Published online Aug 7, 2009. doi: 10.3748/wjg.15.3687
Revised: April 24, 2009
Accepted: May 1, 2009
Published online: August 7, 2009
Fibroepithelial polyps or hypertrophied anal papillae are essentially skin tags that project up from the dentate line and the junction between the skin and the epithelial lining of the anus. They are usually small in size, but sometimes they become enlarged, causing unexpected medical conditions. An extremely rare case of a giant hypertrophied anal papilla complicated by obstructive ileus is reported. Fibroepithelial anal polyp, despite its size, should be included in the differential diagnosis of a smooth mass located near the anal verge, especially in a patient with a history of chronic anal irritation or infection.
- Citation: Galanis I, Dragoumis D, Tsolakis M, Zarampoukas K, Zarampoukas T, Atmatzidis K. Obstructive ileus due to a giant fibroepithelial polyp of the anus. World J Gastroenterol 2009; 15(29): 3687-3690
- URL: https://www.wjgnet.com/1007-9327/full/v15/i29/3687.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3687
Fibroepithelial polyps of the anus, also referred to as hypertrophied anal papillae, are structures formed by hyperplasia of connective tissue in the vicinity of the anal columns. They are usually relatively small in size and asymptomatic. Enlargement of anal papillae is thought to be due to a hyperplastic response of the modified ectoderm to chronic irritation, injury or infection. Following repeated inflammatory episodes they can hypertrophy into the rectum and be confused with adenomatous polyps. Fibroepithelial polyps of the anus should be included in the differential diagnosis of a smooth mass located near the anal verge, especially in a patient with a history of chronic anal irritation or infection. To our knowledge, this is the first case of a giant fibroepithelial polyp of the anus complicated by obstructive ileus: there is only one similar case study in the medical literature regarding a giant hypertrophied anal papilla complicated by massive anal bleeding and prolapse[12].
A 67-year-old woman was admitted to the emergency room with a diffuse, cramping abdominal pain of progressive onset, tendency to vomit and constipation for 5 d. She had experienced similar episodes of intermittent abdominal pain, anal bleeding and persistent perianal pain due to long-standing hemorrhoidal disease over the last 7 years. Despite having been aware of the presence of chronic constipation, she had not sought timely medical treatment. Her family history was unremarkable, as was her medical history, except for clonazepam intake due to epileptic episodes during her childhood.
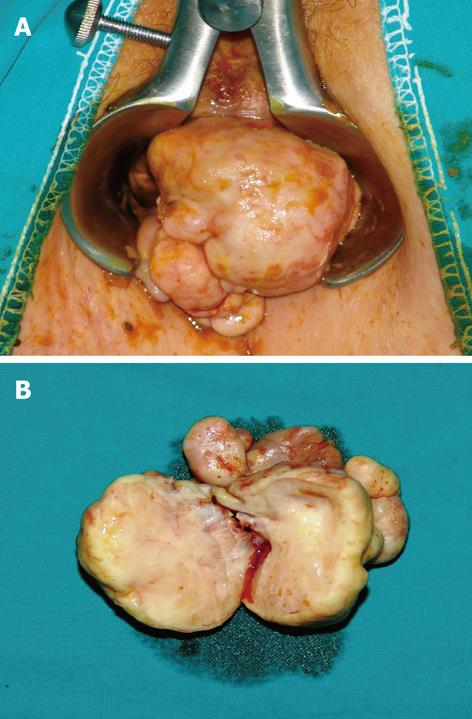
On physical examination, she had reduced bowel sounds, while the upper abdomen was distended with mild tenderness on palpation. Digital examination was negative for the presence of blood in the rectum, but revealed a giant elastic mass with convoluted grooves on a smooth surface in the distal rectum. This lesion was located 2 cm above the dentate line, obstructing the intestinal lumen. Preoperative examinations, consisting of a full blood count, serum kidney and liver functions, as well as cancer markers (CEA, CA 19-9), were within normal limits. Plain abdominal X-rays revealed the presence of dilated small intestine with air-fluid levels. A computed tomography of the abdomen and pelvis demonstrated the presence of a mass in the rectum (Figure 1). Anal examination under anesthesia was carried out. A giant (measuring 15 cm × 12 cm) smooth mass attached to a wide pedicle extending over the entire posterior wall of the anal canal, above the dentate line, was easily observed (Figure 2). During the proctoscopy, biopsy specimens and frozen section analysis confirmed the benign nature of the lesion.
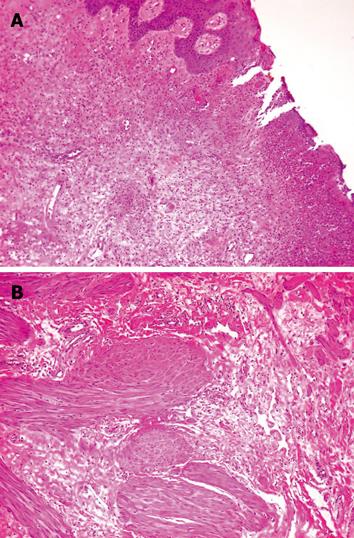
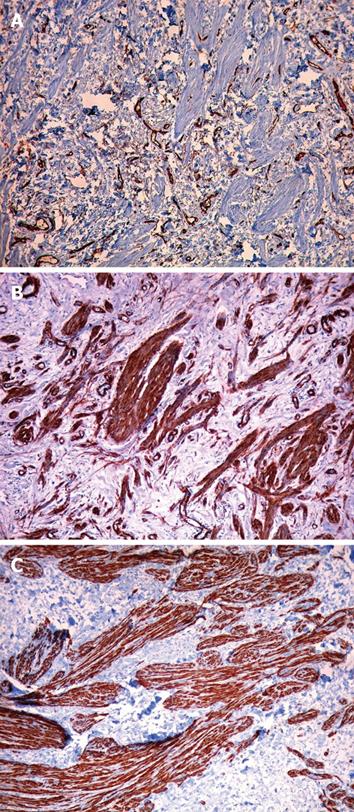
The huge mass was uneventfully removed by local excision with the the aid of an electrothermal bipolar vessel sealer (LigaSure Precise®). The histological assay of the resected specimen showed fibrous tissue covered by multilayered squamous epithelium, many small dilated vessels filled with red blood cells, scattered smooth muscle fibers and a superficial ulceration of the fibrous stroma (Figure 3). In all immunohistochemical sections from the giant fibroepithelial polyp, spindle and stellate mononucleated stromal cells were positive for CD34, SMA (Smooth Muscle Actin) and desmin (Figure 4).
The histological and immunohistochemical findings therefore established the diagnosis of fibroepithelial polyp of the anus. The patient presented no postoperative complications and was discharged after 3 d of hospitalization.
Fibroepithelial polyps of the anus, also known as hypertrophied anal papillae, are common lesions that have attracted little attention in the medical literature. They are enlarged, benign, polypoid projections of the anal squamous epithelium and the subepithelial connective tissue. These lesions are present in 45% of patients who undergo proctoscopic examination and are considered to be acquired triangular protrusions that arise from the base of the rectal columns of Morgagni at the dentate line[2]. As regards our patient, this is a report of a unique case of a very oversized fibroepithelial polyp of the anus which finally led to intestinal obstruction.
Clinically, these polyps may have the appearance of hemorrhoids, but they do not display thick-walled veins or any evidence of hemorrhage and organizing thrombi. In persons with poor anal hygiene, local disease or bowel dysfunction, these structures may become inflamed and edematous. They are usually small in size, asymptomatic and can be regarded as normal anatomic variations. Most anal papillae are 2-5 mm at their greatest dimension, although rarely they may exceed 2 cm. Enlargement of a fibroepithelial polyp to more than 3 cm in diameter is rare, and it is therefore necessary to differentiate such lesions from malignant tumors including leiomyosarcoma, anorectal carcinoma and malignant lymphoma.
Hypertrophied anal papillae are liable to trauma during the passage of stools and may become inflamed. Furthermore, they produce symptoms by projecting at the anal orifice during defecation and sometimes require digital repositioning, strongly simulating a rectal prolapse. Pruritus, foreign body sensation, mucus discharge, sense of incomplete evacuation and discomfort while sitting are the prevailing symptoms associated with this medical condition. The location of a smooth mass just inside the anal verge should suggest the possibility of a fibroepithelial polyp, especially in a patient with a history of chronic anal irritation or locoregional infection[23].
Endoscopically, a fibroepithelial polyp can be easily distinguished from an adenomatous polyp by several distinctive characteristics: (1) its mucosa is whitish compared with the reddish appearance of an adenomatous polyp, (2) the “stalk” of a hypertrophied anal papilla originates from the squamous side of the dentate line, (3) closure of the biopsy forceps on a fibroepithelial polyp results in pain, and (4) biopsy of these structures always demonstrates squamous epithelium. On the other hand, radiographic demonstration (on barium enema examination or computed tomography) of a fibroepithelial polyp is uncommon and occurs only when it becomes large enough to prolapse into the rectum. The differential diagnosis should always include internal hemorrhoids, rectal polyp, anal carcinoma and submucosal anorectal tumor[45].
Groisman et al[6] studied the histological, immunohistochemical and ultrastructural features of a series of 40 fibroepithelial polyps of the anus. The authors concluded that fibroepithelial polyps of the anus are benign lesions characterized by the presence of mononucleated and multinucleated, sometimes atypical, CD34+ stromal cells showing fibroblastic and myofibroblastic differentiation. They also suggested that polyps harboring atypical cells are those of large size. The morphologic resemblance between these lesions and normal anal mucosa supports the hypothesis that fibroepithelial polyps may represent a reactive hyperplasia of the subepithelial connective tissue of the anal mucosa. Mast cell infiltration, by means of their fibrogenic, fibrolytic and angiogenic activities, may play an important role in the pathogenesis of these structures.
The presence of smooth muscle bundles and hyalinized vascular changes at the base of anal fibroepithelial polyps has also been reported. The rectal muscularis mucosa may be found in the upper part of the anal transitional zone. An increase in smooth muscle bundles could be the result of the hyperplastic response which caused anal fibroepithelial polyps to form a central core, and to become enlarged[7]. In our case study, the presence of abundant smooth muscle fibers in the stroma merely emphasizes the extreme enlargement of the polyp.
Another prominent histological feature of fibroepithelial polyps of the anus, but of uncertain significance, is the eosinophilic epithelial vacuolation. This is characterized by the accumulation of PAS-positive homogenous eosinophilic material in superficial keratinocytes. This change may be a non-specific reaction to mechanical trauma, particularly given its propensity to afflict the apex of polyps. Pathologists should be very careful to avoid a misdiagnosis of extramammary Paget disease or oral white sponge nevus, which may sometimes affect anal epithelium[8].
A fibroepithelial polyp that starts projecting into the anal canal requires attention and proper therapeutic strategy. Complete removal by crushing of the base and excision after using an electrothermal bipolar vessel sealing system (EBVS-LigaSure), electrocauterization or ultrasonic energy (Harmonic Scalpel) has been suggested by many authors. Some other surgeons have found that the use of radio frequency devices is a quick, easy and significantly complication-free procedure for these pathological entities. This type of device can ablate the papillae instantly, while the fibrous polyps can be excised after coagulation of the bases and thereafter the pedicles[9].
Although in our case we had no other option but to remove this giant polyp due to the intestinal obstruction it caused, in general, complete removal of these structures, regardless of the method used, offers definite therapeutic benefits and results in improved patient satisfaction.
| 1. | Kusunoki M, Horai T, Sakanoue Y, Yanagi H, Yamamura T, Utsunomiya J. Giant hypertrophied anal papilla. Case report. Eur J Surg. 1991;157:491-492. |
| 2. | Gupta PJ. A study of the symptomatology of hypertrophied anal papillae and fibrous anal polyps. Bratisl Lek Listy. 2005;106:30-33. |
| 3. | Gupta PJ, Kalaskar S. Removal of hypertrophied anal papillae and fibrous anal polyps increases patient satisfaction after anal fissure surgery. Tech Coloproctol. 2003;7:155-158. |
| 4. | Heiken JP, Zuckerman GR, Balfe DM. The hypertrophied anal papilla: recognition on air-contrast barium enema examinations. Radiology. 1984;151:315-318. |
| 5. | Hizawa K, Sakamoto K, Nakahara T, Inuzuka S, Akagi K, Shimono R, Iwai K, Matsumoto T. Endosonographic demonstration of a giant fibrous polyp of the anus. Gastrointest Endosc. 2001;53:824-825. |
| 6. | Groisman GM, Polak-Charcon S. Fibroepithelial polyps of the anus: a histologic, immunohistochemical, and ultrastructural study, including comparison with the normal anal subepithelial layer. Am J Surg Pathol. 1998;22:70-76. |
| 7. | Sakai Y, Matsukuma S. CD34+ stromal cells and hyalinized vascular changes in the anal fibroepithelial polyps. Histopathology. 2002;41:230-235. |
| 8. | Beer TW, Carr NJ. Fibroepithelial polyps of the anus with epithelial vacuolation. Am J Surg Pathol. 1999;23:488-489. |
| 9. | Gupta PJ. Hypertrophied anal papillae and fibrous anal polyps, should they be removed during anal fissure surgery? World J Gastroenterol. 2004;10:2412-2414. |