Published online Jul 14, 2010. doi: 10.3748/wjg.v16.i26.3339
Revised: March 12, 2010
Accepted: March 19, 2010
Published online: July 14, 2010
We report a case of 71-year-old man who developed a hypersensitivity syndrome associated with terbinafine. He was placed on terbinafine (250 mg/d) for the treatment of tinea pedis due to diabetes mellitus. Following the treatment with terbinafine, he developed drug-induced hypersensitivity syndrome (DIHS). Systemic corticosteroid led to transient improvement of his clinical manifestations. Three months after disease onset, he presented with panperitonitis due to ileal perforation, and underwent an emergency operation. The affected ileum was resected and ileostomy was performed in the terminal ileum. Cytomegalovirus (CMV)-specific IgG antibodies were significantly increased, high-titer CMV antigenemia was detected, and pathological examination of the resected ileum confirmed CMV infection. Based on these observations, we strongly recommend that physicians monitor reactivation of the family of herpesvirus other than herpesvirus 6, to manage DIHS properly.
- Citation: Sano S, Ueno H, Yamagami K, Yakushiji Y, Isaka Y, Kawasaki I, Takemura M, Inoue T, Hosoi M. Isolated ileal perforation due to cytomegalovirus reactivation during management of terbinafine hypersensitivity. World J Gastroenterol 2010; 16(26): 3339-3342
- URL: https://www.wjgnet.com/1007-9327/full/v16/i26/3339.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i26.3339
Terbinafine has become established as a drug of choice to treat onychomycosis and other dermatomycoses. Although previously reported cases of drug-induced hypersensitivity syndrome (DIHS) are notably uncommon (anticonvulsants, salazosulfapyridine, allopurinol, minocycline, and mexiletine), the number of reported cases of DIHS induced by terbinafine has been increasing.
It is true human herpesvirus 6 (HHV-6) reactivation has been the most frequently described infection associated with this syndrome, but recent articles have suggested that certain herpesviruses other than HHV-6 might be reactivated in a sequential manner in the development of DIHS (multiple and sequential herpesvirus reactivation)[1-7].
Although rare, cytomegalovirus (CMV) is known to cause ileal perforation, not only in immunocompromised patients such as those with the acquired immunodeficiency syndrome (AIDS) but also immunocompetent patients[8-11]. To the best of our knowledge, especially in the English-language literature, isolated cases of ileal perforation due to CMV infection have never been reported in patients with DHIS.
Here, we report a case of isolated ileal perforation due to CMV in a case of DIHS due to terbinafine, in whom reactivation of HHV-6, Epstein-Barr virus (EBV) and CMV was detected.
A 71-year-old Japanese man with diabetes mellitus with onychomycosis was treated with oral terbinafine. Other medical history was not remarkable: any anticonvulsants, mexiletine, and antibiotics such as minocycline and salazosulfapyridine, were not prescribed. One week after taking terbinafine, he developed a high fever, erythema covering the whole body, and superficial lymph node swelling. Laboratory data at that time showed leukocytosis (16 670/mm3) with 30.2% eosinophils. Atypical lymphocytes were not present. Liver enzymes were slightly elevated: 47 IU/L alanine aminotransferase and 78 IU/L aspartate aminotransferase. DIHS was suspected and terbinafine administration was discontinued soon after the onset of illness. As a result of sustained fever and erythroderma for 1 mo, 30 mg/d systemic corticosteroid was started. After 7 d, his symptoms improved temporarily. However, tapering the corticosteroid dose to 25 mg/d led to recrudescence of his fever and generalized rash (on day 50). Other results of systemic corticosteroids were not remarkable. Retrospectively, seroconversion of anti-HHV-6 antibody was detected; the titer increased from < 10 (on day 14) to 40 (on day 90). Judging from his drug history, characteristic generalized erythematous rash and laboratory data, the diagnosis of DIHS was confirmed. He was again administrated 30 mg/d prednisolone from day 50. Then, the patient was referred to our hospital (Osaka City General Hospital).
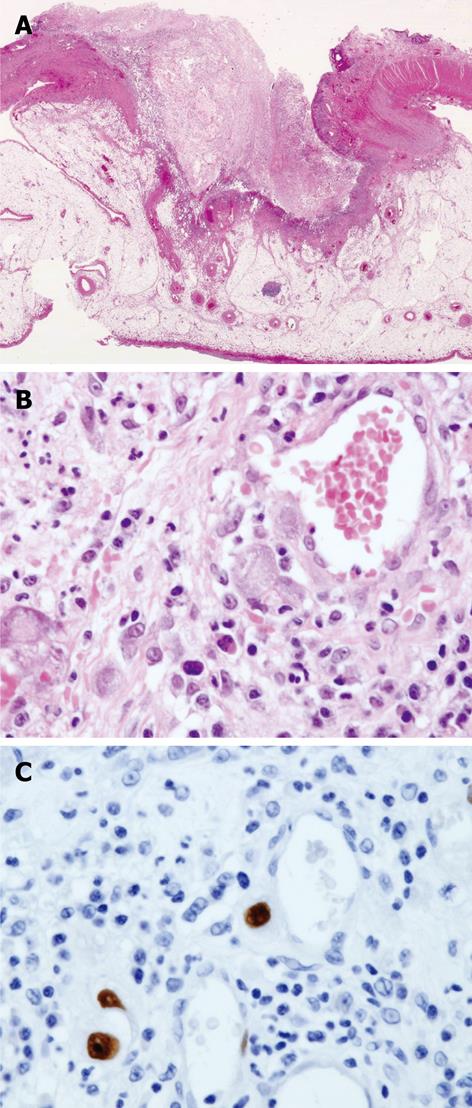
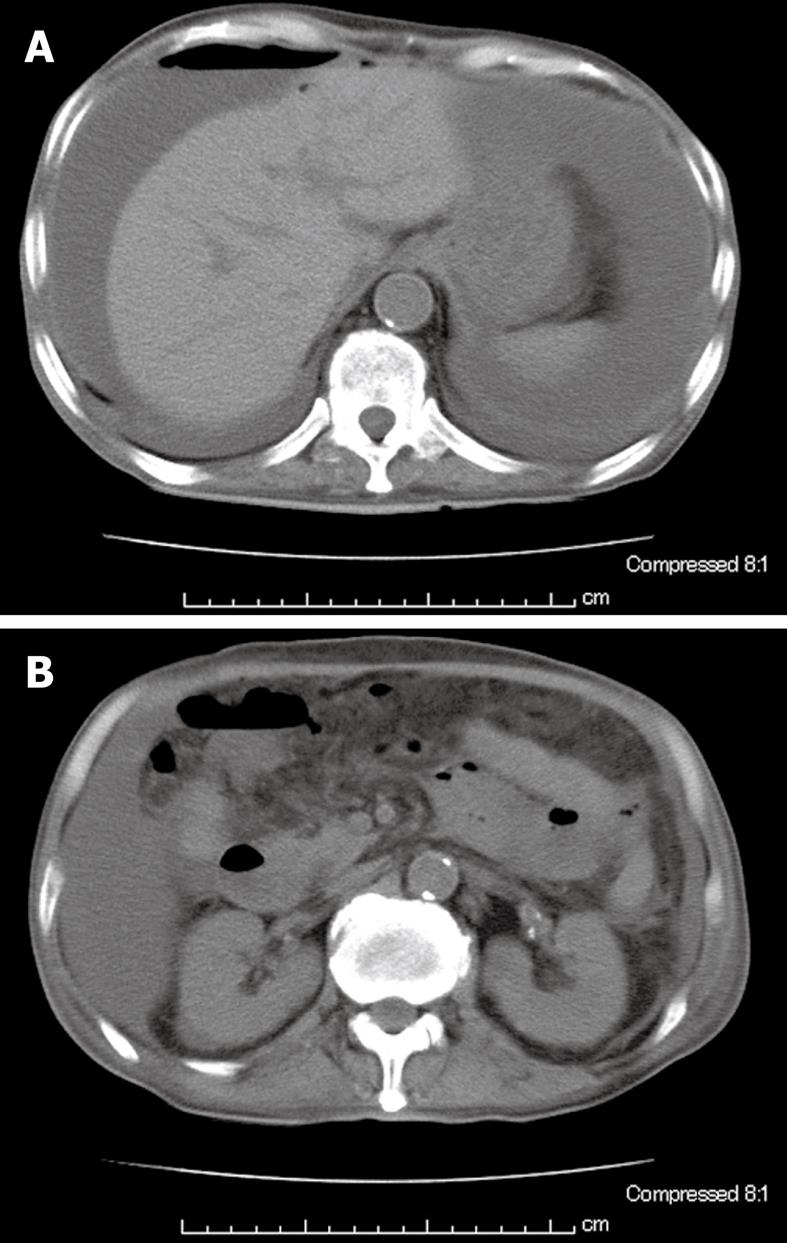
Examination on admission revealed erythematous rash over his entire body, with partially exfoliated lesions and superficial lymphadenopathy. Laboratory data included a normal count of white blood cells without eosinophilia and normal liver enzymes. Antinuclear and antineutrophil cytoplasmic antibodies were negative. The patient was negative for human immunodeficiency virus (HIV). Histological examination of the skin was not performed. Seventy days after the onset of DIHS, the patient complained of abdominal discomfort, and occult blood tests were positive on two occasions. On day 80, colonoscopic examination was performed and no abnormality around the whole colon and terminal ileum was revealed. At that time, CMV antigenemia was strongly suggested by the direct detection of viral antigen in the peripheral blood: CMV antigenemia-1, 56 and antigenemia-2, 89. CMV IgG titer increased to 128 and IgM titer was negative (< 0.8). Intravenous administration of 500 mg/d ganciclovir was started. However, fever with abdominal pain was present on day 82, and physical examination showed muscular defense in the entire abdomen. Abdominal computed tomography (CT) revealed free air, ascites, and swelling of the ileal loop (Figure 1). He was diagnosed as having panperitonitis due to ileal perforation, and underwent an emergency operation. The affected ileum was resected and ileostomy was performed. Pathological examination of the resected ileum revealed acute inflammation with vasculitis and CMV inclusions in the macrophages and endothelial cells, and evidence of CMV on immunostaining (Figure 2). There was no evidence of cancer cells or any other pathogens. Administration of 500 mg/d ganciclovir was continued, and CMV antigenemia was not detected on day 89. Unfortunately, the patient died from pneumonia.
Terbinafine has become established as a drug of choice to treat onychomycosis and other dermatomycoses. Although previously reported cases of DIHS are notably uncommon (anticonvulsants, salazosulfapyridine, allopurinol, minocycline, and mexiletine), the number of reported cases of DIHS induced by terbinafine has been increasing. It was thought that the present case met the criteria for DIHS because the patient had clear exposure to a given drug (in this case, terbinafine), high fever (> 39°C); erythroderma followed by exfoliative dermatitis; diffuse lymphadenopathy; and hypereosinophilia (absolute eosinophil count, 5032/mm3). The results of a lymphocyte-stimulating test for terbinafine performed in our hospital were negative, and it was thought that treatment with prednisolone may have affected the results.
Since Aihara et al[2] in 2001, it has been recognized that CMV is associated with hypersensitivity syndrome. Recent studies have suggested that reactivation of members of the herpesvirus family other than HHV-6 could be associated with DIHS. Moreover, multiple herpesvirus reactivations and sequential reactivation have been reported in the case of DIHS. The list of viruses that have been documented to be reactivated include HHV-6, HHV-7, EBV and CMV[2-7]. In the present case, reactivation of HHV-6, EBV and CMV was confirmed on the basis of serological tests on paired serum samples for HHV-6 and EBV, and polymerase chain reaction for CMV. EBV reactivation was asymptomatic, which might have been due to administration of corticosteroids.
The clinical course of this patient can be divided in three phases: (1) hypersensitivity reaction with eosinophilia; (2) relapse of fever and rash due to HHV-6 reactivation; and (3) ileal perforation due to CMV reactivation. Retrospectively, the worsening of exanthema and poor control of second fever in spite of treatment with prednisolone reflect virus reactivation. We speculate that the virus responsible for this phase was HHV-6, although we could not confirm the absence of CMV infection in this period. The following abdominal pain and ileal perforation was due to CMV reactivation, as confirmed by pathological examination of the resected ileum.
Our patient was unique in that CMV reactivation resulted in ileal perforation during the course of DIHS. Although rare, CMV is known to cause ileal perforation, especially in immunocompromised patients, such as those with AIDS. To the best of our knowledge, isolated cases of ileal perforation due to CMV infection have never been reported in a patient with DIHS (Table 1)[8-11]. Although it remains possible that systemic corticosteroid administration precipitated CMV reactivation, there is also a case report that demonstrated that a patient without any corticosteroids showed reactivation of HHV-6, HHV-7 and CMV[3]. Based on these observations, it is important for physicians to be aware of the possible reactivation of CMV and other herpesviruses in every patient with DIHS, to avoid awkward small intestinal ulcer and perforation.
| AIDS |
| Non-Hodgkin’s lymphoma with chemotherapy |
| Systemic lupus erythematosus |
| Liver transplantation |
| Ulcerative colitis |
| Recurrent gastric cancer |
| Blood transfusion associated with trauma |
| Immunocompetent elderly/neonatal |
| DIHS (present case) |
In summary, we have reported a case of isolated ileal perforation due to CMV reactivation during the management of terbinafine hypersensitivity. Although the prognosis in bowel perforation related to CMV infection is extremely poor, emergency surgery saved our patient’s life. However, earlier diagnosis and prompt administration of antiviral drugs could have avoided surgical treatment. Although CMV could affect multiple organ functions and might be the direct cause of death, effective medication such as ganciclovir is available. Therefore, it is strongly recommended that physicians monitor reactivation of herpesviruses other than HHV-6, to manage DIHS properly.
Peer reviewer: NKH de Boer, PhD, MD, Gastroenterology and Hepatology, VU University Medical Center, PO Box 7057, 1007 MB, Amsterdam, The Netherlands
S- Editor Wang YR L- Editor Kerr C E- Editor Ma WH
| 1. | Komura K, Hasegawa M, Hamaguchi Y, Yukami T, Nagai M, Yachie A, Sato S, Takehara K. Drug-induced hypersensitivity syndrome associated with human herpesvirus 6 and cytomegalovirus reactivation. J Dermatol. 2005;32:976-981. |
| 2. | Aihara M, Sugita Y, Takahashi S, Nagatani T, Arata S, Takeuchi K, Ikezawa Z. Anticonvulsant hypersensitivity syndrome associated with reactivation of cytomegalovirus. Br J Dermatol. 2001;144:1231-1234. |
| 3. | Kano Y, Hiraharas K, Sakuma K, Shiohara T. Several herpesviruses can reactivate in a severe drug-induced multiorgan reaction in the same sequential order as in graft-versus-host disease. Br J Dermatol. 2006;155:301-306. |
| 4. | Aihara M, Sugita Y, Takahashi S, Nagatani T, Arata S, Takeuchi K, Ikezawa Z. Anticonvulsant hypersensitivity syndrome associated with reactivation of cytomegalovirus. Br J Dermatol. 2001;144:1231-1234. |
| 5. | Descamps V, Mahe E, Houhou N, Abramowitz L, Rozenberg F, Ranger-Rogez S, Crickx B. Drug-induced hypersensitivity syndrome associated with Epstein-Barr virus infection. Br J Dermatol. 2003;148:1032-1034. |
| 6. | Sekiguchi A, Kashiwagi T, Ishida-Yamamoto A, Takahashi H, Hashimoto Y, Kimura H, Tohyama M, Hashimoto K, Iizuka H. Drug-induced hypersensitivity syndrome due to mexiletine associated with human herpes virus 6 and cytomegalovirus reactivation. J Dermatol. 2005;32:278-281. |
| 7. | Arakawa M, Kakuto Y, Ichikawa K, Chiba J, Tabata N, Sasaki Y. Allopurinol hypersensitivity syndrome associated with systemic cytomegalovirus infection and systemic bacteremia. Intern Med. 2001;40:331-335. |
| 8. | Meza AD, Bin-Sagheer S, Zuckerman MJ, Morales CA, Verghese A. Ileal perforation due to cytomegalovirus infection. J Natl Med Assoc. 1994;86:145-148. |
| 9. | Bang S, Park YB, Kang BS, Park MC, Hwang MH, Kim HK, Lee SK. CMV enteritis causing ileal perforation in underlying lupus enteritis. Clin Rheumatol. 2004;23:69-72. |
| 10. | Yasunaga M, Hodohara K, Uda K, Miyagawa A, Kitoh K, Andoh A, Okabe H, Ochi Y, Fujiyama Y, Bamba T. Small intestinal perforation due to cytomegalovirus infection in patients with non-Hodgkin's lymphoma. Acta Haematol. 1995;93:98-100. |
| 11. | Van Schaeybroeck S, Hiele M, Miserez M, Croes R. Ileal perforation caused by cytomegalovirus infection in an immunocompetent adult. Acta Clin Belg. 2002;57:154-157. |