Published online Jan 14, 2010. doi: 10.3748/wjg.v16.i2.245
Revised: November 23, 2009
Accepted: November 30, 2009
Published online: January 14, 2010
AIM: To compare the cost and accuracy of upper gastrointestinal (GI) X-ray and upper endoscopy for diagnosis of gastric cancer using data from the 2002-2004 Korean National Cancer Screening Program (NCSP).
METHODS: The study population included 1 503 646 participants in the 2002-2004 stomach cancer screening program who underwent upper GI X-ray or endoscopy. The accuracy of screening was defined as the probability of detecting gastric cancer. We calculated the probability by merging data from the NCSP and the Korea Central Cancer Registry. We estimated the direct costs of the medical examination and the tests for upper GI X-ray, upper endoscopy, and biopsy.
RESULTS: The probability of detecting gastric cancer via upper endoscopy was 2.9-fold higher than via upper GI X-ray. The unit costs of screening using upper GI X-ray and upper endoscopy were $32.67 and $34.89, respectively. In 2008, the estimated cost of identifying one case of gastric cancer was $53 094.64 using upper GI X-ray and $16 900.43 using upper endoscopy. The cost to detect one case of gastric cancer was the same for upper GI X-ray and upper endoscopy at a cost ratio of 1:3.7.
CONCLUSION: Upper endoscopy is slightly more costly to perform, but the cost to detect one case of gastric cancer is lower.
- Citation: Lee HY, Park EC, Jun JK, Choi KS, Hahm MI. Comparing upper gastrointestinal X-ray and endoscopy for gastric cancer diagnosis in Korea. World J Gastroenterol 2010; 16(2): 245-250
- URL: https://www.wjgnet.com/1007-9327/full/v16/i2/245.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i2.245
Gastric cancer is the second most common cause of cancer death worldwide, and countries in East Asia, such as China and Japan, have a high incidence of gastric cancer. Korea has 66 cases per 100 000 in men and 34 cases per 100 000 in women. Although the incidence has declined in recent decades, gastric cancer remains the most frequent cancer diagnosis in Korea[1,2]. The prevention and early detection of gastric cancer is therefore a high priority.
Many Asian countries have no national guidelines or recommendations for gastric cancer screening. In high-risk regions such as Japan and Korea, where gastric cancer is highly prevalent, screening is recommended for individuals over 40 years of age. Japan utilizes mass X-ray screening programs to detect gastric cancer in its early stages[1,3]. In recent years, mass screening with upper endoscopy has replaced upper gastrointestinal (GI) X-ray in several cities in Japan, and is considered to be a superior technique by the Japanese medical system[4,5]. Upper endoscopy is a highly effective screening method that detects early gastric cancer at a higher rate than upper GI X-ray. However, there are cost issues associated with upper endoscopic mass screening, in that it is nearly 4-fold more expensive than upper GI X-ray in the Japanese medical system[5,6]. In addition, primary screening endoscopy was proposed as a cost-effective method to screen for gastric cancer in an intermediate-risk population such as in Singapore[7].
Despite this promising result, direct evidence about the effectiveness of upper endoscopy among individuals at average risk of gastric cancer is still not sufficient to justify its use for routine screening, and no nationwide screening program is available[2,8]. Upper endoscopy may be the most cost-effective screening program for Korea, given the relatively low cost of the technique and the high incidence of gastric cancer.
Korea has an organized population-based screening program in which people within a specified age range regularly receive a personal letter inviting them to undergo cancer screening. In 1999, Korea began screening for gastric cancer as a part of the National Cancer Screening Program (NCSP). The target population was enrolled in Medicaid and had National Health Insurance with a premium below 50%. Currently, NCSP provides screening services free of charge. The NCSP recommends biennial upper GI X-ray or upper endoscopic gastric cancer screening for men and women older than 40[9]. Although the NCSP offers either upper GI X-ray or upper endoscopy examination as an initial screening method for gastric cancer, there is a lack of agreement about the recommendation of screening method among the government, physicians, and the general population[2].
Given the limited healthcare resources, policy-makers require estimates of the effectiveness and costs of alternative prevention programs. Ideally, policy decisions should be based on the long-term effectiveness and cost-effectiveness of gastric cancer screening[10]. However, screening for gastric cancer is not commonly practiced, and there is a paucity of data to lend support to such a program. Few data are currently available regarding the long-term effectiveness of alternative gastric cancer screening strategies. The evaluation of the effects of gastric cancer screening on prognosis is incomplete and epidemiologic data on the survival, mortality, and distribution of gastric cancer stage are still insufficient in Korea. In the present study, we examined the short-term cost-effectiveness. The data presented here are preliminary, and we were unable to show that the screening programs examined are associated with a decrease in gastric cancer mortality.
We estimated an intermediate outcome: the cost per case detected[10,11]. The effectiveness of screening was defined as the probability of detecting gastric cancer. We compared other accuracy indicators between upper GI X-ray and upper endoscopy, such as sensitivity and specificity. We calculated accuracy by merging data from the NCSP and the Korea Central Cancer Registry (KCCR), a nationwide hospital-based cancer registration program that covers more than 90% of the cancer cases in Korea[12].
We used data from the NCSP collected from 2002 to 2004. In total, 1 608 810 participated in the stomach cancer screening program. Of the 1 608 810 participants, male and female subjects who were free of gastric cancers and had complete information related to gastric cancer screening results and identification number were included in this study. The data from 1 503 646 participants in the stomach cancer screening program were finally included in this analysis.
The screening results of the NCSP were reported as follows: “normal”, “benign”, “suspicious”, or “cancer”. We defined both “suspicious” and “cancer” as positive results in each screening method. Outcomes of stomach cancer incidence were based on a 1-year follow-up using the KCCR as a gold standard. We defined cancer incidence by the International Classification of Diseases, code C16 (ICD-10:C16). This research was approved by the Institutional Review Board (IRB) committee.
We used 2 models to calculate the total cost of gastric cancer screening. One model included the additional costs for diagnostic follow-up after obtaining abnormal results to consider the costs of upper endoscopy incurred after the upper GI X-ray, which was outside the scope of the NCSP. The costs for diagnostic follow-up were based on the payment system for clinics. The other model included only the direct costs of providing preventive cancer screening services (i.e. only the cost a screening program would incur).
We estimated the screening costs of the medical examination and the tests for upper GI X-ray, upper endoscopy, and biopsy. When the upper GI X-ray identified an abnormal result, the diagnosis had to be confirmed with upper endoscopy and biopsy, even if the final result was a false positive. Therefore, the patient may incur expenses in addition to the initial screening test. We performed 2 cost analyses: in model I (the standard model), we calculated the cost of diagnosis confirmation when the results of the upper GI X-ray were positive (“suspicious” or “cancer”), whereas model II represented the expense to the screening program and only included the cost of the screening test.
The stomach cancer screening costs were based on the 2008 National Cancer screening payment system. Costs were expressed in US dollars (USD), based on the average exchange rate of 1121.88 won for 1 USD in 2008. We varied the cost-ratio of upper GI X-ray and upper endoscopy screening programs, to explore the change in cost-effectiveness when the cost of upper endoscopy was higher than that of upper GI X-ray, as in other countries.
Between January 2002 and December 2004, 1 503 646 people took part in the NCSP (Table 1). Of those, 71% were screened using upper GI X-ray and 29% were screened with upper endoscopy. Of the participants who were screened in 2002, 75.0% of the participants underwent upper GI X-ray and 25.0% underwent upper endoscopy. In 2004, 68.3% underwent upper GI X-ray and 31.7% underwent upper endoscopy.
| Upper GI X-ray | Upper endoscopy | Total (%) | |
| Year | |||
| 2002 | 290 410 (75.0) | 96 637 (25.0) | 387 047 (100.0) |
| 2003 | 393 217 (70.9) | 161 736 (29.1) | 554 953 (100.0) |
| 2004 | 383 751 (68.3) | 177 895 (31.7) | 561 646 (100.0) |
| Total (%) | 1 067 378 (71.0) | 436 268 (29.0) | 1 503 646 (100.0) |
During a 1-year follow-up period, 3884 new gastric cancer cases were reported, and the gastric cancer incidence was 258.3 per 100 000 people. Of the 1 067 378 people screened with the upper GI X-ray, 109 070 positive results were obtained: 892 were true positives and 108 178 were false positives. In contrast, of the 436 268 participants screened with upper endoscopy, 17 146 positive results led to 1041 true positives and 16 105 false positives (Table 2).
| Upper GI X-ray (n) | Upper endoscopy (n) | |||||
| Cancer | No cancer | Total | Cancer | No cancer | Total | |
| Positive | 892 | 108 178 | 109 070 | 1041 | 16 105 | 17 146 |
| Negative | 1227 | 957 081 | 958 308 | 724 | 418 398 | 419 122 |
| Total | 2119 | 1 065 259 | 1 067 378 | 1765 | 434 503 | 436 268 |
The probability of finding a true positive for gastric cancer in 1 503 646 participants was 836 per 100 000 for the upper GI X-ray screening test and 2386 per 100 000 for upper endoscopy (Table 3). Therefore, the probability of detecting gastric cancer with upper endoscopy was about 2.9-fold higher than with upper GI X-ray. The sensitivities of upper GI X-ray and upper endoscopy were 42.1% and 59.0%, respectively, and the specificities were 89.8% and 96.3%, respectively. The positive predictive value was 0.008 for upper GI X-ray and 0.061 for upper endoscopy, and the negative predictive values were 0.999 and 0.998, respectively.
| Model I | Model II | |||
| Upper GI X-ray | Upper endoscopy | Upper GI X-ray | Upper endoscopy | |
| Probability of gastric cancer (n) | 0.000836 | 0.002386 | 0.000836 | 0.002386 |
| Unit cost, US$ (a) | 44.37 | 40.33 | 37.14 | 40.33 |
| Cost to detect one case of gastric cancer (a/n) | 53 094.64 | 16 900.43 | 44 445.78 | 16 900.43 |
| Reduction in cost to detect one case of gastric cancer | 36 194.21 | 27 545.35 | ||
Table 4 shows the unit costs for gastric cancer screening in 2008. Screening using upper GI X-ray and upper endoscopy cost $32.67 and $34.89, respectively, and the cost ratio was 1:1.07.
| Units | Cost in USD | |
| Screening cost | Medical examination | $4.47 |
| Upper gastrointestinal X-ray | $32.67 | |
| Upper endoscopy | $34.89 | |
| Biopsy | $24.54 | |
| Confirmation cost | $70.73 |
The cost of identifying one case of gastric cancer was estimated to be $53 094.64 with upper GI X-ray screening and $16 900.43 with upper endoscopy in 2008. Therefore, using upper endoscopy as the initial screening test would reduce the cost of detecting one case of gastric cancer by $36 194.21 in model I and $27 545.35 in model II.
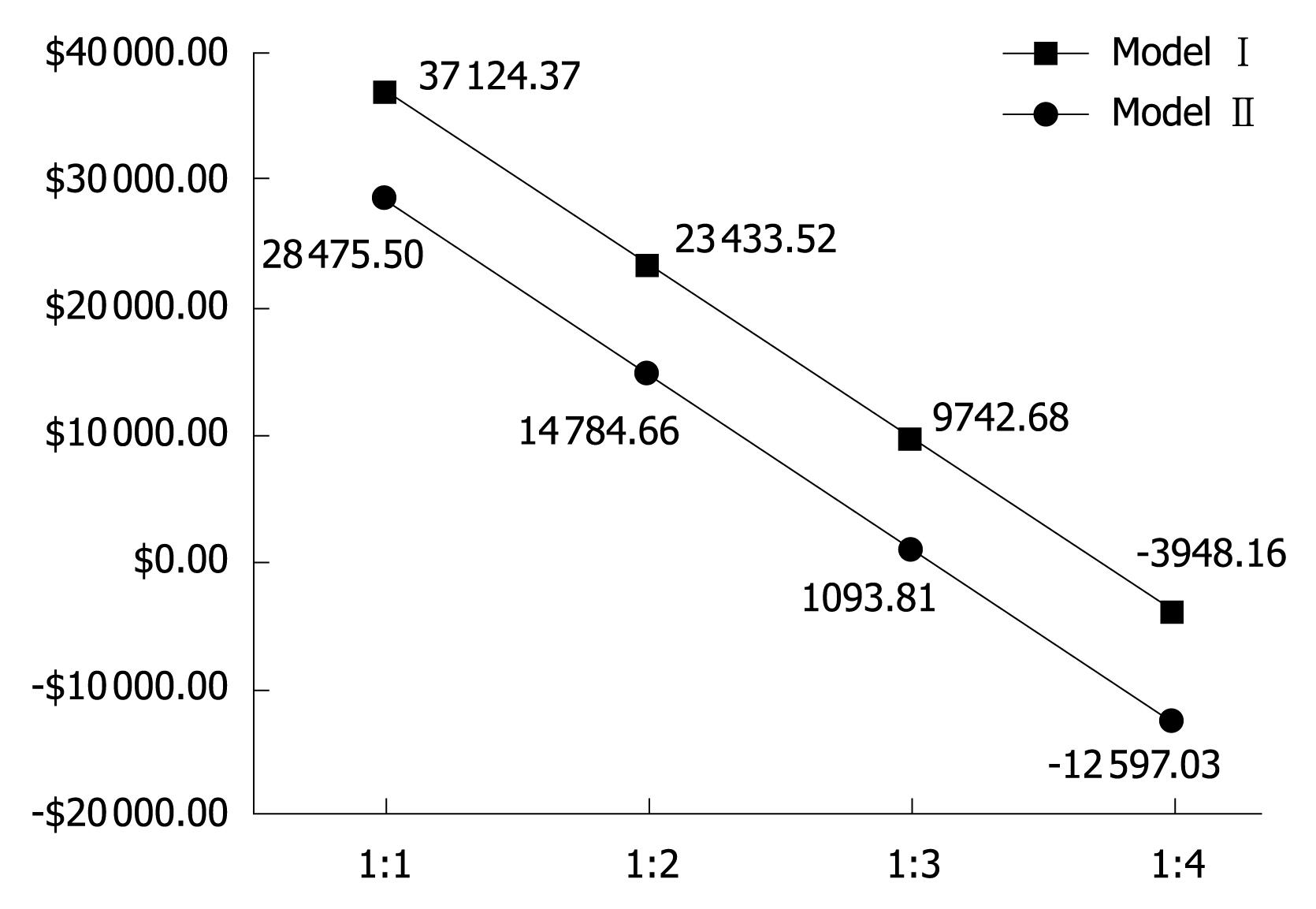
Figure 1 shows the difference in cost-effectiveness according to various cost ratios for the upper GI X-ray and upper endoscopy screening programs. This was analyzed to explore the change in cost-effectiveness when the cost of upper endoscopy exceeded that of upper GI X-ray, as in other countries. At a ratio of 1:1, we can save $37 124.37 in model I. However, when upper endoscopy screening was 4-fold more expensive than upper GI X-ray, it cost $3948.16 more to conduct an upper endoscopy test than an upper GI X-ray. In model I, the cost to detect one case of gastric cancer was the same for upper GI X-ray and upper endoscopy at a cost ratio of 1:3.7.
We found that the upper endoscopy screening test was more accurate and the detection rate was higher than for upper GI X-ray. A few studies have examined the accuracy of upper endoscopy in detecting cancer[1,4,5,13-16]. A study conducted in Niigata, Japan found that the detection rate of gastric cancer when using endoscopy was 2.7-4.6-fold higher than when using upper GI X-ray or photofluorography[1,5]. These investigators reported an endoscopic sensitivity of 77.8% based on a 3-year follow-up using the cancer registry system in Fukui prefecture[14]. Another study based on a follow-up survey of individual participants reported that the sensitivity of endoscopy was 84%[16]. Our findings for sensitivity and specificity were lower than those reported by others for both upper endoscopy and the upper GI X-ray.
It is difficult to directly compare the results of different studies because of differences in target populations and gastric cancer screening systems. For example, our target population was a general population and included people from across the nation. The other studies mentioned here were conducted in municipalities within a prefecture and were hospital-based. Moreover, in Japan photofluorography is the initial assessment for gastric cancer screening followed by upper GI X-ray and upper endoscopy[1,3,4,13,17], whereas in Korea upper GI X-ray or upper endoscopy are the initial tests in organized gastric cancer screening programs.
Despite the diagnostic advantages of upper endoscopy, it is more expensive and requires more staff and technological expertise than upper GI X-ray. In financial terms, the test is not as effective if the cost is high. The cost of upper endoscopy is 3-4-fold more expensive than upper GI X-ray in Japanese gastric cancer screening programs[5,6]. However, Japanese studies showed that even when the ordinary examination fee is charged, upper endoscopy was still the most cost-effective method for detecting gastric cancer[1,5,6]. Nevertheless, it is unlikely that upper endoscopy would be feasible as a mass screening program, even in highly developed countries such as Japan, because of a lack of experienced endoscopists[1,5].
In contrast, there are a number of skilled endoscopists in Korea, making upper endoscopy mass screening more practical. In 2008, there were more than 4000 board-certified endoscopic specialists in Korea who were members of the Korean Society of Gastrointestinal Endoscopy, and their ranks have been increasing by about 150 persons annually. Upper endoscopy mass screening for gastric cancer has a higher detection probability than upper GI X-ray, and upper endoscopy is a more cost-effective screening method in Korea, given the relatively low cost of this technique (about the same as upper GI X-ray) and the high incidence of gastric cancer[1,18]. The results of our study indicate that upper endoscopy will be a more cost-effective mass screening program than upper GI X-ray until the cost per cancer case detected becomes 3.7-fold more expensive than with upper GI X-ray.
The majority of people who undergo cancer screening receive no benefit from the procedure and may actually be exposed to additional health risks as a result of screening. These risks arise from complications that can result in hospitalization or even death, from false positive results that lead to unnecessary, invasive follow-up procedures, and from over diagnosis (i.e. the treatment of cancers that, in the absence of screening, would neither have been detected in the patient’s lifetime nor caused death). Therefore, mass screening is a tradeoff between major benefits to a few and small risks to many[19].
Calculation of the total cost of gastric cancer screening must include the costs of upper endoscopy incurred after the initial assessment, as well as those of complications that infrequently result from the procedure. The balance of cost-effectiveness includes not only financial costs, but also non-financial costs including anxiety, emotional distress, and inconvenience. We didnot include these non-financial costs in our study. Upper endoscopy is an invasive, but relatively safe procedure with an extremely low complication rate (mortality, 1 in 3300-40 000)[7,13,20]. Upper endoscopy enables simultaneous biopsy for histological confirmation of malignancy. Early detection with upper endoscopy permits curative management by surgical resection and endoscopic mucosal resection[4,17]. Upper endoscopy can detect gastric cancer at an earlier stage than upper GI X-ray. However, we were unable to compare the stage distribution of gastric cancer detected by upper endoscopy or upper GI X-ray, because NCSP does not require the reporting of detailed clinical information including the stage of gastric cancer detected by screening.
Another weakness in our study was the inability to control self-selection bias, because we didnot have information about socioeconomic status such as income level, education level, or job status and risk factors. These problems should be resolved in a prospective study that we have planned for the future. In a previous study, respondents with higher income levels were more likely to have an upper endoscopy test. Under the Korean health insurance system, the cost of the upper endoscopy test is almost the same as that for the upper GI X-ray. In addition, the NCSP offers a free-of-charge endoscopy test for gastric cancer screening. Despite these programs, disparities in the use of endoscopy vary with household income, possibly suggesting that misconceptions exist about the cost of endoscopy. In addition, the higher rates of endoscopy use in those with a family history of gastric cancer might indicate that the endoscopy test was the preferred test for a high-risk population[2].
Screening large numbers of people is a costly undertaking. Healthcare providers and policy-makers are increasingly interested in the efficient allocation of medical resources, including those used for cancer screening programs. It is essential to have a framework that compares the health benefits and resource expenditures associated with competing medical and public health interventions that will allow decision-makers to identify cost-effective interventions. A complete cost-effectiveness analysis of alternative screening strategies depends on the treatment cost and its effect in terms of life years saved (or quality-adjusted life years saved)[10,19]. Longer follow-up is required to generate the mortality results critical for decision-making. However, decisions about whether and how to screen for cancer cannot always be delayed until mortality data are available. Some degree of modeling is frequently required to translate intermediate trial outcomes to long-term outcomes, making cost-effectiveness analysis necessary[19].
The data presented here are preliminary, and we were unable to show that the screening programs examined were associated with a decrease in gastric cancer mortality. Follow-up studies are needed to further investigate this. However, the intermediate outcomes used here indicate that, in Korea, upper endoscopy is a more cost-effective screening program than upper GI X-ray. Although the incidence and mortality of gastric cancer has decreased in Korea during the last decade, gastric cancer screening continues to be a major issue because incidence and mortality remain high.
The best test is a matter of personal preference, which should be considered when physicians make recommendations for screening. Upper endoscopy is gaining acceptance as a standard method for gastric cancer screening and the preferred gastric cancer screening method according to a population-based survey[2,21]. The providers’ assessment of individuals’ screening preferences, in combination with intervention strategies to promote performance of the preferred screening method, may increase compliance with gastric cancer screening recommendations[22,23]. It will be imperative to consider these results when making decisions about population-based screening strategies[24]. Evidence-based screening should be promoted in the future to prevent premature death from gastric cancer. To achieve this goal, it is necessary to determine the effectiveness of upper GI X-ray and upper endoscopy mass screening in reducing mortality.
In high-risk regions such as Japan and Korea, where gastric cancer is highly prevalent, screening is recommended for individuals over 40 years of age. However, many Asian countries have no national guidelines or recommendations for gastric cancer screening.
In recent years, mass screening with upper endoscopy has replaced upper gastrointestinal (GI) X-ray in several cities in Japan, and is considered to be a superior technique by the Japanese medical system. However, there are cost issues associated with upper endoscopic mass screening. In addition, primary screening endoscopy was proposed as a cost-effective method to screen for gastric cancer in an intermediate-risk population such as in Singapore. Despite this promising result, direct evidence about the effectiveness of upper endoscopy among individuals at average risk of gastric cancer is still not sufficient to justify its use for routine screening, and no nationwide screening program is available.
The authors identified that upper endoscopy slightly more costly to perform, but the cost to detect one case of gastric cancer was lower. Their study showed the usefulness of endoscopy as an organized screening technique across the nation.
Upper endoscopy mass screening is a more cost-effective screening method than upper GI X-ray in Korea, and with its relatively low cost, the high incidence of gastric cancer, and the number of skilled endoscopists, upper endoscopy mass screening is more practical for gastric cancer screening.
The work is an interesting study to be accepted for publication.
Peer reviewer: Luis Bujanda, Professor, Departament of Gastroenterology, CIBEREHD, University of Country Basque, Donostia Hospital, Paseo Dr. Beguiristain s/n, 20014 San Sebastián, Spain
S- Editor Tian L L- Editor Cant MR E- Editor Ma WH
| 1. | Leung WK, Wu MS, Kakugawa Y, Kim JJ, Yeoh KG, Goh KL, Wu KC, Wu DC, Sollano J, Kachintorn U. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol. 2008;9:279-287. |
| 2. | Choi KS, Kwak MS, Lee HY, Jun JK, Hahm MI, Park EC. Screening for gastric cancer in Korea: population-based preferences for endoscopy versus upper gastrointestinal series. Cancer Epidemiol Biomarkers Prev. 2009;18:1390-1398. |
| 3. | Mizoue T, Yoshimura T, Tokui N, Hoshiyama Y, Yatsuya H, Sakata K, Kondo T, Kikuchi S, Toyoshima H, Hayakawa N. Prospective study of screening for stomach cancer in Japan. Int J Cancer. 2003;106:103-107. |
| 4. | Suzuki H, Gotoda T, Sasako M, Saito D. Detection of early gastric cancer: misunderstanding the role of mass screening. Gastric Cancer. 2006;9:315-319. |
| 5. | Tashiro A, Sano M, Kinameri K, Fujita K, Takeuchi Y. Comparing mass screening techniques for gastric cancer in Japan. World J Gastroenterol. 2006;12:4873-4874. |
| 6. | Matsumoto S, Yamasaki K, Tsuji K, Shirahama S. Results of mass endoscopic examination for gastric cancer in Kamigoto Hospital, Nagasaki Prefecture. World J Gastroenterol. 2007;13:4316-4320. |
| 7. | Dan YY, So JB, Yeoh KG. Endoscopic screening for gastric cancer. Clin Gastroenterol Hepatol. 2006;4:709-716. |
| 8. | Hosokawa O, Miyanaga T, Kaizaki Y, Hattori M, Dohden K, Ohta K, Itou Y, Aoyagi H. Decreased death from gastric cancer by endoscopic screening: association with a population-based cancer registry. Scand J Gastroenterol. 2008;43:1112-1115. |
| 9. | Ministry for Health, Welfare and Family Affairs, National Cancer Center. Cancer facts & figures 2008 in Korea, 2008. |
| 10. | Legood R, Gray AM, Mahé C, Wolstenholme J, Jayant K, Nene BM, Shastri SS, Malvi SG, Muwonge R, Budukh AM. Screening for cervical cancer in India: How much will it cost? A trial based analysis of the cost per case detected. Int J Cancer. 2005;117:981-987. |
| 11. | Ekwueme DU, Gardner JG, Subramanian S, Tangka FK, Bapat B, Richardson LC. Cost analysis of the National Breast and Cervical Cancer Early Detection Program: selected states, 2003 to 2004. Cancer. 2008;112:626-635. |
| 12. | Ministry for Health, Welfare and Family Affairs. Annual Report of cancer incidence (2005) and survival (1993-2005) in Korea, 2008. |
| 13. | Hamashima C, Shibuya D, Yamazaki H, Inoue K, Fukao A, Saito H, Sobue T. The Japanese guidelines for gastric cancer screening. Jpn J Clin Oncol. 2008;38:259-267. |
| 14. | Hosokawa O, Hattori M, Takeda T, Watanabe K, Fujita M. Accuracy of endoscopy in detecting gastric cancer. Jpn J Gastroenterol Mass Survey. 2004;42:33-39. |
| 15. | Hosokawa O, Tsuda S, Kidani E, Watanabe K, Tanigawa Y, Shirasaki S, Hayashi H, Hinoshita T. Diagnosis of gastric cancer up to three years after negative upper gastrointestinal endoscopy. Endoscopy. 1998;30:669-674. |
| 16. | Otsuji M, Kouno Y, Otsuji A, Tokushige J, Shimotatara K, Arimura K. Assessment of small diameter panendoscopy for diagnosis of gastric cancer: comparative study with follow-up survey date. Stomach and Intestine. 1989;24:1291-1297. |
| 17. | Kunisaki C, Ishino J, Nakajima S, Motohashi H, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, Shimada H. Outcomes of mass screening for gastric carcinoma. Ann Surg Oncol. 2006;13:221-228. |
| 18. | Choi IJ. [Gastric cancer screening and diagnosis]. Korean J Gastroenterol. 2009;54:67-76. |
| 19. | Knudsen AB, McMahon PM, Gazelle GS. Use of modeling to evaluate the cost-effectiveness of cancer screening programs. J Clin Oncol. 2007;25:203-208. |
| 21. | National Cancer Center. Annual report of national cancer screening program in Korea, 2008. |
| 22. | Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15:389-394. |
| 23. | Leard LE, Savides TJ, Ganiats TG. Patient preferences for colorectal cancer screening. J Fam Pract. 1997;45:211-218. |
| 24. | Lee YC, Lin JT, Wu HM, Liu TY, Yen MF, Chiu HM, Wang HP, Wu MS, Hsiu-Hsi Chen T. Cost-effectiveness analysis between primary and secondary preventive strategies for gastric cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:875-885. |