Published online Aug 7, 2009. doi: 10.3748/wjg.15.3684
Revised: June 30, 2009
Accepted: July 7, 2009
Published online: August 7, 2009
Splenosis is a condition in which splenic tissue is present in a non-anatomical position. Implants of splenic tissue can mimic neoplasms and only specific examinations can confirm the correct diagnosis. Here we report a case of a 23-year-old male patient with a history of surgical splenectomy during childhood after trauma. He was admitted to the emergency department with acute bowel obstruction. An abdominal-pelvic computed tomography (CT) scan revealed small bowel obstruction and the presence of two rounded, solid masses located in the rectal-vescical pouch. Quantitative analyses of the different density values in the arterial phase and early portal venous phase demonstrated that these lesions were highly vascularised (92 and 97 Hounsfield Units, respectively). The hypothesis of an ectopic splenic mass was made after evaluation of the CT images and clinical history. The acute bowel obstruction caused by adhesive intestinal syndrome was resolved by surgical adhesiolysis. The smallest mass adherent to the rectum was removed. Histopathologic examination confirmed the benign nature of the lesion, which consisted of splenic tissue.
- Citation: Garaci FG, Grande M, Villa M, Mancino S, Konda D, Attinà GM, Galatà G, Simonetti G. What is a reliable CT scan for diagnosing splenosis under emergency conditions? World J Gastroenterol 2009; 15(29): 3684-3686
- URL: https://www.wjgnet.com/1007-9327/full/v15/i29/3684.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3684
Splenosis is a condition in which splenic tissue is present in a non-anatomical position due to its auto-transplantation after splenic trauma or surgery causing injury to the splenic capsule. It can be found as a single mass or multiple intraperitoneal or pelvic masses that may or may not be associated with pain. In some cases, it can manifest as an acute abdominal pain secondary to the torsion of the splenic pedicle. These splenic implants can mimic neoplasms and only specific examinations can confirm the diagnosis. Although ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI) can help in localizing and establishing the size and structure of these implants and in determining their relationship with adjacent organs, they are non-specific examinations. Only by using specific agents that are selectively sequestrated by the reticulo-endothelial system [such as 99mTechnetium-labelled heat-denatured autologous red blood cells or 111Indium-labeled platelets, single photon emission computed tomography scans and recently ferumoxide-enhanced MRI (small iron oxide particles SPIO)] allow a specific diagnosis of intra-abdominal splenosis. However, these examinations cannot be performed in an emergency situation.
Several authors report the role of these advanced imaging techniques in the diagnosis of splenosis, however, there exist no studies in the literature reporting the use of imaging techniques in emergency situations.
Here we describe the role of contrast-enhanced CT in the diagnosis of splenosis in an emergency situation.
A 23-year-old male patient was admitted to the emergency department of our hospital with acute abdominal pain. He presented with fever, periumbilical colic-like pain, nausea and vomiting with absolute constipation. Clinical examination revealed a distended abdomen that was tender but not peritonitic and feverous. At auscultation, peristalsis was very slow. Digital rectal examination revealed a large lobulated mass imprinting the anterior wall of the rectum, while testicular palpation did not reveal abnormal findings. Laboratory results revealed the presence of leukocytosis. The patient had a history of childhood splenectomy for a blunt abdominal trauma caused by a horse’s kick. No other significant medical data were reported.
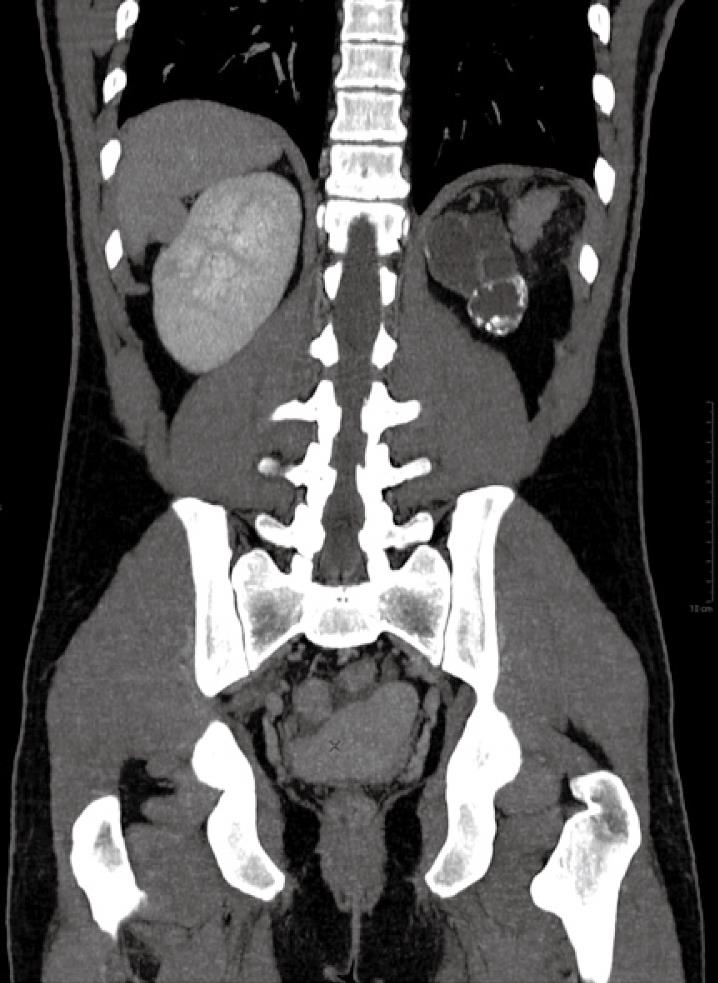
An abdomino-pelvic CT scan revealed a small bowel obstruction and two well-demarcated rounded solid masses (10 and 3.5 cm) located in the rectovesical pouch posterior to the prostate gland and the seminal vesicles. These lesions did not show any macroscopic contiguity with the surrounding organs (i.e. the prostate gland, the bladder, the seminal vesicles and the rectal ampulla). No lymphadenopathy (iliac or obturator group) or signs of invasion of the adipose tissue of the rectovesical pouch were found. These features excluded malignant behaviour of the lesions.
Pre-contrast CT images showed these masses were isodense to liver. In particular, a quantitative analysis of the density value was made by the positioning of multiple regions of interest (ROIs) into the lesions, demonstrating Hounsfield Unit (HU) values ranging between 55 and 60. In the post-contrast CT scans (after intravenous injection of 130 mL of contrast media, Ultravist, 3 mL/s flow rate), these lesions became homogeneously hyperdense (92 HU) in the arterial phase (no typical striped enhancement pattern) (Figure 1) and isodense in the early portal venous phase (Figure 2). Quantitative analyses of the different density values in the arterial and early portal venous phases demonstrated that these lesions were highly vascularised (92 and 97 HU, respectively). The enhancement pattern was similar to that of parenchymatous organs, such as the liver. The origin of the masses as being from the prostate or seminal vesicles was thereby ruled out because of the early and homogenous enhancement. On the basis of both the CT findings and clinical data, the splenic origin of these lesions was hypothesized.
The patient underwent surgery to resolve the intestinal occlusion. An adhesiolysis for small bowel obstruction secondary to adhesive intestinal syndrome was conducted. A mass was found in the rectovesical pouch attached to the bladder and to the prostate gland and was macroscopically compatible with splenic tissue. Another similar smaller mass was found adherent to the rectum (Figure 3). This mass was successfully removed. Histopathologic examination demonstrated the benign nature of the lesion, which consisted of splenic tissue. The larger mass was not removed as it was not associated with any clinical symptom.
Although splenic implants are generally asymptomatic, they can lead to recurrent episodes of abdomino-pelvic pain or small bowel obstruction secondary to adhesive bands to the splenic implants. Splenosis can be confused with other intra-abdominal masses. Differential diagnoses of splenosis include endometriosis, peritoneal mesothelioma, renal neoplasms, abdominal lymphomas and peritoneal metastatic implants[1]. Splenosis should be suspected in patients with a history of splenic trauma. Non-invasive diagnosis of splenosis needs integration of radiological and scintigraphic methods[2].
In patients with bowel obstruction, a history of splenic trauma and an occasional finding of an abdominal mass, contrast-enhanced CT scan is an efficient tool for the diagnosis of splenosis. In pre-contrast enhanced CT scans, normal splenic tissue appears homogenous with a density ranging between 56 and 65 HU, which is similar or slightly lower than that of normal liver tissue. After high flow-rate (3-4 mL/s) administration of contrast media, early post-contrast scans show an inhomogeneous impregnation with a cord-like pattern. This is probably related to the existence of a double blood-circulation inside the red pulp where areas of early enhancement represent fast circulation with direct connections between arterioles and venules, and areas of late enhancement represent a slower circulation with connections between the arterioles and the venules through the Billroth-channels[34]. The splenic parenchyma reaches a homogeneous enhancement approximately 1 min after contrast agent administration with density values ranging between 75 and 97 HU[5].
Although differential diagnosis includes a variety of other conditions presenting with a pelvic mass, the relation with the surrounding tissues and the contrast-enhancement characteristics can help in the diagnosis of splenosis. In particular, in the case we present, the absence of infiltration of the prostate gland, seminal vesicles and rectum ruled out the malignant nature of the masses. Furthermore, the enhancement pattern made a malignancy less probable, such as a sarcoma that would have presented as an inhomogeneous enhancement on both pre- and post-contrast images. The hypothesis of an ectopic splenic mass was made after an accurate evaluation of the CT images and correlation with clinical history.
In the case, we present demonstrates the importance of contrast-enhanced CT imaging with ROI analysis in the differential diagnosis of splenosis from other pelvic masses in emergency conditions.
| 1. | Imbriaco M, Camera L, Manciuria A, Salvatore M. A case of multiple intra-abdominal splenosis with computed tomography and magnetic resonance imaging correlative findings. World J Gastroenterol. 2008;14:1453-1455. |
| 2. | Kok J, Lin M, Lin P, Ngu C, Sam S, Loh C, Kociuba K. Splenosis presenting as multiple intra-abdominal masses mimicking malignancy. ANZ J Surg. 2008;78:406-407. |
| 3. | Urban BA, Fishman EK. Helical CT of the spleen. AJR Am J Roentgenol. 1998;170:997-1003. |
| 4. | Miles KA, McPherson SJ, Hayball MP. Transient splenic inhomogeneity with contrast-enhanced CT: mechanism and effect of liver disease. Radiology. 1995;194:91-95. |
| 5. | Nelson RC, Chezmar JL, Peterson JE, Bernardino ME. Contrast-enhanced CT of the liver and spleen: comparison of ionic and nonionic contrast agents. AJR Am J Roentgenol. 1989;153:973-976. |