Published online Oct 14, 2009. doi: 10.3748/wjg.15.4853
Revised: September 8, 2009
Accepted: September 15, 2009
Published online: October 14, 2009
Peptic ulcer disease is uncommon in children and rarely suspected as a cause of abdominal complaints in this age group; the diagnosis is therefore made almost exclusively when complications develop. Peptic ulcer disease is usually not considered in the differential diagnosis of pediatric patients. We present the case of a 30-month-old boy with duodenal perforation due to a peptic ulcer without a known etiology. The patient was admitted through the emergency department due to severe hematochezia and ongoing anemia; he presented with neither abdominal pain nor abdominal distension. There were no medical problems, and no drugs, such as corticosteroids or nonsteroidal anti-inflammatory drugs, had been prescribed or administered recently. We tried to control the active bleeding by medical treatment including arterial embolization, but the active bleeding was not controlled. Finally, an exploratory laparotomy was performed. A discrete anterior perforation with active bleeding of the duodenal wall was found. After the operation, there were no complications and the patient recovered fully.
- Citation: Lee NM, Yun SW, Chae SA, Yoo BH, Cha SJ, Kwak BK. Perforated duodenal ulcer presenting with massive hematochezia in a 30-month-old child. World J Gastroenterol 2009; 15(38): 4853-4855
- URL: https://www.wjgnet.com/1007-9327/full/v15/i38/4853.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4853
Upper gastrointestinal (GI) bleeding in children accounts for approximately 10% of all GI bleeding in children[1,2]. Gastric and duodenal ulcers are infrequent causes of GI bleeding in children[3-5]. The majority of children with active gastritis and ulcers of the stomach or duodenum have an associated systemic condition, such as overwhelming sepsis, severe head or body trauma, or burns[6]. A history of taking medications such as corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) is also important. However, in the absence of such significant history, symptoms of childhood peptic ulcer disease can easily be overlooked in the initial stages, which can result in catastrophic consequences such as perforation or hemorrhage[3,7].
We report here on a 30-month-old boy with duodenal perforation due to an ulcer. The patient presented to the emergency department (ED) with massive hematochezia (gastrointestinal bleeding) and ongoing active bleeding, and was subsequently found to have a perforated duodenal ulcer. This patient had an atypical presentation in that there were no antecedent signs or symptoms of peptic ulcer disease before the perforation.
A 30-month-old boy visited the ED with acute massive hematochezia. Two days before, he had watery diarrhea twice per day for 2 d, and was successfully managed with fluid therapy without any other medications at the ED. The patient was doing well before the incident except for a mild decrease in appetite. On arrival to the ED, he was alert, but he looked acutely ill. The patient presented with only hematochezia without abdominal pain or abdominal distension.
The medical history revealed that he was delivered vaginally at term, and otherwise had no significant prenatal or postnatal complications. There were no previous hospitalizations or medical problems, his immunization status was up-to-date, and no drugs had been prescribed or administered recently (especially NSAIDs).
On admission, the body weight was recorded to be 11.0 kg (25-50th percentile), height was 84 cm (3-10th percentile), and head circumference was 53.5 cm (25-50th percentile). His vital signs were as follows: blood pressure 110/60 mmHg; pulse rate 80 beats/minute (bpm); respiration rate 20 breaths/min; temperature 36.6°C.
The patient looked acutely ill and had pale conjunctiva. Chest examination revealed regular heart beats without murmurs and clear breath sounds. Bowel sounds were hyperactive without localized tenderness or rebound tenderness. The abdomen was flat and soft without palpable mass.
The hemoglobin (Hb) was 11.9 g/dL two days ago, but dropped to 7.9 g/dL when checked on ED arrival. However, after 2 h, it dropped further to 7.3 g/dL. Therefore, an ongoing loss of blood was suspected and a transfusion started. Despite massive transfusions, Hb continued to decrease and fell to 4.8 g/dL, and platelets were also reduced to 75 000/mm3 after 2 h. Blood pressure could not be measured and heart rate was more than 160 bpm. A femoral central line catheter was inserted to transfuse packed red blood cells (P-RBC) and platelets. Even with ongoing transfusions, vital signs remained unstable and hematochezia was not improving.
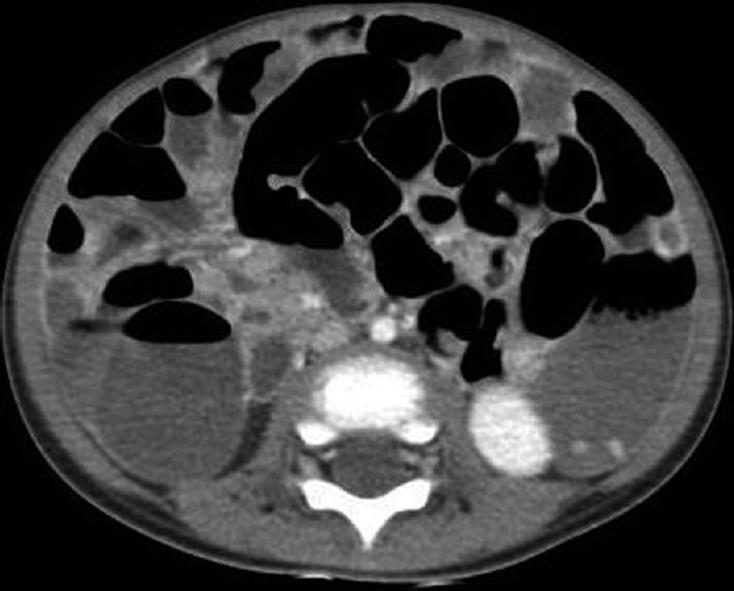
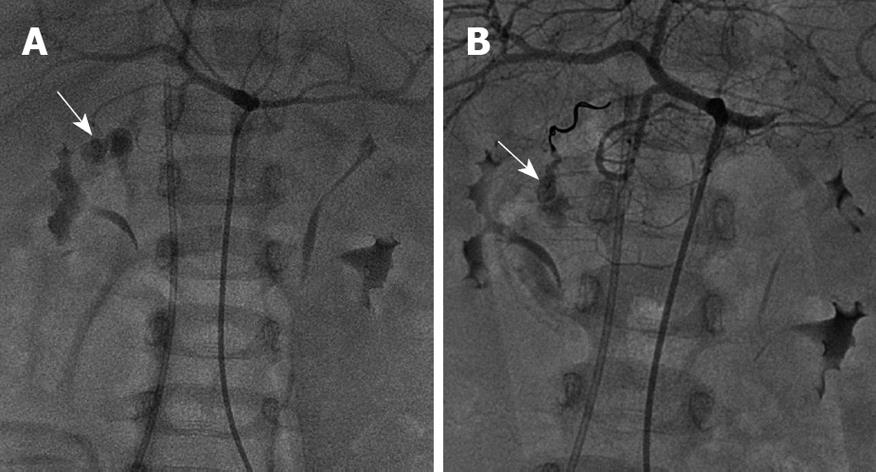
Emergency abdominal CT was performed, which revealed an air-fluid level with distension of the small bowel and colon; in addition, the diameter of the abdominal aorta was decreased. Based on the CT scan, acute blood loss was strongly suspected (Figure 1). To determine the bleeding focus, angiography was performed, which showed extravasation at the duodenal branch of the gastroduodenal artery. Embolization was attempted with 3 coils; however, this could not stop the continuous arterial bleeding (Figure 2). The patient was transfused with 19 pints of P-RBC, 16 pints of platelets and 7 pints of fresh frozen plasma (FFP) because his vital signs were unstable before the operation started.
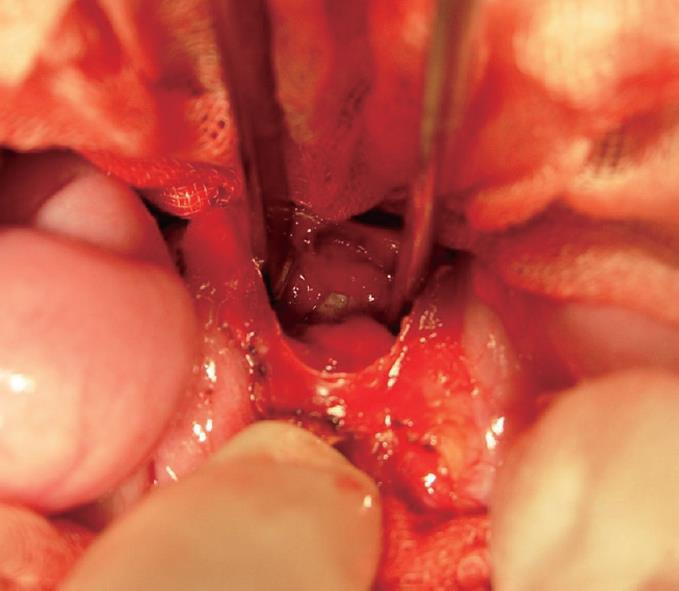
On hospital day #2, an exploratory laparotomy was performed 20 h after arrival at the ED. On entering the peritoneum, a large amount of blood-stained fluid was encountered. A discrete anterior perforation of the duodenal wall was found; there was a perforation injury that was half the size of the whole duodenal diameter at the anterior wall of the second portion of the duodenum. Serosal ulceration and active arterial bleeding were also seen at the gall bladder neck which was in contact with the perforation site. It showed an ulcer base of about 1.5 cm and bleeding in the posterior wall of the perforation site (Figure 3).
After the operation, the vital signs were stable. Hb was maintained in the normal range. We confirmed that the Helicobacter pylori (H pylori) IgM was negative. The patient fully recovered and was eventually discharged without any sequelae.
Peptic ulcer disease is uncommon in children and rarely suspected as a cause of abdominal complaints in this age group[2,4,8]. The diagnosis is therefore made almost exclusively when children develop complications; peptic ulcer disease is rarely included in the differential diagnosis of pediatric patients[2,6,9,10]. Peptic ulcer disease is classified as either gastric or duodenal, based on the location, and either primary (intrinsic) or secondary (extrinsic), depending on the etiology. Ulcer disease in children less than 10 years of age is usually secondary and is located predominantly in the duodenum. However, if a primary ulcer is present in this age group, it is usually gastric in origin. In children 10 years or older, primary ulcer disease is more common[3,4,11,12].
The vast majority of primary duodenal ulcers are associated with H pylori infection of the gastric antral mucosa[7,12-16]. Wong et al [17] reported that patients with perforation underwent laparoscopic patch or open repair. All patients had a course of proton pump inhibitors postoperatively and in 90% of the patients H pylori was identified. In Hong Kong[2], acute upper gastrointestinal bleeding in children was dominated by duodenal ulcers in 75% of the patients and H pylori infection was identified in 55% of the patients.
Secondary ulcer disease occurs as a result of some external predisposing cause, such as medications or stress. Associated medications include aspirin, NSAIDs, and steroids. In infants, stress-induced ulcers are often caused by traumatic delivery, respiratory or cardiac distress, sepsis, hypoglycemia, or dehydration. In older children, life-threatening illness and trauma are the main causes; ulcers associated with intracranial pathology (Cushing’s ulcer) or burns (Curling’s ulcer) have been well described. Since secondary ulcer disease predominantly occurs in the duodenum, it is more likely to present catastrophically, with hemorrhage or perforation as the initial features[5,11,12]. In one study, 30% of patients had perforation on initial presentation[8]. Often, exploratory laparotomy is the only way to diagnose patients with secondary ulcer disease because of the presentation of patients with an acute abdomen.
Moon et al[3] reported the case of a 3-year-old boy presenting with shock who was diagnosed as having a perforated duodenal ulcer. Wilson et al[4] reported the case of a 7-year-old boy who was admitted with gastroenteritis that was complicated by an acute perforated duodenal ulcer. In addition, Sisil Kumara et al[6] reported on a 3-year-old boy who had taken prednisolone for a skin eruption and was diagnosed with a perforated duodenal ulcer. In all three of the above cases, chest radiographs showed air under the diaphragm. However, in our case, the gallbladder shielded the perforation site, and we did not see signs of a perforation. Barandica et al[9] reported that CT was associated with a 26% false-negative rate in the detection of hollow viscus injuries in children.
Chan et al[18] reported that 32 children with endoscopically proven ulcers of the duodenum were evaluated for their long-term outcome after H2-receptor antagonist (H2RA) treatment. In that study, 12.5% of the patients presented with a perforation. All four patients that had perforations were initially treated with a patch repair; two had persistent ulceration despite H2RA treatment and required a proximal gastric vagotomy.
In summary, our patient did not have any of the known causes to explain the development of secondary ulcer disease such as medications and stress, and H pylori infection was not detected in the duodenum. The patient did not exhibit symptoms of a bowel perforation such as abdominal tenderness or rebound tenderness; he presented with lower gastrointestinal bleeding symptoms including massive hematochezia rather than hematemesis or melena. The upright abdominal radiographs did not show free air under the diaphragm. Because the gallbladder wall covered the site of the duodenal perforation, the symptoms associated with bowel perforation were not apparent.
Peer reviewers: Frank I Tovey, OBE, ChM, FRCS, Honorary Research Fellow, Department of Surgery, University College London, London, United Kingdom; Dr. Philip Abraham, Professor, Consultant Gastroenterologist & Hepatologist, P. D. Hinduja National Hospital & Medical Research Centre, Veer Savarkar Marg, Mahim, Mumbai 400 016, India
S- Editor Tian L L- Editor O'Neill M E- Editor Lin YP
| 1. | Stevenson RJ. Gastrointestinal bleeding in children. Surg Clin North Am. 1985;65:1455-1480. |
| 2. | Ameh EA. Duodenal ulcer in childhood in developing countries. Indian Pediatr. 2003;40:272. |
| 3. | Moon D, Weeks D, Burgess B, O'Connor R. Perforated duodenal ulcer presenting with shock in a child. Am J Emerg Med. 1997;15:167-169. |
| 4. | Wilson JM, Darby CR. Perforated duodenal ulcer: an unusual complication of gastroenteritis. Arch Dis Child. 1990;65:990-991. |
| 5. | Flynn DM, Booth IW. Investigation and management of gastrointestinal bleeding in children. Current Paediatrics. 2004;14:576-585. |
| 6. | Sisil Kumara PD, Weerawardena WA, Esufali ST. A perforated duodenal ulcer in a child. Ceylon Med J. 2000;45:133-134. |
| 7. | Edwards MJ, Kollenberg SJ, Brandt ML, Wesson DE, Nuchtern JG, Minifee PK, Cass DL. Surgery for peptic ulcer disease in children in the post-histamine2-blocker era. J Pediatr Surg. 2005;40:850-854. |
| 8. | Cruze K, Snyder WH Jr. Acute perforation of the alimentary tract in infancy and childhood. Ann Surg. 1961;154:93-99. |
| 9. | Barandica R, Patel M. Pediatric duodenal perforation missed on computed tomography. Ann Emerg Med. 1997;30:545-547. |
| 10. | Grosfeld JL, Molinari F, Chaet M, Engum SA, West KW, Rescorla FJ, Scherer LR 3rd. Gastrointestinal perforation and peritonitis in infants and children: experience with 179 cases over ten years. Surgery. 1996;120:650-655; discussion 655-656. |
| 11. | Dohil R, Hassall E. Peptic ulcer disease in children. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:53-73. |
| 12. | Quinn S, Rowland M, Drumm B. Peptic ulcer disease in children. Current Paediatrics. 2003;13:107-113. |
| 13. | Boyanova L, Koumanova R, Lazarova E, Jelev C. Helicobacter pylori and Helicobacter heilmannii in children. A Bulgarian study. Diagn Microbiol Infect Dis. 2003;46:249-252. |
| 14. | Demir H, Gürakan F, Ozen H, Saltik IN, Yüce A, Ozçay F, Koçak N. Peptic ulcer disease in children without Helicobacter pylori infection. Helicobacter. 2002;7:111. |
| 15. | Torres J, Pérez-Pérez G, Goodman KJ, Atherton JC, Gold BD, Harris PR, la Garza AM, Guarner J, Muñoz O. A comprehensive review of the natural history of Helicobacter pylori infection in children. Arch Med Res. 2000;31:431-469. |
| 16. | Drumm B. Helicobacter pylori in the pediatric patient. Gastroenterol Clin North Am. 1993;22:169-182. |
| 17. | Wong BP, Chao NS, Leung MW, Chung KW, Kwok WK, Liu KK. Complications of peptic ulcer disease in children and adolescents: minimally invasive treatments offer feasible surgical options. J Pediatr Surg. 2006;41:2073-2075. |
| 18. | Chan KL, Tam PK, Saing H. Long-term follow-up of childhood duodenal ulcers. J Pediatr Surg. 1997;32:1609-1611. |