department of our hospital on December 31, 2007 for a sudden onset of persistent epigastric pain for 10 h. He had a history of prolonged episodes of postprandial abdominal distension. The pain was associated with nausea and vomiting without any clear inducing factors, and did not radiate to the back and shoulders. The symptoms included anorexia, constipation, obstipation and poor sleep. Furthermore, he had no history of abdominal surgery or trauma. On admission, his temperature was 36.5°C, blood pressure was 127/72 mmHg, respiratory rate and pulse rate were 17 breaths/min and 70 beats/min, respectively. Physical examination showed tenderness, rebound tenderness and slight muscular rigidity in the right lower quadrant of abdomen. Laboratory findings included 86.8% of neutrophils and 116.0 U/L of hemoglobin. Plain abdominal X-ray revealed mildly dilated pneumatic intestinal canal loops but no typical air-fluid level shadow in the left upper quadrant of abdomen (Figure 1). The patient was initially diagnosed as localized peritonitis which was differentially diagnosed from acute appendicitis and intestinal mesentery intorsion.
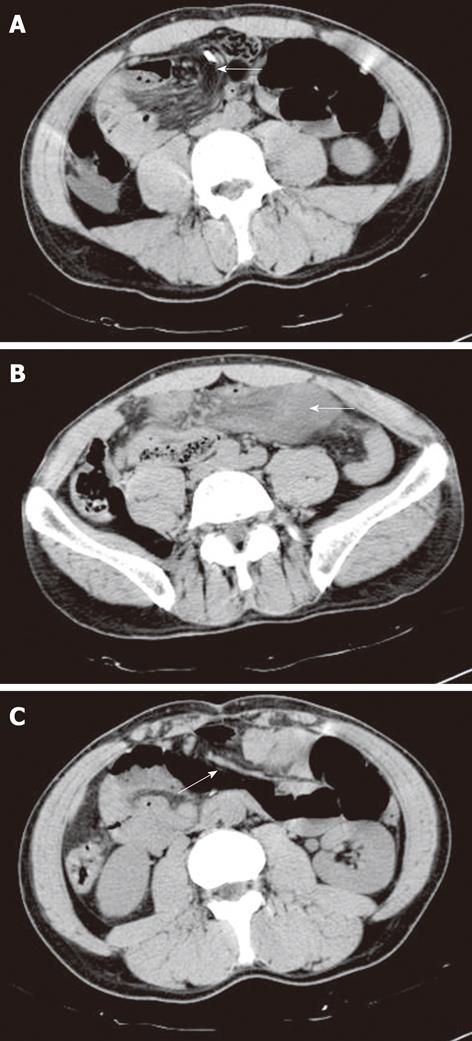
The patient had no significant improvement after initial treatment with fluid replacement, antibiotics and gastrointestinal decompression. He developed peritonitis with the pain exacerbated. Computed tomography (CT) scan revealed suspicious upper abdominal mesentery intorsion (Figure 2). Exploratory laparoscopy demonstrated appendix in the retroileal position, descending mesocolon dorsal root that was connected to the ascending colon encapsulating the small intestine, an orifice in the ileal pars caeca from which a 30 cm herniated ileum formed a “C”-shaped loop at the root of ileocecal junction strangulating at the orifice, and a purple incarcerated intestinal canal.
We liberated the incarcerated intestinal canal by opening the membrane at the mesentery root from the ileocecal junction to Treitz ligament and reduced the mesoileal malrotation. The strangulated intestine was about 50 cm from the ileocecal junction. After liberation, the intestinal canal was recovered with its color changed from purple to pink, and vascular pulsation was obvious and peristalsis was resumed.
The patient had an uneventful recovery and was discharged on January 8, 2008. The patient was diagnosed as localized peritonitis, small intestinal malrotation, internal herniation, strangulation of small bowel and abdominal separation after operation, and followed up for 18 mo during which no complications and post prandial abdominal distention occurred.
Since a large number of patients visiting emergency department complain of acute abdominal pain and most of them have typical symptoms and signs, appropriate evaluation can be accomplished with the aid of relevant auxiliary investigations[3]. The complaints are usually relieved after symptomatic treatment. In some rare cases, its initial diagnosis may be difficult as in our case. The incidence of internal hernia is low, accounting for less than 1% of all acute abdomen cases[4-6]. However, the overall mortality may be higher than 50% if it is not appropriately treated, especially when strangulation occurs. A fast and correct diagnosis is therefore necessary.
Our patient suffered from abdominal pain which exacerbated although it was treated with fluid resuscitation and antibiotics. Nasogastric tube decompression did not produce desirable effect and vomiting continued. Since the condition was nonspecific, its differential diagnosis was difficult from acute abdomen caused by factors such as mechanical intestinal obstruction. Plain abdominal X-ray has been recommended for patients with highly suspected obstruction[7-9] according to The Royal College of Radiologists Guidelines[10]. A single plain abdominal X-ray is not adequate to make a definitive judgment of suspected obstruction[9], and CT scan is the reasonable next step for further investigation of abdomen[2,11]. Abdominal CT scan has a good inter-observer agreement in unselected patients with acute abdominal pain at emergency department and plays an important role in diagnosis of acute intestinal obstruction and in planning of surgical treatment. Although internal hernias are uncommon, they should be included in the differential diagnosis from intestinal obstruction, especially in the absence of abdominal surgery or trauma. Recognition of the characteristic findings on CT scan may assist in identification of internal hernias in most cases of small bowel obstruction. Since the general condition of this patient deteriorated very quickly and CT revealed a mesentery intorsion, surgery was performed. The function of strangulated bowel was recovered after its loop was released and the mesenteric malrotation was reduced.
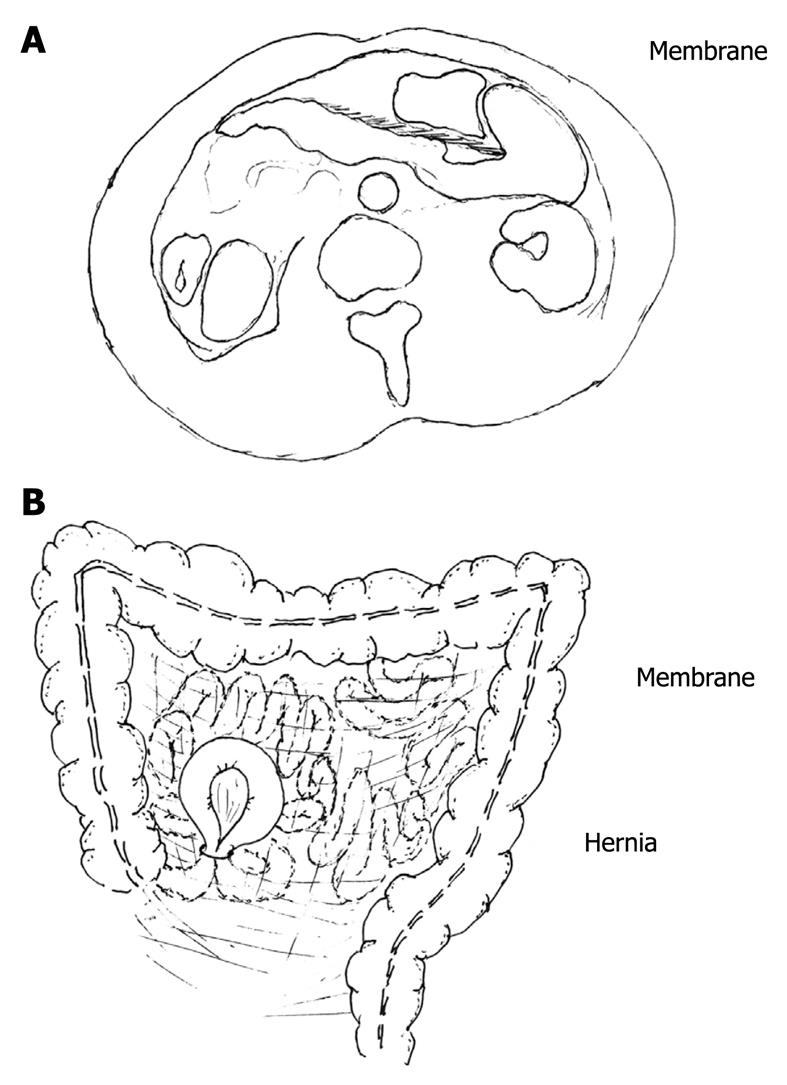
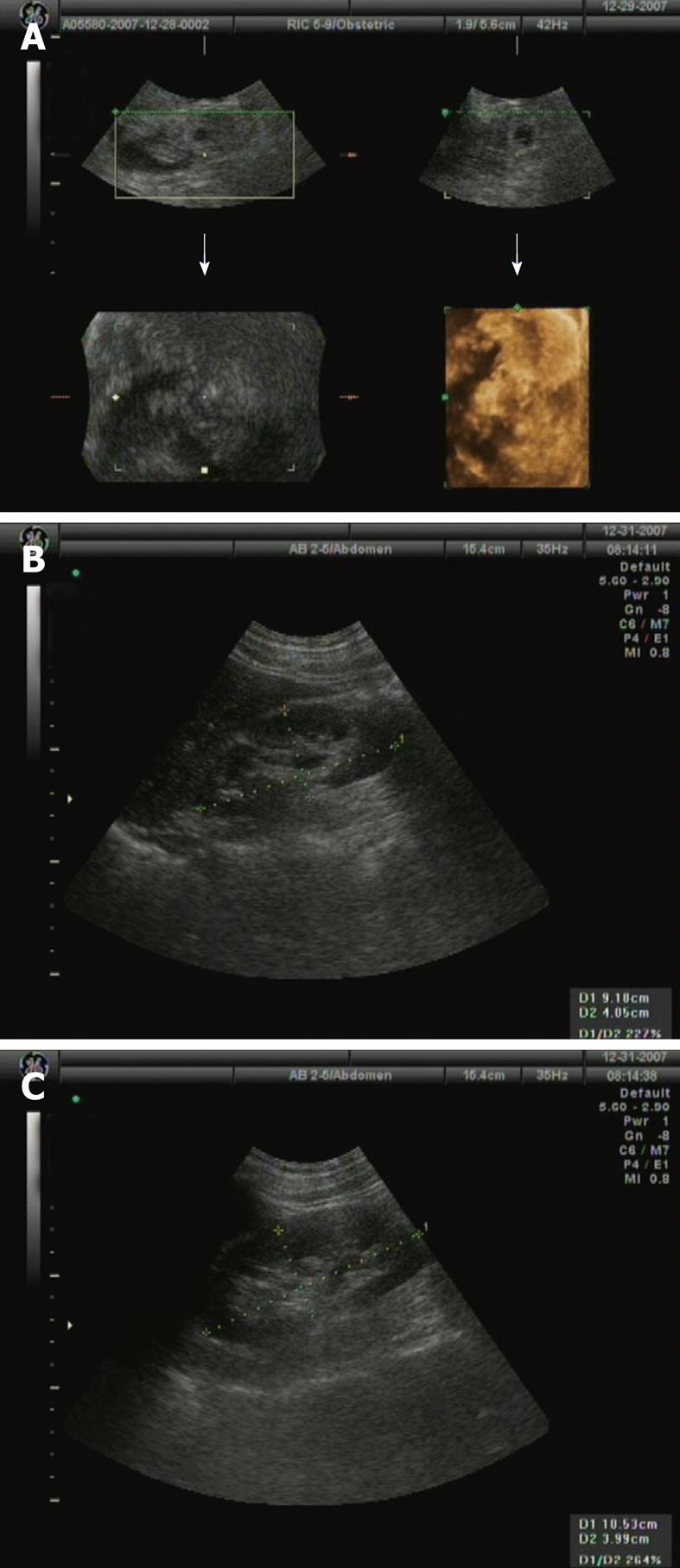
Although abdominal separation in our case could not be definitely diagnosed before operation by the radiologist and clinician[8] due to the presence of peritonitis, surgery was performed during which the otherwise rare phenomenon of abdominal separation was discovered, namely a membrane divides the abdominal cavity into two compartments. The anterior compartment contains the colon, while the posterior compartment encapsulates the small intestine, forming an orifice at the end of ileocecal junction. It is at this orifice that a 30 cm ileum is protruded and strangulates the anterior compartment, causing abdominal pain. A CT scan showed an intra-abdominal membrane-like line dividing the two compartments (Figures 2 and 3). Ultrasonography did not show specific intraabdominal evidence (Figure 4). This patient experienced episodes of post prandial abdominal distension, which supported the findings on abdominal CT scan and at operation. His symptoms were relieved after operation. We therefore recommend that abdominal separation should be differentially diagnosed from acute abdomen. Early diagnosis and operation will greatly reduce the morbidity and mortality of intestinal strangulation.
The intestine has returned to the abdominal cavity and the midgut consisting mainly of the duodenum, jejunum, ileum, ascending colon, and transverse colon has completed its 270-degree loop by weeks 10 and 20 of embryo development, respectively. With the growth of small intestine, the ascending and descending colon are pushing against the body wall in a secondary retroperitoneal location like the pancreas and duodenum[12,13]. Whether the mesentery separates abdomen into two parts of peritonum during the development is not well known. Whether there is any genetic change needs to be further investigated.
In conclusion, abdominal separation with internal hernias is a rare condition that can present as acute abdomen. Such patients can recover if they are properly treated. We strongly recommend that abdominal separation should be differentially diagnosed from acute abdomen.
Peer reviewer: Yasuhiro Fujino, MD, PhD, Director, Department of Surgery, Hyogo Cancer Center, 13-70 Kitaoji-cho, Akashi, 673-8558, Japan
S- Editor Wang JL L- Editor Wang XL E- Editor Zheng XM
| 1. | Kamin RA, Nowicki TA, Courtney DS, Powers RD. Pearls and pitfalls in the emergency department evaluation of abdominal pain. Emerg Med Clin North Am. 2003;21:61-72, vi. |
| 2. | van Randen A, Laméris W, Nio CY, Spijkerboer AM, Meier MA, Tutein Nolthenius C, Smithuis F, Bossuyt PM, Boermeester MA, Stoker J. Inter-observer agreement for abdominal CT in unselected patients with acute abdominal pain. Eur Radiol. 2009;19:1394-1407. |
| 3. | Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77:971-978. |
| 4. | Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186:703-717. |
| 5. | Selçuk D, Kantarci F, Oğüt G, Korman U. Radiological evaluation of internal abdominal hernias. Turk J Gastroenterol. 2005;16:57-64. |
| 6. | Varela GG, López-Loredo A, García León JF. Broad ligament hernia-associated bowel obstruction. JSLS. 2007;11:127-130. |
| 7. | Ahn SH, Mayo-Smith WW, Murphy BL, Reinert SE, Cronan JJ. Acute nontraumatic abdominal pain in adult patients: abdominal radiography compared with CT evaluation. Radiology. 2002;225:159-164. |
| 8. | Thompson WM, Kilani RK, Smith BB, Thomas J, Jaffe TA, Delong DM, Paulson EK. Accuracy of abdominal radiography in acute small-bowel obstruction: does reviewer experience matter? AJR Am J Roentgenol. 2007;188:W233-W238. |
| 9. | Smith JE, Hall EJ. The use of plain abdominal x rays in the emergency department. Emerg Med J. 2009;26:160-163. |
| 10. | Remedios D, McCoubrie P, The Royal College Of Radiologists Guidelines Working Party. Making the best use of clinical radiology services: a new approach to referral guidelines. Clin Radiol. 2007;62:919-920. |
| 11. | Takeyama N, Gokan T, Ohgiya Y, Satoh S, Hashizume T, Hataya K, Kushiro H, Nakanishi M, Kusano M, Munechika H. CT of internal hernias. Radiographics. 2005;25:997-1015. |
| 12. | Cochard LR. Netter's atlas of human embryology. Teterboro: Icon Learning Systems 2002; 140-141. |
| 13. | Israelit S, Brook OR, Nira BR, Guralnik L, Hershko D. Left-sided perforated acute appendicitis in an adult with midgut malrotation: the role of computed tomography. Emerg Radiol. 2009;16:217-218. |