Published online Oct 14, 2009. doi: 10.3748/wjg.15.4806
Revised: August 6, 2009
Accepted: August 13, 2009
Published online: October 14, 2009
AIM: To evaluate the clinicopathologic characteristics of patients with metastases to the gallbladder (MGBs).
METHODS: We performed a single-center retrospective study of 20 patients with MGBs diagnosed pathologically from 1999 to 2007.
RESULTS: Among 417 gallbladder (GB) malignancies, 20 (4.8%) were MGBs. The primary malignancies originated from the stomach (n = 8), colorectum (n = 3), liver (n = 2), kidney (n = 2), skin (n = 2), extrahepatic bile duct (n = 1), uterine cervix (n = 1), and appendix (n = 1). Twelve patients were diagnosed metachronously, presenting with cholecystitis (n = 4), abdominal pain (n = 2), jaundice (n = 1), weight loss (n = 1), and serum CA 19-9 elevation (n = 1); five patients were asymptomatic. The median survival after the diagnosis of MGB was 8.7 mo. On Cox regression analysis, R0 resection was the only factor associated with a prolonged survival [hazard ratio (HR): 0.01, P = 0.002]; presentation with cholecystitis was associated with poor survival (HR: 463.27, P = 0.006).
CONCLUSION: MGBs accounted for 4.8% of all pathologically diagnosed GB malignancies. The most common origin was the stomach. The median survival of MGB was 8.7 mo.
- Citation: Yoon WJ, Yoon YB, Kim YJ, Ryu JK, Kim YT. Metastasis to the gallbladder: A single-center experience of 20 cases in South Korea. World J Gastroenterol 2009; 15(38): 4806-4809
- URL: https://www.wjgnet.com/1007-9327/full/v15/i38/4806.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4806
| Site of origin | Pathology |
| Stomach (n = 8) | Adenocarcinoma (n = 7) |
| Signet ring cell carcinoma (n = 1) | |
| Colorectum (n = 3) | Adenocarcinoma (n = 3) |
| Liver (n = 2) | Hepatocellular carcinoma (n = 2) |
| Kidney (n = 2) | Renal cell carcinoma (n = 2) |
| Skin (n = 2) | Melanoma (n = 2) |
| Extrahepatic bile duct (n = 1) | Adenocarcinoma (n = 1) |
| Uterine cervix (n = 1) | Squamous cell carcinoma (n = 1) |
| Appendix (n = 1) | Mucinous adenocarcinoma (n = 1) |
| Synchronously diagnosed | Metachronously diagnosed |
| Anterior resection and liver tumorectomy | Distal pancreatectomy (for pancreatic metastasis) |
| Low anterior resection and liver tumorectomy | Right hemicolectomy |
| Total colectomy and liver tumorectomy | Debulking surgery |
| Palliative common bile duct resection | |
| Palliative gastrojejunostomy | |
| Palliative total gastrectomy | |
| Palliative left lobectomy of the liver | |
| Palliative subtotal gastrectomy and palliative right hemicolectomy |
| Factor | Median survival1 | P value |
| Sex | 0.794 | |
| Male (n = 14) | 11.2 | |
| Female (n = 6) | 6.2 | |
| Primary origin | 0.224 | |
| Gastrointestinal organs (n = 15) | 8.2 | |
| Non-gastrointestinal organs (n = 5) | 35.0 | |
| Chronological relationship between primary malignancy and MGB | 0.913 | |
| Synchronous (n = 8) | 11.2 | |
| Metachronous (n = 12) | 6.9 | |
| Asymptomatic upon diagnosis of MGB | 0.023 | |
| Yes (n = 5) | 40.0 | |
| No (n = 15) | 6.9 | |
| Presentation with acute cholecystitis | < 0.001 | |
| Yes (n = 4) | 2.8 | |
| No (n = 16) | 15.6 | |
| Preoperative diagnosis of MGB | 0.007 | |
| Yes (n = 9) | 35.0 | |
| No (n = 11) | 4.7 | |
| Age at diagnosis of the MGB (yr) | 0.009 | |
| ≥ 70 (n = 5) | 6.2 | |
| < 70 (n = 15) | 21.2 | |
| Secondary involvement of organs other than the GB | 0.586 | |
| Yes (n = 11) | 15.6 | |
| No (n = 9) | 8.7 | |
| Recurrence at the remaining primary site | 0.252 | |
| Yes (n = 1) | 4.7 | |
| No (n = 19) | 11.2 | |
| R0 resection | < 0.001 | |
| Yes (n = 9) | 40.0 | |
| No (n = 11) | 6.2 |
| Factor | HR | 95% CI | P value |
| Male sex | 5.78 | 0.84-39.87 | 0.075 |
| Asymptomatic upon diagnosis of the MGB | 0.79 | 0.15-4.18 | 0.781 |
| Presentation with acute cholecystitis | 36.12 | 2.82-463.27 | 0.006 |
| Preoperative diagnosis of MGB | 0.58 | 0.13-2.62 | 0.477 |
| Age at diagnosis of the MGB ≥ 70 yr | 3.69 | 0.42-32.38 | 0.239 |
| R0 resection | 0.01 | 0.001-0.20 | 0.002 |
Metastases to the gallbladder (MGBs) are rare in clinical practice[1]. Although malignant melanoma[2] and renal cell carcinoma[3] are reported to metastasize to the gallbladder (GB), these data are based on autopsy series of these tumors. Reports on MGBs arising from malignancies other than malignant melanoma and renal cell carcinoma are usually in the form of single case reports[4,5]. There are few, if any, reports that describe MGBs from the perspective of the GB to this date.
This paper describes the clinicopathologic features of 20 patients with MGBs diagnosed over a period of 9 years at a single tertiary hospital.
We reviewed the pathology reports of all GB malignancies diagnosed with pathological confirmation from January 1999 to December 2007 at Seoul National University Hospital. We evaluated the clinicopathologic characteristics of the patients with MGBs. Patients were excluded when direct invasion of the GB from the primary malignancy was confirmed on imaging or intraoperatively.
By reviewing the medical records, sex, the primary origin of the MGB, age at diagnosis of the primary malignancy, age at diagnosis of the MGB, presenting symptoms and signs at diagnosis of the MGB, time interval between the diagnoses of the primary malignancy and the MGB, involvement of organs other than the GB, diagnosis of secondary involvement of the GB before surgery, treatment after the diagnosis of the MGB, and survival after the diagnosis of the MGB were evaluated. Overall follow-up survival information was obtained by contacting the Resident Service Division of the Ministry of Public Administration and Security, Seoul, Korea, and by reviewing medical records. The endpoints of this study were patient death or June 30, 2008.
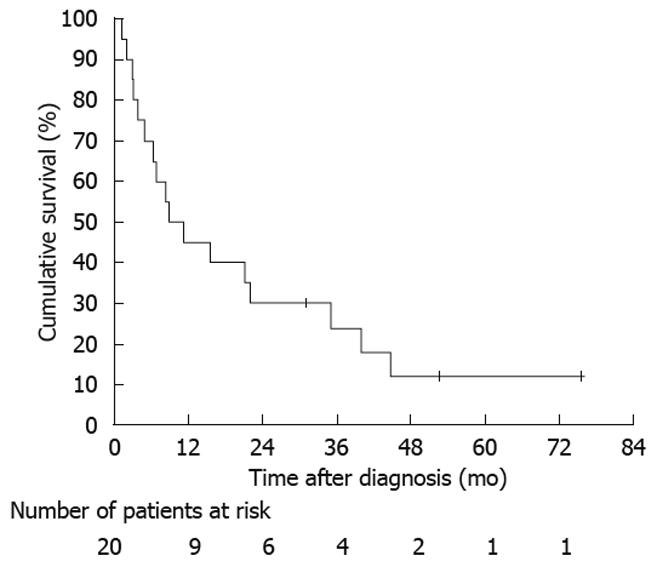
The median survival was estimated using the Kaplan-Meier method. Factors associated with prolonged survival were determined using the log-rank test. The factors including age at diagnosis of the MGB, sex, and factors associated with survival in the univariate analysis at P < 0.20 were included as covariates in the Cox regression analysis. Values are reported as the median. Two-sided P values of < 0.05 were considered statistically significant. All analyses were performed using SPSS for Windows Ver. 11.0 (SPSS Inc., Chicago, Ill., USA). This study was approved by the institutional review board at our hospital.
A total of 417 cases of GB malignancies were diagnosed with pathological confirmation. Among these, 20 cases (14 male and six female) were MGBs, accounting for 4.8% of the GB malignancies.
The median age at diagnosis of MGB was 65 years (range, 28-76 years). The median age at diagnosis of the primary malignancy was 62.5 years (range, 27-76 years). The primary malignancies originated from the stomach (n = 8), colorectum (n = 3), liver (n = 2), kidney (n = 2), skin (n = 2), extrahepatic bile duct (n = 1), uterine cervix (n = 1), and appendix (n = 1) (Table 1). Cancer involvement of organs other than the GB was present in 11 patients.
Eight MGBs were diagnosed synchronously. The primary origins were the stomach (n = 3), colorectum (n = 3), extrahepatic bile duct (n = 1), and liver (n = 1). Twelve MGBs were diagnosed metachronously with a median interval of 24.9 mo (range, 5-191 mo). The primary origin in these patients were the stomach (n = 5), kidney (n = 2), skin (n = 2), liver (n = 1), uterine cervix (n = 1), and appendix (n = 1). Metachronously diagnosed patients presented with cholecystitis (n = 4), abdominal pain (n = 2), jaundice (n = 1), weight loss (n = 1), and elevation of serum CA 19-9 (n = 1); five patients were asymptomatic and the MGBs were detected during follow-up of the primary malignancy. In the four patients that presented with cholecystitis, only one patient had gallstones. Recurrence of the primary malignancy in the remaining primary origin was detected in one patient.
Treatment consisted of surgery (n = 9), surgery plus chemotherapy (n = 8), surgery plus chemoradiation (n = 2), and surgery plus transarterial chemoembolization (n = 1). All synchronously diagnosed patients underwent concurrent surgical procedures; three of 12 metachronously diagnosed patients underwent concurrent surgical procedures (Table 2). The preoperative radiological diagnosis of MGB was made in 9 (45%) patients. Complete surgical resection of all tumors present, i.e. R0 resection, was achieved in nine patients. There was a tendency to achieve R0 resection in patients with preoperative diagnosis of MGBs (66.7% in patients with preoperative diagnosis vs 27.3% in patients without preoperative diagnosis, P = 0.078).
The overall median survival after the diagnosis of MGB was 8.7 mo (Figure 1). On univariate analysis, R0 resection (P < 0.001), asymptomatic on diagnosis of MGB (P = 0.023), and preoperative diagnosis of MGB (P = 0.007) were associated with a prolonged survival; presentation with acute cholecystitis (P < 0.001) and age at diagnosis of MGB ≥ 70 years (P = 0.009) were associated with a poor survival (Table 3). On multivariate analysis, the only factor associated with prolonged survival was R0 resection [hazard ratio (HR): 0.01, 95% confidence interval (CI): 0.001-0.20, P = 0.002]; presentation with acute cholecystitis was associated with poor survival (HR: 36.12, 95% CI: 2.82-463.27, P = 0.006) (Table 4).
The present retrospective analysis of 9 years’ experience at a single tertiary hospital contributes to our understanding of the clinicopathologic features of MGBs. MGBs accounted for 4.8% of all GB malignancies. The most common primary origin was the stomach. Twelve cases (60%) of MGBs were diagnosed metachronously with a median interval of 24.9 mo. The median survival after the diagnosis of MGB was 8.7 mo. On multivariate analysis, R0 resection was the only factor associated with prolonged survival; presentation with acute cholecystitis was associated with poor survival.
Malignant melanoma and renal cell carcinoma are reported to metastasize to the GB. In an autopsy series of 125 patients with malignant melanoma, nineteen (15%) had MGBs[2]. In an analysis of 687 necropsies of patients with renal cell carcinoma, four cases had MGBs[3]. However, the data available on MGBs are only from autopsy series of certain malignancies such as melanoma or renal cell carcinoma, or reviews of a certain metastatic carcinoma to the GB such as melanoma[6,7], or in the form of single case reports of tumors such as melanoma[8-11], breast cancer[4], and hepatocellular carcinoma[5]. Furthermore, there is limited data on the proportion of MGBs among GB malignancies.
Malignant melanoma is reported to be the most common origin of MGBs[1]. In this study, malignant melanoma accounted for 10% of primary malignancies. Interestingly, the stomach was the most common primary origin of MGB in our study. This may result from bias arising from the small number of patients. However, the fact that stomach cancer is the most common cancer in Korea may have resulted in this finding[12].
In the analysis of the factors associated with survival, R0 resection was the only factor associated with prolonged survival, which can be taken as a matter of course. The presentation of MGB with acute cholecystitis was associated with poor survival. A possible explanation for this finding is that a major infectious episode, such as acute cholecystitis, may have had a major negative impact on the patient’s survival.
Our study has certain limitations. This study is based on information collected from patients with pathologically diagnosed GB malignancies only. The number of patients is small. In addition, the primary malignancies and treatments are varied. Nevertheless, this study provides some insight into the nature of MGBs.
In conclusion, MGBs accounted for 4.8% of all pathologically diagnosed GB malignancies over a period of 9 years. The stomach was the most common site of the primary malignancy. The overall median survival after diagnosis of the MGB was 8.7 mo. R0 resection was the only factor associated with a prolonged survival.
Metastases to the gallbladder (MGBs) are rare. There is limited data on the characteristics of patients with MGBs.
Although malignant melanoma and renal cell carcinoma are reported to metastasize to the GB, these data are based on autopsy series of these tumors. Despite the small number of cases, this report of 20 MGB cases is one of the largest among reports on MGBs.
The proportion of MGBs among pathologically confirmed GB malignancies is 4.8%. R0 resection is the only factor associated with a prolonged survival in MGB patients.
This is a well-written paper presenting material on patients with metastasis of the gallbladder. Although the series of patients is rather small, which is also discussed in the paper, it gives some information which is new and of scientific and clinical interest as well.
Peer reviewer: Curt Einarsson, Professor, Department of Medicine, Karolinska Institute, Karolinska University Hospital Huddinge, Dept of Gastroenterology and Hepatology, K 63, Huddinge SE-141 86, Sweden
S- Editor Li LF L- Editor Webster JR E- Editor Zheng XM
| 1. | DeMatos P, Anthony PP. Tumours of the gallbladder and extrahepatic bile ducts: Secondary tumours and melanoma. Pathology and genetics of tumours of the digestive system. World Health Organization classification of tumors. Lyon: IARC Press 2000; 217. |
| 2. | Dasgupta T, Brasfield R. Metastatic melanoma. A clinicopathological study. Cancer. 1964;17:1323-1339. |
| 3. | Weiss L, Harlos JP, Torhorst J, Gunthard B, Hartveit F, Svendsen E, Huang WL, Grundmann E, Eder M, Zwicknagl M. Metastatic patterns of renal carcinoma: an analysis of 687 necropsies. J Cancer Res Clin Oncol. 1988;114:605-612. |
| 4. | Zagouri F, Sergentanis TN, Koulocheri D, Nonni A, Bousiotou A, Domeyer P, Michalopoulos NV, Dardamanis D, Konstadoulakis MM, Zografos GC. Bilateral synchronous breast carcinomas followed by a metastasis to the gallbladder: a case report. World J Surg Oncol. 2007;5:101. |
| 5. | Hwang JH, Yoon YB, Kim YT, Kang HW, Yoon WJ, Jeong JB, Lee HS, Jang JY, Kim SW, Kim WH. A case of metastatic hepatocellular carcinoma presenting with isolated gallbladder polyp after successful treatment of the primary cancer. Korean J Gastroenterol. 2003;41:321-324. |
| 6. | Dong XD, DeMatos P, Prieto VG, Seigler HF. Melanoma of the gallbladder: a review of cases seen at Duke University Medical Center. Cancer. 1999;85:32-39. |
| 7. | Katz SC, Bowne WB, Wolchok JD, Busam KJ, Jaques DP, Coit DG. Surgical management of melanoma of the gallbladder: a report of 13 cases and review of the literature. Am J Surg. 2007;193:493-497. |
| 8. | Tuveri M, Tuveri A. Isolated metastatic melanoma to the gallbladder: is laparoscopic cholecystectomy indicated?: a case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2007;17:141-144. |
| 9. | Takayama Y, Asayama Y, Yoshimitsu K, Irie H, Tajima T, Hirakawa M, Ishigami K, Kakihara D, Sugitani A, Moroi Y. Metastatic melanoma of the gallbladder. Comput Med Imaging Graph. 2007;31:469-471. |
| 10. | Nelms JK, Patel JA, Atkinson DP, Raves JJ. Metastatic malignant melanoma of the gallbladder presenting as biliary colic: a case report and review of literature. Am Surg. 2007;73:833-835. |
| 11. | Marone U, Caracò C, Losito S, Daponte A, Chiofalo MG, Mori S, Cerra R, Pezzullo L, Mozzillo N. Laparoscopic cholecystectomy for melanoma metastatic to the gallbladder: is it an adequate surgical procedure? Report of a case and review of the literature. World J Surg Oncol. 2007;5:141. |
| 12. | Korea Ministry for Health, Welfare and Family Affairs. Cancer facts & figures 2008. : Korea Ministry for Health, Welfare and Affairs 2008; . |