Published online Sep 21, 2009. doi: 10.3748/wjg.15.4467
Revised: August 15, 2009
Accepted: August 22, 2009
Published online: September 21, 2009
A patient with obstructive jaundice was examined by multidetector row helical computed tomography (MDCT) and magnetic resonance imaging (MRI), and his common bile duct was observed to be leading into the distal portion of the horizontal duodenum with a pancreaticobiliary union outside the duodenal wall. A mass was also found in the proximal jejunum. All the above findings were confirmed by subsequent surgery, thus contrast-enhanced MDCT and MRI with appropriate image post-processing could provide non-invasive and accurate information regarding anatomy and lesions of the pancreaticobiliary duct and duodenal union, which may improve the feasibility of surgery and reduce postoperative complications.
- Citation: Wu DS, Chen WX, Wang XP. Ectopic pancreaticobiliary drainage accompanied by proximal jejunal adenoma: A case report. World J Gastroenterol 2009; 15(35): 4467-4470
- URL: https://www.wjgnet.com/1007-9327/full/v15/i35/4467.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4467
Anomalous termination of the common bile duct (CBD) is not an uncommon anatomical variation with incidence ranging from 5.6% to 23%[1-3]. Pancreaticobiliary maljunction (PBM) is a congenital anomaly in which the pancreatic duct meets the bile duct outside of the duodenal wall. Previous studies using endoscopic retrograde cholangiopancreatography (ERCP) found some sporadic cases. As ERCP is invasive with serious complications, e.g. pancreatitis, computed tomography (CT) or magnetic resonance imaging (MRI) may be another diagnostic choice for these patients. However, few studies up till now have reported such cases by CT or MRI. This study reports findings of both multidetector row helical computed tomography (MDCT) and MRI in a patient with anomalous termination of CBD, PBM and proximal jejunal adenoma. Both MDCT and MRI provide non-invasive and accurate information about anatomy and lesions of the pancreaticobiliary duct and duodenal union (PDDU).
A 71-year-old woman presented with icteric skin and sclera for the past three months without fever, abdominal pain or distention, nausea or vomiting. Physical examination revealed no abdominal tenderness or mass. On admission, total and direct bilirubin levels were 138.5 μmol/L and 120 μmol/L respectively, alanine aminotransferase was 78 IU/L, aspartate aminotransferase was 184 IU/L, alkaline phosphatase was 1031 IU/L, and carcinoembryonic antigen and α-fetoprotein levels were within normal values. She had a history of cholecystectomy 18 years ago. MDCT and MRI were performed within a week. The scan parameters for the MDCT scanner (Sensation 16, Siemens Medical Solutions, Siemens, Germany) included 120 kVp, 121-124 mAs, 5-mm slice thickness, 1-mm reconstructive thickness, and a table speed of 24 mm/s (pitch, 1). Non-ionic contrast material 90 mL (Iohexol, 300 mg I/mL) was injected at a flow rate of 3 mL/s. The MR (1.5-T, Siemens Sonata, Siemens, Germany, Leonardo work station) scanning protocol included unenhanced axial T2W scan (HASTE; TR/TE, 6379 ms/83 ms), coronal T2W imaging (True-FISP; TR/TE, 3.8 ms/1.9 ms), magnetic resonance cholangiopancreatography (TSE; TR/TE, 100 ms/1.8 ms), axial T1W (GRE, TR/TE, 100 ms/1.8 ms, 70° flip angle) and Gadolinium-enhanced three-dimensional VIBE (TR/TE, 4.8 ms/2.2 ms, 70° flip angle) information. The images were retrospectively reviewed in consensus by two experienced radiologists who were unaware of other imaging and surgical findings.
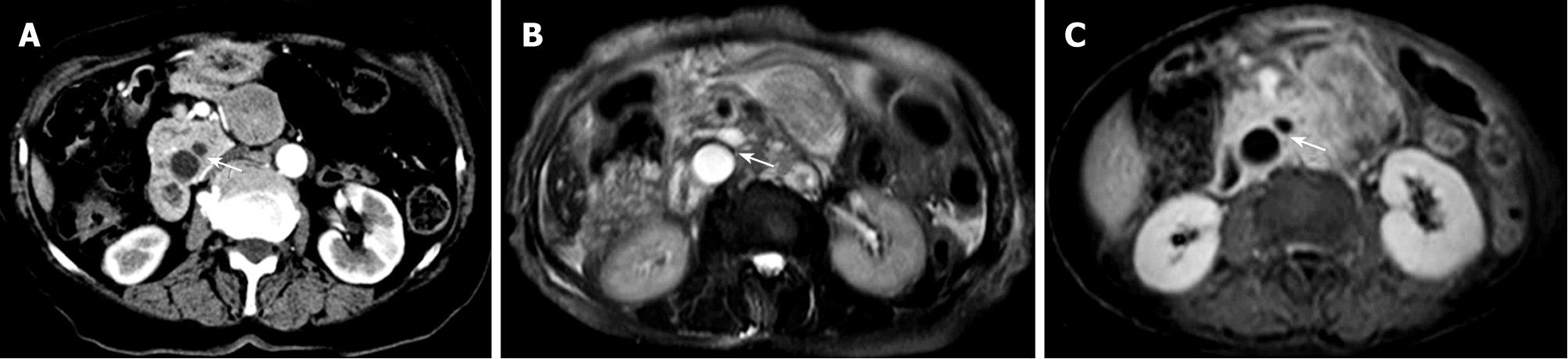
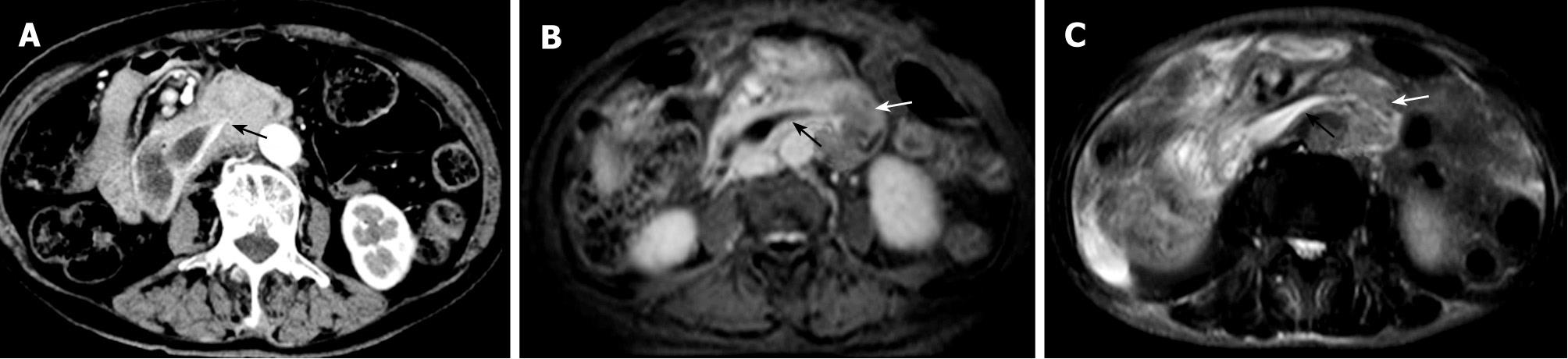
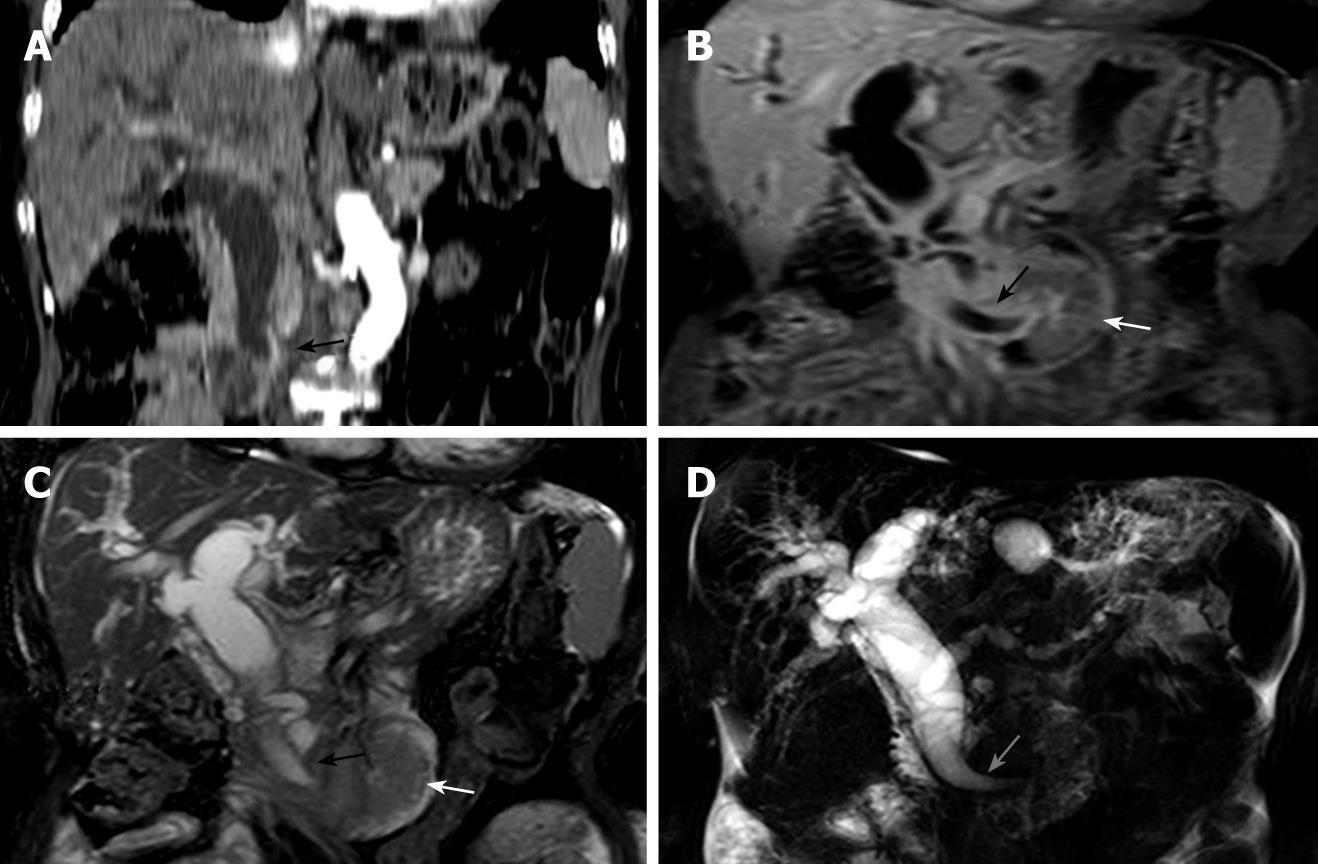
On the continuous transverse images of MDCT and MR, the CBD which was joined by the main pancreatic duct (MPD) outside the duodenal wall below the level of the uncinate process (Figure 1) was found to terminate at the distal portion of the horizontal duodenum (Figure 2). The coronal images of MDCT and MR, as well as MRCP images, showed a more clear presentation than transverse images regarding the ectopic pancreaticobiliary junction and low termination of the CBD at the horizontal duodenum (Figure 3). Both MPD and extra- and intrahepatic ducts showed extensive dilatation. The CBD was 2.4 cm at the largest diameter with a tapered configuration of the distal portion (Figure 2B and C). A discrete mass, surgically proven to be jejunal adenoma, was detected in the vicinity of the duodenojejunal flexure without dilatation of the proximal gut, but with adhesion to the proximal jejunum (Figure 2B and C). The mass was enhanced heterogeneously on contrast-enhanced CT and MR images.
During subsequent operation, the CBD was found to be dilated and it extended along the duodenum and terminated at the horizontal duodenum.
In 75% of cases, the common bile duct enters the posteromedial aspect of the descending duodenum through an intramural common channel called the hepatopancreatic ampulla (ampulla of Vater), where the CBD is joined by the main pancreatic duct and the terminal pancreatic duct is inferior and anterior to the CBD[4]. But the CBD can terminate at anomalous sites, including the third or fourth part of the duodenum, pyloric canal, duodenal bulb, or stomach[5,6-9]. The union of the pancreatic and biliary ducts can also locate outside the duodenal wall forming a very long common channel (usually more than 15 mm), which is representative of the appearance of a PBM.
The cause of an anomalous pancreaticobiliary system has been ascribed to unidentified abnormalities during embryogenesis. The ventral diverticulum of the foregut forms the liver, gallbladder, bile ducts and ventral pancreas. Abnormalities of the pancreaticobiliary junctions occur where these are demarcated. Boyden produced a hypothesis that ectopic bile duct drainage occurs because of the disproportional elongation and early subdivision of the primitive hepatic diverticulum which divides into the pars hepatica and pars cystica[10,11].
Multiple modalities permit depiction of the anatomy and lesions of the PDDU, including abdominal ultrasonography, ERCP, CT and MRI. Sonographic images often do not clearly display PBM and ectopic termination of the CBD, and ERCP is invasive and can be associated with significant complications, such as a 1% to 13.5% incidence of post-ERCP pancreatitis[12]. In contrast, MDCT and MRI are modern and non-invasive techniques revealing more anatomical details with no risk of procedure-induced complications. With appropriate image post-processing, MDCT and MRI may provide prompt identification of anatomy and abnormalities of the biliary and pancreatic ducts and the surrounding structures, which would help endoscopists and surgeons to discern the anatomy requiring special attention during ERCP operation, choledochoscopic exploration, endoscopic and choledochoscopic papillotomy and local resection of PDDU carcinomas. CT and MRI examinations can also offer valuable information in adults with underlying abnormalities of the pancreatic duct or biliary duct when the symptoms and signs are nonspecific (intermittent abdominal pain, occasional jaundice and cholangitis).
Based on the density of bile, it is easy to differentiate the CBD from surrounding soft tissue and trace its course until its termination on CT images. In high-spatial-resolution CT, the MPD and pancreaticobiliary junction can be well observed. MR imaging combined with magnetic resonance cholangiopancreatography (MRCP) has a distinctive advantage in revealing the pancreaticobiliary system. In terms of the intensity of bile, pancreatic and intestinal juice, the configuration and courses of the CBD, MPD, and enteric gut can be directly observed. At the same time, transverse images can offer additional information about the surrounding tissue and show tiny structures at the termination. In the present case, tracing the CBD from the level below the hepatic hilum until the third part of the duodenum in continuous planar, the termination was found at the distal aspect of the horizontal duodenum on CT and MR transverse images. This was clearer on coronal images than on transverse and MRCP images. Dilated CBD and pancreatic duct made it easy and definite to determine the area of termination. The union of the pancreatic and biliary ducts was seen to be located outside the duodenal wall.
Extensive dilatation of the pancreaticobiliary ducts accompanied by a mass located on the proximal jejunum was another characteristic finding in our case. Because the gut proximal to the adenoma showed no dilatation and the CBD revealed a tapered end, it could be concluded that dilatation of the pancreaticobiliary ducts was not the result of the space-occupied mass. Miyano et al[13] reported that the majority of patients with PBM in their study showed evidence of proximal biliary dilatation. Babbitt[14] proposed that PBM might be the etiology of choledochal dilatation and cyst formation. The resultant injury to the choledochus from enzymatic biliopancreatic reflux may then cause choledochal dilatation, choledochal fibrosis without dilatation, and possibly biliary atresia[15]. PBM may result in the frequent occurrence of biliary carcinoma and pancreatitis[16,17]. In this case, a PBM was found which may have been the cause of choledochal dilatation associated with choledochal injury and fibrosis and bile stasis, but there was no choledochal cyst formation, biliary carcinoma or pancreatitis. With bilio-pancreatic reflux, hypertension of the pancreatic duct could also result in dilatation of the MPD.
In summary, MDCT and MR imaging, with appropriate image post-processing, could provide non-invasive and accurate information about anatomy and lesions of the PDDU, which may improve the feasibility of surgery and reduce postoperative complications.
Peer reviewer: Norbert Senninger, Professor, Department of General Surgery, University Clinics, Westphalian-Wilhelm’s-University, Waldeyerstrasse 1, D-48149 Muenster, Germany
S- Editor Li LF L- Editor Logan S E- Editor Ma WH
| 1. | Lee HJ, Ha HK, Kim MH, Jeong YK, Kim PN, Lee MG, Kim JS, Suh DJ, Lee SG, Min YI. ERCP and CT findings of ectopic drainage of the common bile duct into the duodenal bulb. AJR Am J Roentgenol. 1997;169:517-520. |
| 2. | Rosario MT, Neves CP, Ferreira AF, Luis AS. Ectopic papilla of Vater. Gastrointest Endosc. 1990;36:606-607. |
| 3. | Keddie NC, Taylor AW, Sykes PA. The termination of the common bile duct. Br J Surg. 1974;61:623-625. |
| 4. | Avisse C, Flament JB, Delattre JF. Ampulla of Vater. Anatomic, embryologic, and surgical aspects. Surg Clin North Am. 2000;80:201-212. |
| 5. | Lindner HH, Pena VA, Ruggeri RA. A clinical and anatomical study of anomalous terminations of the common bile duct into the duodenum. Ann Surg. 1976;184:626-632. |
| 6. | Kubota T, Fujioka T, Honda S, Suetsuna J, Matsunaga K, Terao H, Nasu M. The papilla of Vater emptying into the duodenal bulb. Report of two cases. Jpn J Med. 1988;27:79-82. |
| 7. | Turner MA, Cho SR, Messmer JM. Pitfalls in cholangiographic interpretation. Radiographics. 1987;7:1067-1105. |
| 8. | Kanematsu M, Imaeda T, Seki M, Goto H, Doi H, Shimokawa K. Accessory bile duct draining into the stomach: case report and review. Gastrointest Radiol. 1992;17:27-30. |
| 9. | Doty J, Hassall E, Fonkalsrud EW. Anomalous drainage of the common bile duct into the fourth portion of the duodenum. Clinical sequelae. Arch Surg. 1985;120:1077-1079. |
| 10. | Moore KL, Persaud TVN. The developing human. 6th ed. Philadelphia: W.B. Saunders 1998; 276-282. |
| 11. | Mortele KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006;26:715-731. |
| 12. | Pande H, Thuluvath P. Pharmacological prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Drugs. 2003;63:1799-1812. |
| 13. | Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg. 2000;9:187-195. |
| 14. | Babbitt DP. [Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb]. Ann Radiol (Paris). 1969;12:231-240. |
| 15. | Ladd AP, Rescorla FJ. Anomalous biliary drainage associated with pancreaticobiliary maljunction and nondilatation of the common bile duct. J Pediatr Surg. 2003;38:E13-E15. |
| 16. | Kamisawa T, Matsukawa M, Amemiya K, Tu Y, Egawa N, Okamoto A, Aizawa S. Pancreatitis associated with pancreaticobiliary maljunction. Hepatogastroenterology. 2003;50:1665-1668. |
| 17. | Kamisawa T, Amemiya K, Tu Y, Egawa N, Sakaki N, Tsuruta K, Okamoto A, Munakata A. Clinical significance of a long common channel. Pancreatology. 2002;2:122-128. |