Published online Sep 14, 2009. doi: 10.3748/wjg.15.4334
Revised: August 2, 2009
Accepted: August 9, 2009
Published online: September 14, 2009
A 33-year-old woman who presented with epigastric discomfort and diarrhea underwent an abdominal ultrasound (US). This investigation and subsequent contrast-enhanced computed tomography, magnetic resonance imaging and endoscopic US with fine needle aspiration (FNA) revealed a 40 mm well-circumscribed mass in the uncinate process of the pancreas. Findings were suggestive of a mucinous or solid-cystic pseudopapillary tumor of the pancreas, although other lesions such as a non-functioning neuroendocrine tumor could not be ruled out. FNA samples were negative for malignant cells, but of limited value due to poor cellularity. It was decided to surgically remove the tumor because malignancy could not be discounted. Multiple intraoperative biopsies were suggestive of mesenchymal tumor and consequently a conservative resection (uncinatectomy) was performed. The postoperative course was uneventful. The definitive diagnosis was ganglioneuroma. Immunocytochemistry showed positive staining with vimentin, S-100 protein, neurofilament and neuron-specific enolase. Ganglioneuroma is a rare benign tumor that can also present as a pancreatic tumor. Uncinatectomy is feasible, safe and a good surgical technique for the treatment of non-malignant tumors located in the uncinate process of the pancreas.
- Citation: Poves I, Burdío F, Iglesias M, Martínez-Serrano MLÁ, Aguilar G, Grande L. Resection of the uncinate process of the pancreas due to a ganglioneuroma. World J Gastroenterol 2009; 15(34): 4334-4338
- URL: https://www.wjgnet.com/1007-9327/full/v15/i34/4334.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4334
Ganglioneuroma is a rare benign soft tissue tumor that arises from sympathetic nerve fibers. It is most frequently discovered during childhood or in young adults. The two most common presentations are in the mediastinum and retroperitoneum[1,2]. Although often difficult and not always possible, a preoperative diagnosis can be obtained by fine-needle aspiration (FNA)[1-3]. Clinical features, FNA and histological findings have been accurately described[3]. Adequate treatment consists of radical resection of the whole tumor and definitive diagnosis is obtained after surgical removal by morphologic examination of the complete specimen.
Most solid pancreatic masses are malignant and extended radical surgery is usually the standard of care. Conservative surgery of the pancreas has been advocated mostly for benign or premalignant lesions, most of which are cystic or neuroendocrine tumors (NETs)[4,5]. Uncinatectomy is a relatively novel surgical technique recently described for the treatment of non-malignant lesions[6].
We present the case of a young woman who had an apparent solid-cystic pancreatic mass in the uncinate process of the head of the pancreas and who was treated by conservative resection (uncinatectomy), with a definitive diagnosis of ganglioneuroma. Informed consent for writing this article has been obtained from the patient.
A 33-year-old woman was diagnosed with a well-circumscribed pancreatic mass measuring 40 mm in diameter in the head of the pancreas. The mass was discovered during the course of an abdominal ultrasound performed while the patient was being assessed for epigastric pain and diarrhea. The physical examination did not reveal any relevant findings. Serum analysis showed a discrete hypochromic microcytic anemia only. On initial abdominal ultrasound (US), the lesion appeared to have a solid consistency. An abdominal contrast-enhanced computed tomography (CT), contrast-enhanced magnetic resonance imaging (MRI) and endoscopic ultrasound (EUS) with FNA biopsy were all carried out to complete the patient’s assessment. Tumoral (CA 19.9, CEA) and hormonal markers were normal. Following the guidelines of our centre, the study protocol for pancreatic nodules was followed.
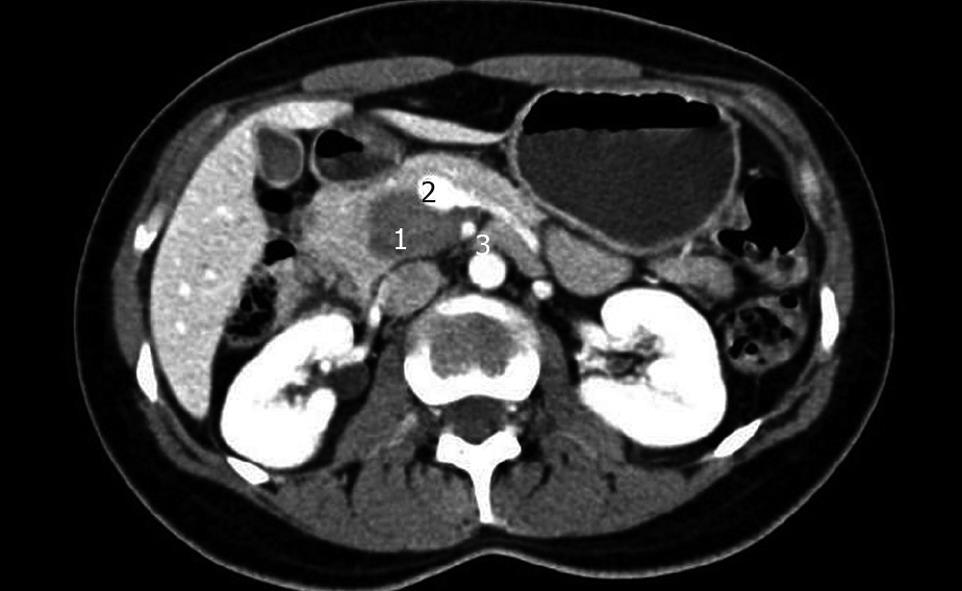
This examination showed the presence of a hypodense, non-infiltrative tumor measuring 36 mm × 22 mm × 36 mm in both arterial and portal phases, with the appearance of having internal walls, located in the head of the pancreas and occupying the uncinate process in close contact with the superior mesenteric artery and vein, celiac trunk and hepatic artery. These findings were suggestive of a cystic or solid-cystic pseudopapillary tumor of the pancreas.
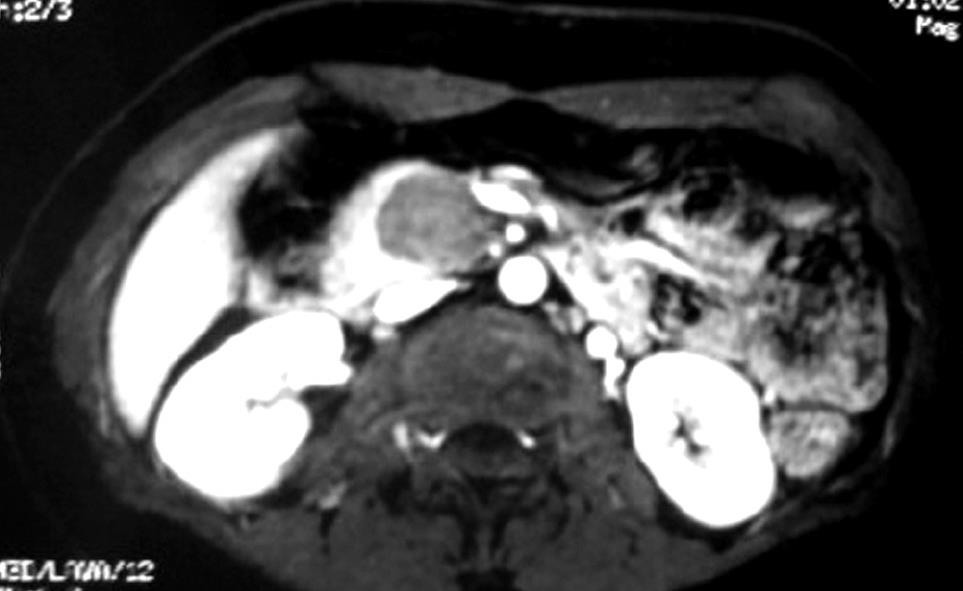
This examination showed a hypointense-T1 lesion that did not present any modifications following IV contrast administration (Gadolinium) that would be suggestive of a mucinous pancreatic tumor.
This examination showed a 42 mm × 21 mm well-defined, non-infiltrative and heterogeneous mass in the uncinate process of the pancreas, in contact with the portal-mesenteric axis. There were no pathologic lymph nodes and the remaining pancreas looked normal. The pancreatic duct was not dilated. Repeated direct FNA showed a tumor of extremely hard consistency, which made it difficult to obtain good quality samples. The ones obtained were negative for malignant cells, but of limited cellularity.
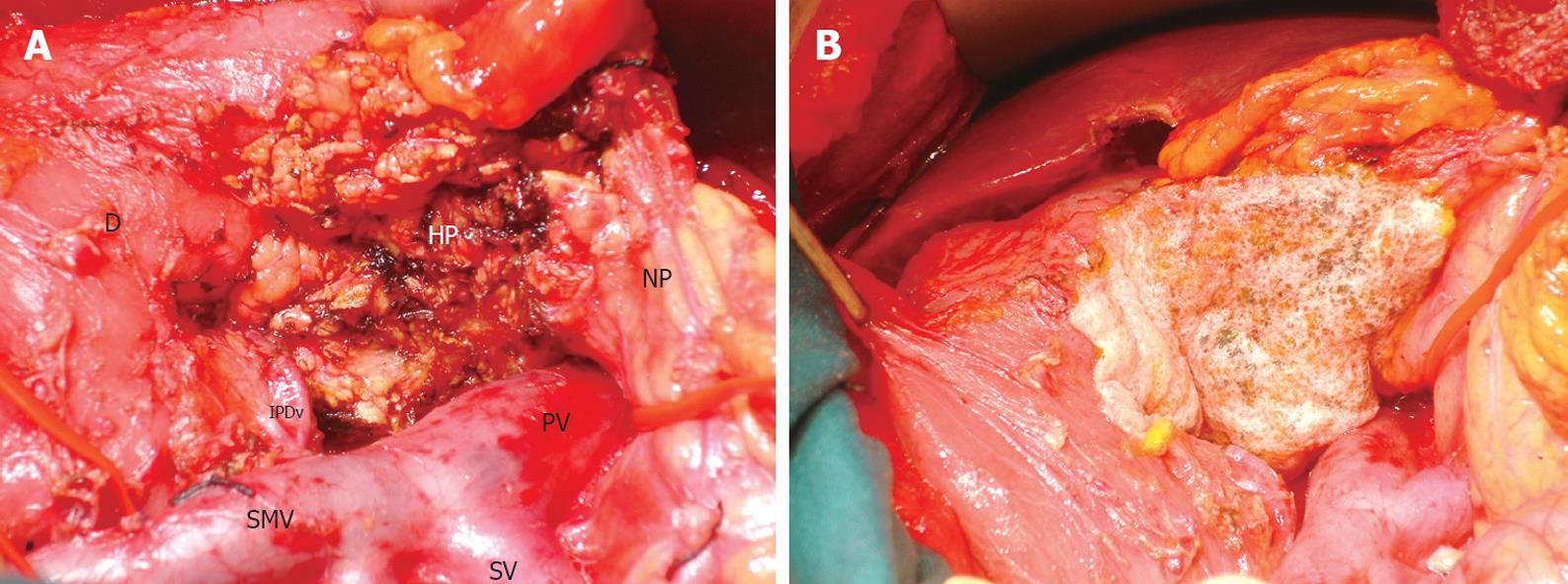
Although the diagnosis was not clear, it was decided to surgically remove the tumor because of a suspected solid-cystic pseudopapillary tumor or a non-functioning NET. Informed consent for conducting the protocol study and posterior operation was obtained from the patient. The operation was carried out through a right subcostal incision extended slightly to the left. During the exploration a well-delineated, non-infiltrative mass that occupied the uncinate process of the head of the pancreas was found. The mass was attached to the portal and superior mesenteric veins and to the superior mesenteric artery. Intraoperative multiple tumor biopsies (three tru-cut) showed fibrous tissue with some histiocytic cells suggestive of mesenchymal tumor. Intraoperative excisional biopsy of the intraaortic-cava, portal and hepatic lymph nodes showed no malignancy. Inferior pancreato-duodenal vessels were preserved. A complete resection of the uncinate process with preservation of the duodenum and the head of the pancreas was then performed (Figure 3A). Harmonic scalpel (Ethicon Endo-Surgery, Johnson & Johnson, Cincinnati, OH, USA) was used for cutting the pancreatic parenchyma. Cholecystectomy was carried out and a posterior cholangiography showed no leaking in the bile or in the pancreatic ducts. TachoSil® (Nycomed Pharma S.A.) sealant was applied, wrapping the head of the pancreas to prevent the formation of a pancreatic fistula (Figure 3B). An aspirative drain was established from the bed of the pancreatic resection site. The postoperative course was uneventful, and the patient was discharged on the sixth day.
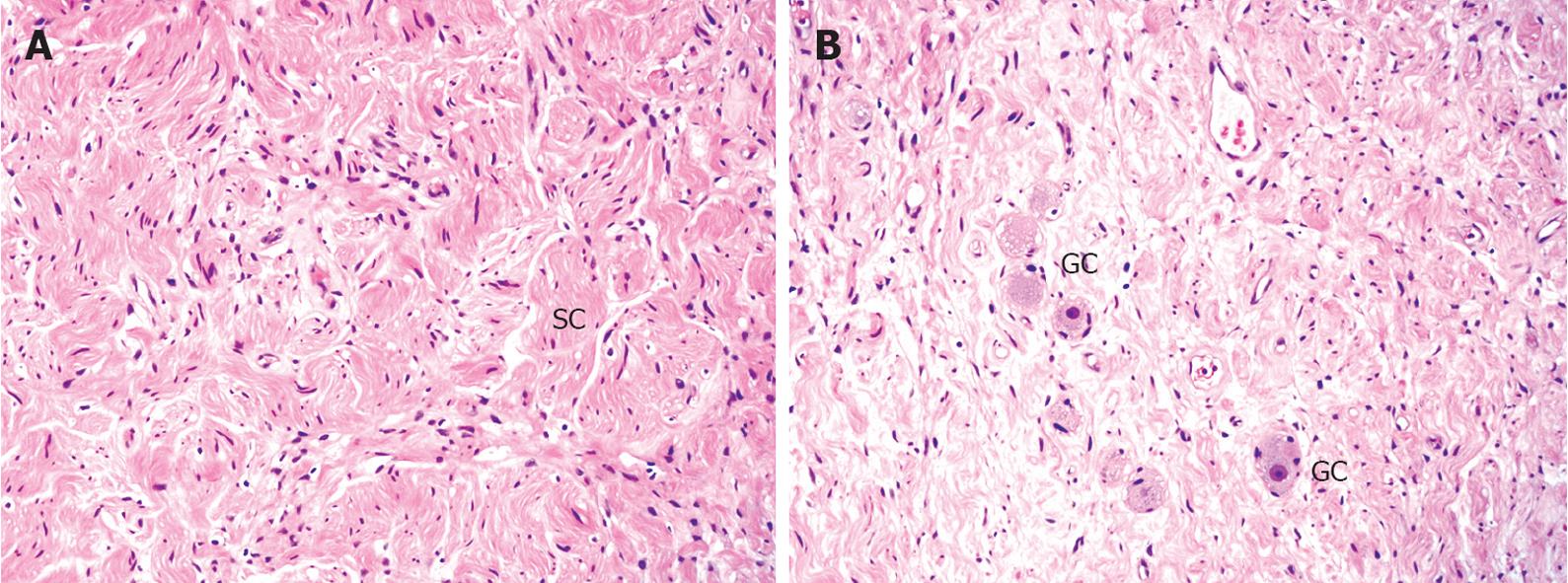
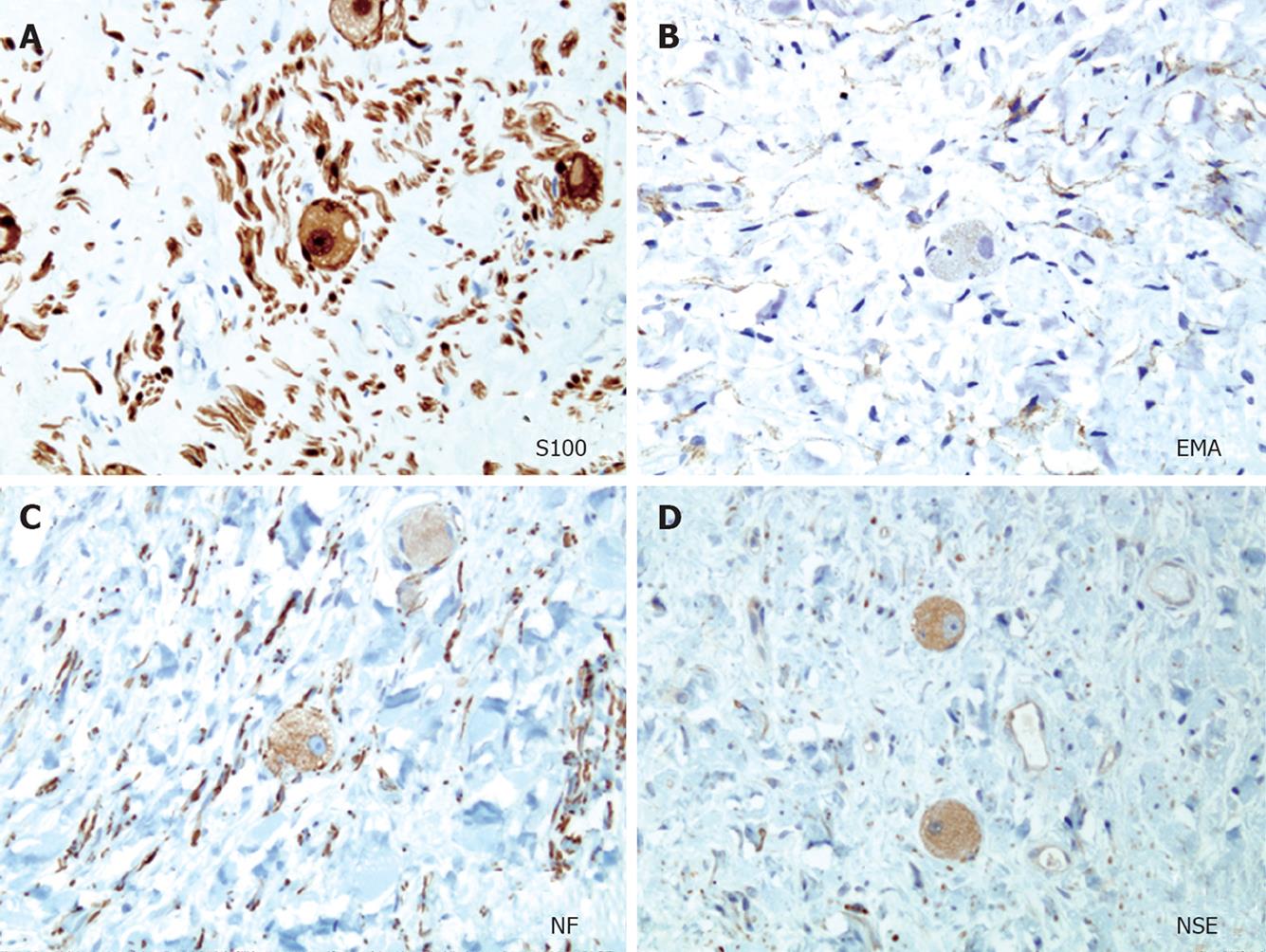
The definitive diagnosis was a ganglioneuroma (Figures 4, 5 and 6). The immunocytochemistry study showed positive staining with vimentin, S-100 protein, neurofilament and neuron-specific enolase (Figure 6).
Ganglioneuromas are very rare soft tissue tumors composed of gangliocytes and mature stroma[1,3,7]. They usually consist of benign masses that produce symptoms caused by their growth and location. Ganglioneuromas are usually asymptomatic and are often discovered casually during the course of explorations when looking for other diseases. Although the most frequent presentations are in the mediastinum and in the retroperitoneum[1-3], ganglioneuromas can also be found at any other location of the body such as in the neck or pelvis. In our review of the literature we have not been able to find any previous description of a pancreatic localization. Diagnostic imaging is very difficult because ganglioneuromas present as a non-specific solid mass. MRI seems to be the most accurate diagnostic imaging method although not a definitive one[7]. Unlike in other tumors, FNA is not always definitive, but its usefulness has been proven in some cases. A definitive diagnosis can only be reached after morphological examination of the removed specimen. Adequate treatment of ganglioneuromas is total surgical removal.
Retroperitoneal ganglioneuromas usually present as sarcomatous soft tissue tumors. In the case we present here, the macroscopic appearance of the tumor was that of a pancreatic mass with limits that extended into the pancreas as confirmed by all the imaging studies performed. Although it can be hypothesized that these tumors usually originate from peripancreatic nerve fibers, they invade pancreatic tissue, as it is impossible to find a plane between the tumor and the pancreatic parenchyma. In fact, in this case the morphological macroscopic study showed that the mass was completely attached to the pancreas in a continuous manner (Figure 4A). The only way to obtain a definitive diagnosis and to provide total certainty of no malignancy was total excision of the tumor. A differential diagnosis, taking into account tumor characteristics and preoperative imaging results, was done to differentiate between mucinous cystadenoma, non-functioning NET and solid-cystic papillary tumor, all of which could have the potential to become malignant. NETs can also present as cystic lesions although this occurrence is rare[8]. Somatostatin receptor scintigraphy with octreoscan has been recommended as the best imaging technique in NETs, being able to visualize more than 70% of these type of tumors[9]. In our case, we decided not to perform this exploration because the decision for radical resection was proposed independently of this result. We preferred to carry out multiple tru-cut biopsies intraoperatively, prior to deciding what type of pancreatic resection to perform. Biopsy results were suggestive of a benign soft tissue tumor, although some malignant entities such as pseudoinflammatory tumor or primary malignant fibrous histiocytoma could not be completely ruled out before the tumor was removed in its entirety. Local resection without standard lymphadenectomy was performed.
Further knowledge gained over the last few years regarding the anatomy of the pancreas has helped to develop the concept of conservative surgery. Conservative surgery has gained popularity among surgeons and not only for lesions located in the left pancreas[10]. Preserving the duodeno-pancreatic region is an issue for tumors that are also nested in the head of the pancreas. Resection of the uncinate process is an alternative to pancreato-duodenectomy (PD) for the treatment of non-malignant or pre-malignant lesions located in this area. Sharma et al[6] described the technique used to perform an uncinatectomy for the treatment of intraductal papillary mucinous neoplasms. Some other procedures such as resection of the head of the pancreas with preservation of the duodenum, median or central pancreatectomy, or enucleation, can be carried out depending on the type and precise location of the lesion. When these procedures have to be carried out, it is mandatory to obtain adequate preoperative or intraoperative confirmation of the benign nature of the samples. The postoperative course and long term sequelae are much better for conservative surgery than for PD.
As with enucleation, the main concern when performing an uncinatectomy is the risk of leakage into the main pancreatic duct. To minimize the risk of this severe complication, direct intraoperative US exploration is highly recommended during resection. Nevertheless, in many cases the pancreatic duct is narrow and is hard to identify. Intraoperative cholangiography and retrograde contrast back filling of the pancreatic duct can be an option for assessing the integrity of both the biliary and pancreatic ducts.
In conclusion, ganglioneuroma is a rare benign tumor that can also present as a pancreatic tumor. When a favorable location permits it, conservative resection of the pancreas is the treatment of choice. Uncinatectomy is feasible, safe and a good surgical technique for the treatment of non-malignant tumors located in the uncinate process of the pancreas.
Peer reviewer: Masaki Nagaya, MD, PhD, Islet Transplantation and Cell Bilology, Joslin Diabetes Center, One Joslin Place, Joslin Diabetes Center, Boston 02215, United States
S- Editor Li LF L- Editor Logan S E- Editor Ma WH
| 1. | Yen H, Cobb CJ. Retroperitoneal ganglioneuroma: a report of diagnosis by fine-needle aspiration cytology. Diagn Cytopathol. 1998;19:385-387. |
| 2. | Jain M, Shubha BS, Sethi S, Banga V, Bagga D. Retroperitoneal ganglioneuroma: report of a case diagnosed by fine-needle aspiration cytology, with review of the literature. Diagn Cytopathol. 1999;21:194-196. |
| 3. | Domanski HA. Fine-needle aspiration of ganglioneuroma. Diagn Cytopathol. 2005;32:363-366. |
| 4. | Fernandez-Cruz L, Cosa R, Blanco L, Levi S, Lopez-Boado MA, Navarro S. Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg. 2007;11:1607-1621; discussion 1621-1622. |
| 5. | Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, Wilson SD, Pitt HA. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004;239:651-657; discussion 657-659. |
| 6. | Sharma MS, Brams DM, Birkett DH, Munson JL. Uncinatectomy: a novel surgical option for the management of intraductal papillary mucinous tumors of the pancreas. Dig Surg. 2006;23:121-124. |
| 7. | Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002;22:911-934. |
| 8. | Ahrendt SA, Komorowski RA, Demeure MJ, Wilson SD, Pitt HA. Cystic pancreatic neuroendocrine tumors: is preoperative diagnosis possible? J Gastrointest Surg. 2002;6:66-74. |