Published online Jul 14, 2010. doi: 10.3748/wjg.v16.i26.3305
Revised: May 9, 2010
Accepted: May 16, 2010
Published online: July 14, 2010
AIM: To describe patient characteristics and the results of surgical treatment for hepatic hydatidosis (HH) in the Hospital Hernán Henríquez Aravena from December 2001 to March 2005.
METHODS: Subjects older than 16 years with suspected HH were included based on the clinical picture and radiological studies. Variables examined included clinical and laboratory aspects, outcome, features of the parasite and surgical aspects. Descriptive statistics were used, calculating central tendency, dispersion and extreme tendency.
RESULTS: The series was comprised of 122 patients, with an average age of 44 ± 16.9 years. The most frequently used surgical technique was subtotal cystectomy in 90% of the patients, followed by hepatic resection (hepatectomy, segmentectomy and subsegmentectomy) in 5%. In 2%, a combination of subtotal cystectomy and segmentectomy was performed. In addition, 28% of the series presented complications in the postoperative period and mortality was 2%.
CONCLUSION: The most frequently used surgical technique for HH was subtotal cystectomy and the morbidity and mortality rates in this Chilean series are comparable to other national and international series.
- Citation: Losada Morales H, Burgos San Juan L, Silva Abarca J, Muñoz Castro C. Experience with the surgical treatment of hepatic hydatidosis: Case series with follow-up. World J Gastroenterol 2010; 16(26): 3305-3309
- URL: https://www.wjgnet.com/1007-9327/full/v16/i26/3305.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i26.3305
Hepatic hydatidosis (HH) is a zoonosis produced by Equinococcus granulosus that presents a high prevalence and incidence in southern Chile, at a rate of 38 per 100 000[1-2]. There are many options for HH treatment. Based on World Health Organization guidelines and our experience, surgery is one of the most effective treatments for HH[3-5].
There is a wide range of surgical techniques for treating HH, from radical surgery with complete removal of the cyst leaving no residual cavity (pericystectomy or regulated hepatic resection), to more conservative techniques with partial removal of the cyst and treatment of that part of the cyst remaining in the hepatic parenchyma: subtotal cystectomy plus epiploplasty, subtotal cystectomy plus capitonnage, cystostomy plus epiploplasty, among others[3-12]. Some reports show that epiploplasty decreases the incidence of deep abdominal abscess after surgical treatment[10-12].
The surgical technique preferred by our team is subtotal cystectomy, leaving the smallest amount of cyst in the hepatic parenchyma, accompanied by epiploplasty[11,12]. Performing complete dissection of the liver’s ligamentous attachments we can thus provide even better exposure for resection of the cyst, only leaving the part close to vascular structures.
Our hypothesis is that morbidity and mortality rates associated with the surgical treatment of HH in the Hospital Hernán Henríquez Aravena, Temuco, Chile, are comparable to national and international figures. Our aim is to describe patient characteristics, the results of the surgical treatment and the morbidity and mortality associated with the surgical treatment of HH in the Hospital Hernán Henríquez Aravena from December 2001 to March 2005.
Patients were subjects older than 16 years with suspected HH based on the clinical findings and radiological studies which were performed in Hospital Hernán Henríquez Aravena (Temuco, Chile) from December 2001 to March 2005. Our protocol did not include preoperative albendazole.
Subtotal cystectomy: Surgical technique in which part of the adventitious membrane of the hydatid cyst is resected. In this technique, we only leave the part of the adventitia adjacent to the vascular structures. When possible, this part is covered by a vascularized omental flap (epiploplasty).
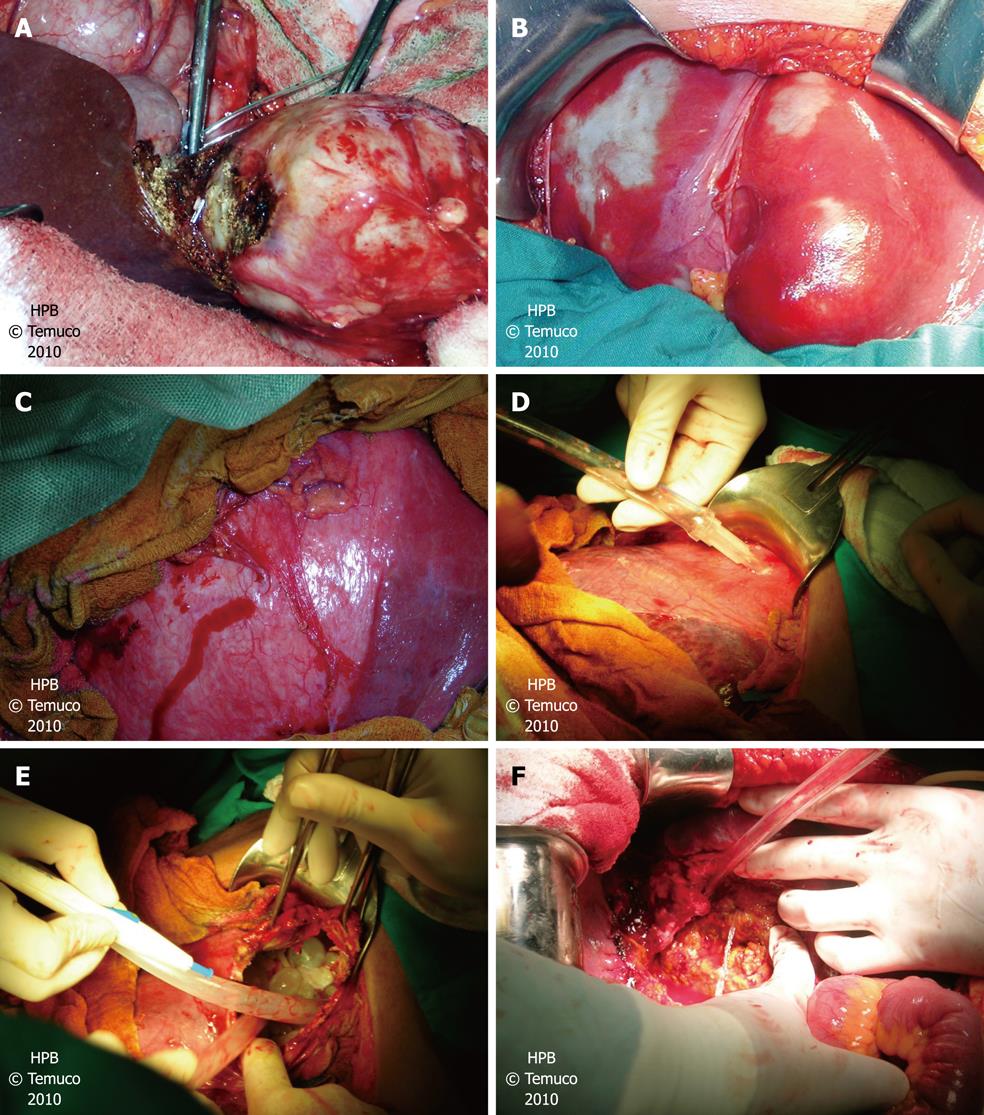
Pericystectomy: Total resection of the cyst’s adventitious membrane, in which the plane between the adventitious membrane and hepatic parenchyma is dissected. This technique is used for peripheral cysts and is performed with afferent vascular control (Figure 1A).
The biliopancreatic surgery team prefers to treat HH via the abdomen no matter where the cysts are located. A subcostal laparotomy is used, either right or bilateral, depending on the location of the cysts; or a J laparotomy towards the right. The round ligament is sectioned and tied off and the liver is then moved to locate the cyst (Figure 1B). On some occasions, intraoperative echography is used when cysts are difficult to locate. Once a cyst has been located, we protect the surgical area with compresses containing either diluted povidone or 20% hypertonic saline solution as per the surgeon’s choice (Figure 1C). The cyst is subsequently punctured and all the hydatid fluid and daughter vesicles are aspirated (Figure 1D and E). The germinative membrane is removed and the protection field withdrawn. Depending on the location, the subtotal cystectomy is planned, beginning the resection of the cyst wall with electrocoagulation, controlling the hemostasia, leaving only that part of the cyst which is adjacent to the vascular structures. This area is then reviewed in search of biliary communications, which are sutured with 3-0 resorbable material. Some team members perform a cholecystectomy and they inject physiological serum into the cystic duct through a nelaton probe to make small biliary communications visible (Figure 1F). Depending on the number of communications, satisfaction with the closing of the communications and the diameter of the bile duct, a choledochostomy is performed. The only absolute indication for a choledochostomy is a clinical picture compatible with cholangiohydatidosis, in which the bile duct is always drained. Nevertheless, in recent months, we have tried to drain the bile duct using endoscopic retrograde cholangiography. An epiploplasty is subsequently performed with a greater omentum pedicle flap. Drains are not positioned as a matter of course and are at the surgeon’s discretion.
Variables examined included clinical and laboratory features, clinical images and evolutionary complications, surgical and clinical evolution variables.
Variables examined included ultrasound (US) and computed tomography (CT) characteristics of the cyst, the number of cysts (continuous variable), location of the cysts (categorized into right hemi-liver, left hemiliver, bilateral or central liver), diameter of the lesion, evolutionary complications of the cyst (hepatic abscess of hydatid origin (HAH), hepatothoracic transit (HHT), rupture to the abdominal cavity and cholangiohydatidosis.
Surgical variables: The substance used to protect the surgical area is considered (povidone and/or hypertonic solution), as is the surgical technique (categorized into subtotal cystectomy, pericystectomy, segmentectomy and hepatectomy). The use of choledochostomy and/or drain (dichotomized: yes or no) is evaluated.
Clinical evolution variables: The duration of hospitalization is assessed, and the presence of postoperative complications (categorized into: residual cavity, infection of the operating site, atelectasis, pneumonia, hemoperitoneum, bilioperitoneum, evisceration and pneumothorax).
Abscess in the residual cavity is defined as any purulent collection in relation to the liver surgical bed that needs treatment (surgery or CT-guided drainage).
Postoperative follow-up was carried out by clinical assessment. For any abnormal finding US or CT was undertaken. Liver recurrence was defined as any cyst image (such as hydatid cyst) with postoperative normal images.
Descriptive statistics were used, calculating measures of central tendency (mean, median) dispersion (SD) and extreme values. Database was analyzed using the program Stata® 8.0.
The series included 122 patients with a mean age of 44 ± 16.90 years; with a median of 44 years and range 17-85 years. The distribution by gender showed 73 (60%) male and 49 (40%) female. Forty-nine patients (40%) were admitted by the emergency service and 73 (60%) by the clinic. The mean number of cysts found by US was 1.57 ± 0.91 and the mean number found in surgery was 1.37 ± 0.63. The mean diameter of the main lesion was 10.77 ± 5.62 cm with a median of 10 cm and range 5-30 cm.
When describing the location of the largest cyst, we found that 73 (60%) were located in the right hemi-liver and 49 (40%) in the left hemi-liver. At the time of this study only 49 patients (40%) had undergone CT. Ninety-eight lesions (80%) were hypodense.
The most frequently used surgical technique was subtotal cystectomy in 110 (90%) cases (Table 1). In those patients who underwent a subtotal cystectomy, 90 (82%) also received epiploplasty.
| Technique | n (%) |
| Subtotal cystectomy | 110 (90) |
| Liver resection | 6 (5) |
| Subtotal cystectomy + liver segmentectomy | 2 (2) |
| Others | 4 (3) |
| Total | 122 (100) |
There were evolutionary complications of HH in 20 patients (16%). Intraoperatively, evolutionary complications were found in 49 patients (40%), with the most frequent being cholangiohydatidosis in 38 (31%), followed by HHT in 24 (20%), HAH in 18 (15%) and rupture in 12 (10%).
The surgical area was protected with povidone in 107 patients (88%) and hypertonic solution in 15 (12%). The bile duct was explored via choledochostomy in 39 patients (32%), with the most common indication being suspected cholangiohydatidosis. Cholangiohydatidosis was treated by bile duct exploration and antibiotic treatment. A drain was left in the cystectomy site at the end of the surgery in 81 patients (66%). Twenty-eight per cent of the series (34 patients) presented postoperative complications. The most frequent was atelectasis and pneumonia in 28 patients (23%), surgical site infection in 6 (5%), hemorrhage in 6 (5%). Three patients presented abscess in the residual cavity. Two were solved surgically and 1 patient was treated by CT-guided drainage.
The clinical, evolutionary and laboratory variables according to the presence of complications are described in Table 2.
| Variables | Patients with postoperative complications (n = 25) | Patients without postoperative complications (n = 97) |
| Age (yr) | 48.2 ± 15 | 43.63 ± 17 |
| Sex (% male) | 60 | 33 |
| Evolutionary complications of the cyst (before surgery) (%) (HAH, HHT, rupture to the abdominal cavity and cholangiohydatidosis) | 20 | 9 |
| Protection of the surgical area (% povidone) | 24 | 21 |
| Number of cysts | 1.56 ± 0.9 | 1.32 ± 0.5 |
| Leukocyte count (cells/mm3) | 10 245 ± 3955 | 9095 ± 4605 |
| Total bilirubin (mg/dL) | 2.03 ± 2.4 | 1.43 ± 3.7 |
| Alkaline phosphatase (U/L) | 616 ± 576 | 397 ± 440 |
| AST (U/L) | 85.8 ± 39 | 55.8 ± 91 |
| ALT (U/L) | 83.47 ± 94 | 73 ± 96 |
The mortality of the series was 3 patients (2%). Six patients (5%) received albendazole as a pharmacological therapy subsequent to the surgery, despite our protocol. Twenty-three patients (19%) were operated on for pulmonary hydatidosis at some point in the postoperative evolution, with the most frequent surgery being cystectomy in 111 patients (91%), followed by pulmonary lobectomy (9%).
With an average follow-up of 22.4 ± 8 mo, 13 patients (11%) presented recurrence. In 10 patients recurrence was in relation to a surgical site.
When the biopsies of the patients operated for suspected HH were reviewed, we found that HH was confirmed in 120 patients (98%). In only 3 patients did the biopsy show different results: in 2 patients the biopsy revealed a simple hepatic cyst with signs of inflammation and in 1 patient a primitive neuroectodermic tumor was discovered.
The mean hospital stay was 16.33 ± 8 d with a median of 13 d and range 3-62 d.
All the patients in our series had abdominal pain as the main symptom upon admittance. Our center does not run routine immunological exams for Equinococcus because several previous reports from our center question their diagnostic value[13]. Our diagnostic suspicion is based on epidemiological history, the study of images and the clinical presentation of the patient.
The mean age of the series (44 years) and the predominance of males are remarkable aspects in that these vary from what was recently reported by a Greek series where female gender was higher and patients were younger[14].
The average diameter of the main lesion (10.77 ± 5.62 cm) is less than that reported in a previous cohort conducted in our center (14.5 ± 6 cm). Predominant location in the right hemi-liver tallies with national and international series[11-15].
Among the evolutionary complications of HH, the most frequent was cholangiohydatidosis (31%), followed by hepatothoracic transit (20%). This contrasts with a previous cohort studied in our center, where the most frequent evolutionary complication was HAH (51.5%) followed by cholangiohydatidosis (10.6%)[11].
We have changed the preference of surgical area protection to diluted povidone, due to some cases of hypernatremia which occurred with use of hypertonic saline solution.
With respect to the surgical technique, our team prefers subtotal cystectomy with epiploplasty. We are emphatic about resecting most of the content of the cyst, leaving only the surface in contact with the vascular structures, which we would call an “almost total cystectomy”. To this end, it is necessary to have a complete mobilization of the liver and to be familiar with the vascular structures of the hepatic segments.
Our service does not perform routine choledochostomies in HH surgery. This is demonstrated in the 32% of patients in the series who underwent this procedure, where the majority had suspected cholangiohydatidosis.
Unlike other centers[14], postoperative treatment with albendazole is not routine in our service; this is based on previous studies made in our center that showed a low concentration in the interior of the cyst and the non-existence of an association between the intracystic concentration of albendazole and the viability of the scolices[16].
The recurrence of abdominal hydatidosis (11%) is comparable to a recently published series carried out in Turkey with similar surgical approach[15].
The morbidity (28%) is comparable to that reported by 2 recent international series and 1 cohort conducted in our center[11,12,14] and the mortality (2%) is comparable to that reported recently in a Greek series[14].
A greater prevalence of evolutionary complications and a greater alteration in hepatic test results can be seen in those patients who presented postoperative complications. This tendency must be corroborated in a cohort study designed for this purpose.
The median duration of the hospital stay (16.33 d) is comparable to that published by a previous Chilean series (17 d)[17].
In conclusion, in our Chilean series, subtotal cystectomy was the most common procedure undertaken for HH. The rates of morbidity and mortality are comparable to those reported by other national and international series.
Hepatic hydatidosis (HH) is a zoonosis produced by Equinococcus granulosus that presents a high prevalence and incidence in southern Chile. Based on World Health Organization guidelines and our experience, surgery is one of the most effective treatments for HH.
Patient characteristics and the results of surgical treatment for HH in the Hospital Hernán Henríquez Aravena from December 2001 to March 2005 were described.
The authors are very experienced with the treatment of HH and the number of patients presented would allow for a meaningful analysis, which could help to improve the quality of care for these patients.
The authors describe their surgical technique used in HH treating and compare morbidity and mortality with the available literature.
Peer reviewer: Beat Schnüriger, MD, University of Southern California, Keck School of Medicine, Department of Surgery, Division of Acute Care Surgery (Trauma, Emergency Surgery and Surgical Critical Care), 1200 North State Street, Inpatient Tower (C), 5th Floor, Room C5L100, Los Angeles, CA 90033-4525, United States
S- Editor Tian L L- Editor Logan S E- Editor Lin YP
| 1. | Craig PS, Larrieu E. Control of cystic echinococcosis/hydatidosis: 1863-2002. Adv Parasitol. 2006;61:443-508. |
| 2. | Aliaga F, Oberg C. [Epidemiology of human hydatidosis in the IX Region of la Araucania, Chile 1991-1998]. Bol Chil Parasitol. 2000;55:54-58. |
| 3. | Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ. 1996;74:231-242. |
| 4. | Manterola C, Fernández O, Muñoz S, Vial M, Losada H, Carrasco R, Bello N, Barroso M. Laparoscopic pericystectomy for liver hydatid cysts. Surg Endosc. 2002;16:521-524. |
| 5. | Belchev B, Donev S, Belchev N. [The postoperative results of the surgical treatment of hepatic echinococcosis using a closed surgical method]. Khirurgiia (Sofiia). 1997;50:20-21. |
| 6. | Sabău D, Coman A, Bratu D, Smarandache G, Dumitra A, Sabău A. [Laparoscopic surgery for hepatic hydatid cyst--possibilities and limitations]. Chirurgia (Bucur). 2007;102:543-548. |
| 7. | Daradkeh S, El-Muhtaseb H, Farah G, Sroujieh AS, Abu-Khalaf M. Predictors of morbidity and mortality in the surgical management of hydatid cyst of the liver. Langenbecks Arch Surg. 2007;392:35-39. |
| 8. | Demirci S, Eraslan S, Anadol E, Bozatli L. Comparison of the results of different surgical techniques in the management of hydatid cysts of the liver. World J Surg. 1989;13:88-90; discussion 90-91. |
| 9. | Reza Mousavi S, Khoshnevis J, Kharazm P. Surgical treatment of hydatid cyst of the liver: drainage versus omentoplasty. Ann Hepatol. 2005;4:272-274. |
| 10. | Dziri C, Paquet JC, Hay JM, Fingerhut A, Msika S, Zeitoun G, Sastre B, Khalfallah T. Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver: a multicenter, prospective, randomized trial. French Associations for Surgical Research. J Am Coll Surg. 1999;188:281-289. |
| 11. | Manterola C, Vial M, Pineda V, Sanhueza A, Barroso M. Factors associated with morbidity in liver hydatid surgery. ANZ J Surg. 2005;75:889-892. |
| 12. | Safioleas MC, Misiakos EP, Kouvaraki M, Stamatakos MK, Manti CP, Felekouras ES. Hydatid disease of the liver: a continuing surgical problem. Arch Surg. 2006;141:1101-1108. |
| 13. | Manterola C, Cuadra A, Muñoz S, Sanhueza A, Bustos L, Vial M, Fonseca F. In a diagnostic test study the validity of three serodiagnostic test was compared in patients with liver echinococcosis. J Clin Epidemiol. 2005;58:401-406. |
| 14. | Avgerinos ED, Pavlakis E, Stathoulopoulos A, Manoukas E, Skarpas G, Tsatsoulis P. Clinical presentations and surgical management of liver hydatidosis: our 20 year experience. HPB (Oxford). 2006;8:189-193. |
| 15. | Akbulut S, Senol A, Sezgin A, Cakabay B, Dursun M, Satici O. Radical vs conservative surgery for hydatid liver cysts: experience from single center. World J Gastroenterol. 2010;16:953-959. |
| 16. | Manterola C, Mansilla JA, Fonseca F. Preoperative albendazole and scolices viability in patients with hepatic echinococcosis. World J Surg. 2005;29:750-753. |
| 17. | Lorca HM, Campanella RC, Gavrilovics AB, Lagos LS, Florín CV. Estimation of total and partial costs about diagnosis, surgical treatment and monitoring of hepatic hydatid disease in Hospital San Juan de Dios , Santiago, Chile, 1990-1999. Rev Chil Cir. 2003;55:60-64. |