Published online Jul 21, 2009. doi: 10.3748/wjg.15.3448
Revised: June 19, 2009
Accepted: June 26, 2009
Published online: July 21, 2009
Esophageal carcinosarcoma is a rare malignant tumor composing of both carcinomatous and sarcomatous elements. Endoscopic therapy is less invasive and may represent an alternative to esophagectomy for superficial esophageal carcinosarcoma. Here, we report a 61-year-old male who was diagnosed as esophageal carcinosarcoma and underwent endoscopic polypectomy with well tolerance and favorable prognosis. We also present a brief review of the literature.
- Citation: Ji F, Xu YM, Xu CF. Endoscopic polypectomy: A promising therapeutic choice for esophageal carcinosarcoma. World J Gastroenterol 2009; 15(27): 3448-3450
- URL: https://www.wjgnet.com/1007-9327/full/v15/i27/3448.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3448
Esophageal carcinosarcoma is a rare malignant neoplasm consisting of both carcinomatous and sarcomatous components[1]. Esophagectomy has been traditionally considered the first option for esophageal carcinosarcoma patients[1]. Endoscopic therapy is less invasive and allows the esophagus to be preserved, and may represent an alternative to esophagectomy for superficial esophageal carcinosarcoma. We here report a case of esophageal carcinosarcoma who underwent endoscopic polypectomy with well tolerance and favorable prognosis.
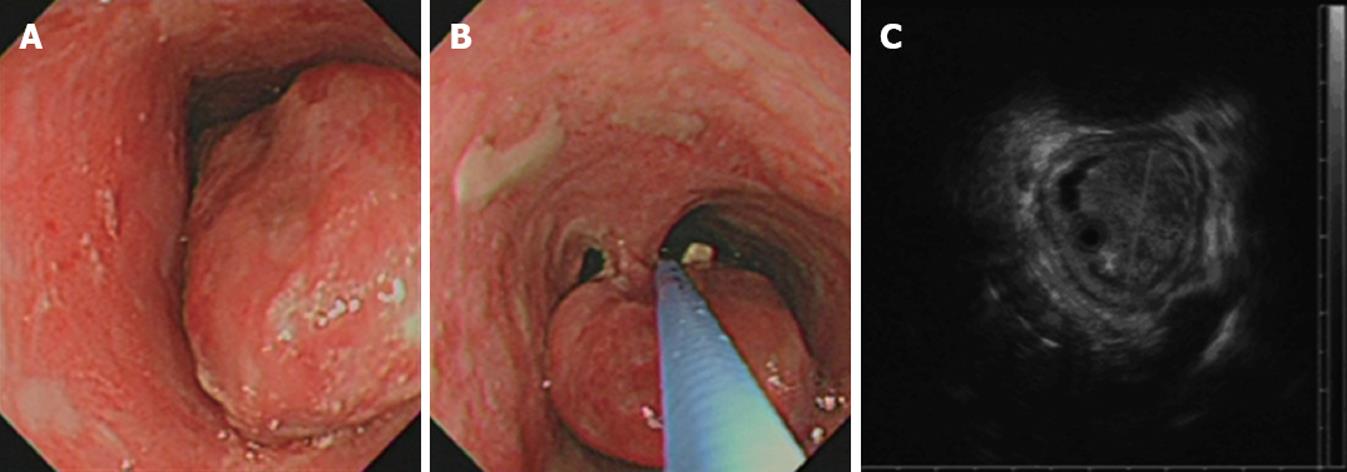
A 61-year-old male was admitted to our hospital with a 20-day history of progressive dysphagia. He was a heavy smoker and alcohol drinker, neither his medical nor family history included any relevant disease. Physical examination revealed no abnormalities. All serum tumor markers were normal. Barium meal showed a regularly-shaped circular stenosis in the upper esophagus. Endoscopy revealed a pedunculated polypoid tumor with ulcer on its surface. The tumor was located at 25-30 cm from the incisor teeth, and packed in the lumen of the esophagus (Figure 1A and B). Biopsy proved the mass to be a carcinosarcoma.
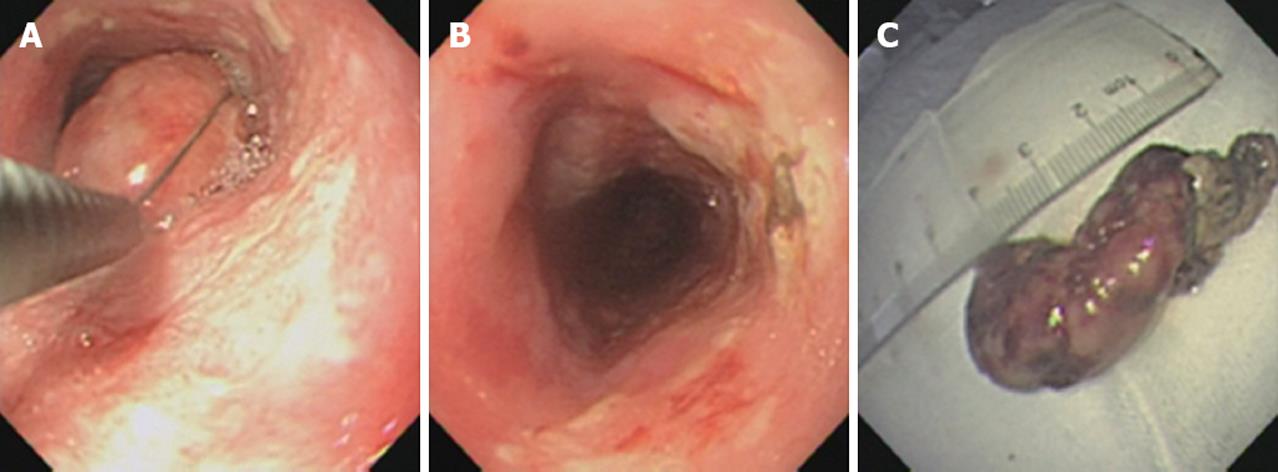
Endoscopic ultrasonography (EUS) and computed tomography (CT) scan were subsequently performed to show the stage of carcinosarcoma. EUS revealed a 5 cm × 3 cm × 3 cm hypoechoic mass with regular margins confined to the mucosal layer with no involvement of other layers or regional lymph nodes (Figure 1C). CT scan displayed an intraluminal mass but no evidence of metastases in brain, chest or abdominal organs. According to the clinical examinations, we performed an endoscopic polypectomy using a polypectomy loop to resect the bulky pedunculated tumor (Figure 2).
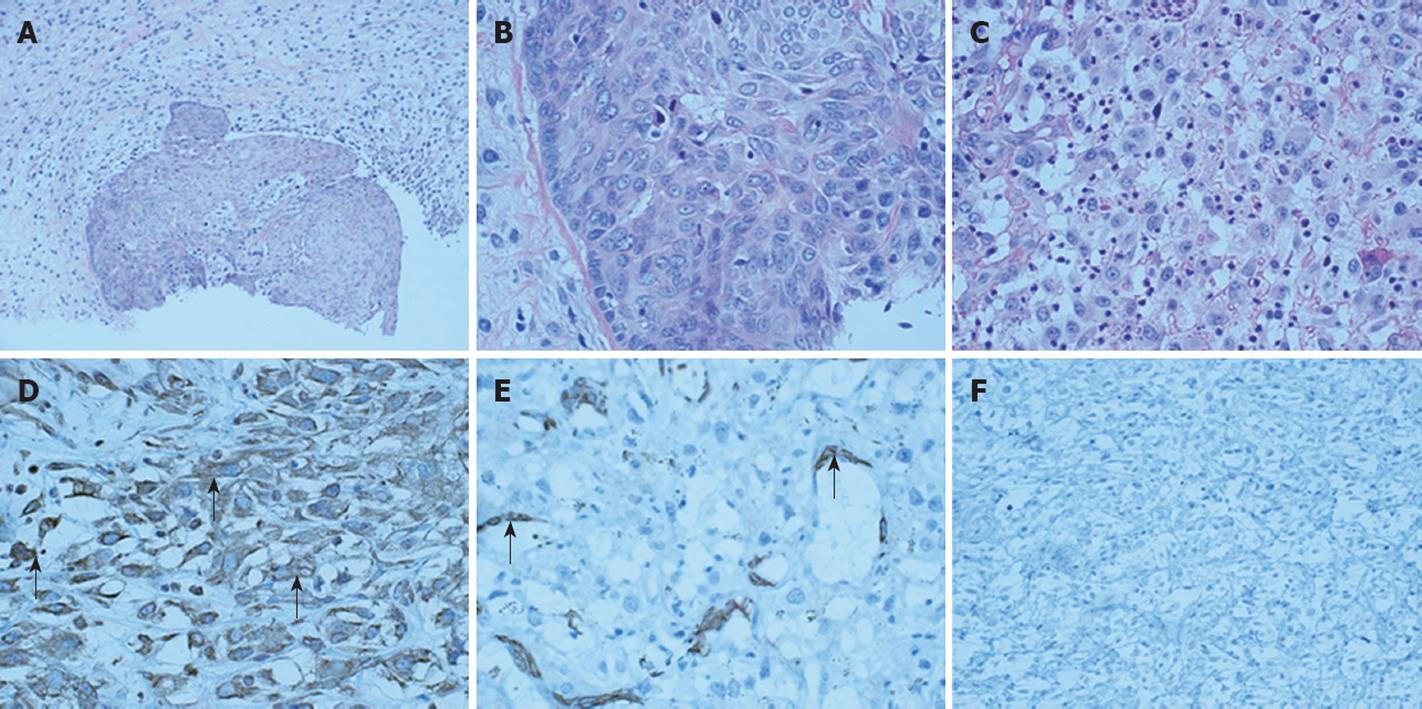
Histology confirmed both carcinomatous and sarcomatous areas in the resected mass (Figure 3A). Large nuclei of polygonal tumor cells with conspicuous nucleoli were observed in the carcinomatous area (Figure 3B) while multiform cells with abundant mitotic figures and bizarre giant cells were observed in the sarcomatous area (Figure 3C). Eosinophilic cytoplasm of tumor cells was found in both carcinomatous and sarcomatous areas with no definite keratinization and intercellular bridges between tumor cells. To further study the histogenesis of sarcoma, we used vimentin, smooth muscle antigen (SMA) and desmin (three well-established immunomarkers for mesenchymal tumor, myofibroblastoma and leiomyoma, respectively) to detect the corresponding antigen expression level in cells of the sarcomatous area. Immunohistology revealed positive vimentin (Figure 3D), negative SMA or desmin (Figure 3E and F), suggesting that the sarcoma has a mesenchymal origin.
Polypectomy was performed. The patient recovered well and was discharged three days later with no relapse 17 mo after operation.
Carcinosarcoma is a rare esophageal tumor showing polypoid configurations, with an incidence of 0.1%-1.5% of all esophageal malignancies[1]. This type of tumor is usually composed of invasive and/or in situ squamous carcinoma cells surrounding the base and surface of exophytic tumor and sarcomatous spindle cells forming the body of polypoid mass[2].
The clinical presentation of esophageal carcinosarcoma is similar to that of squamous cell carcinoma with dysphagia as the most prominent and frequent symptom[1]. The mean age of patients at diagnosis in both histological groups is 70 years with a strong male predominance[1]. The anatomic distribution of both tumor types follows a similar pattern with the middle third of esophagus being the most common location[1]. The bulky nature of esophageal carcinosarcoma is due to its earlier clinical manifestations of dysphagia and obstruction[3], which may also explain why the more favorable prognosis is associated with carcinosarcoma rather than with other esphophageal tumors.
The histogenesis of sarcomatous spindle cell component of esophageal carcinosarcoma is still controversial. Some cases of esophageal carcinosarcoma with osteosarcoma, basaloid squamous carcinoma and rhabdomyosarcoma have been reported[4]. In our case, the esophageal tumor consisted of both carcinomatous and sarcomatous parts, and immunohistochemistry of sarcomatous parts revealed positive vimentin, a mesenchymal tumor immunomarker.
The treatment modality for esophageal carcinosarcoma include esophagectomy, endoscopic resection, chemo-radiotherapy, etc[5–7]. TNM staging is a critical determining factor for treatment decisions. Imaging methods such as EUS, CT and positron emission tomography (PET) play an important role in TNM staging. Compared with CT and PET, EUS is superior for T and N staging of esophageal cancer[89]. Esophagectomy has been traditionally considered the first option for esophageal carcinosarcoma patients[1]. With the advances in micro-invasive techniques, endoscopic procedures, including endoscopic polypectomy, endoscopic mucosal resection and endoscopic submucosal dissection, may represent an alternative to esophagectomy for superficial esophageal carcinosarcoma[6] and are more tolerable, less invasive, less expensive, and most importantly, allow the esophagus to be preserved, compared with traditional esophagectomy.
In our case, endoscopic examination showed a pedunculated polypoid esophageal mass, biopsy indicated the diagnosis of carcinosarcoma, EUS and CT scan showed no evidence of local and distant metastases. Endoscopic polypectomy was subsequently performed. The patient tolerated well to the operation, recovered well, with no relapse during the 17-mo follow-up period, suggesting that endoscopic polypectomy is a promising therapeutic choice for esophageal carcinosarcoma.
In summary, esophageal carcinosarcoma is a rare disease entity. EUS is a useful and accurate method for T and N staging of esophageal carcinosarcoma. Endoscopic therapy is an interesting alternative to surgery for patients with large pedunculated esophageal carcinosarcoma with no involvement of lymph nodes.
| 1. | Ziauddin MF, Rodriguez HE, Quiros ED, Connolly MM, Podbielski FJ. Carcinosarcoma of the esophagus--pattern of recurrence. Dig Surg. 2001;18:216-218. |
| 2. | Kuhajda FP, Sun TT, Mendelsohn G. Polypoid squamous carcinoma of the esophagus. A case report with immunostaining for keratin. Am J Surg Pathol. 1983;7:495-499. |
| 3. | Madan AK, Long AE, Weldon CB, Jaffe BM. Esophageal carcinosarcoma. J Gastrointest Surg. 2001;5:414-417. |
| 4. | Nakakubo Y, Okushiba S, Ohno K, Ito K, Sato K, Morikawa T, Kondo S, Kato H, Ito T, Nagashima K. True carcinosarcoma of the esophagus with osteosarcoma. Hepatogastroenterology. 2001;48:137-139. |
| 5. | Hung JJ, Li AF, Liu JS, Lin YS, Hsu WH. Esophageal carcinosarcoma with basaloid squamous cell carcinoma and osteosarcoma. Ann Thorac Surg. 2008;85:1102-1104. |
| 6. | Pesenti C, Bories E, Danisi C, Monges G, Giovannini M. Endoscopic treatment of esophageal carcinosarcoma: report of a case. Endoscopy. 2004;36:95. |
| 7. | Sanada Y, Hihara J, Yoshida K, Yamaguchi Y. Esophageal carcinosarcoma with intramural metastasis. Dis Esophagus. 2006;19:119-131. |
| 8. | Shimpi RA, George J, Jowell P, Gress FG. Staging of esophageal cancer by EUS: staging accuracy revisited. Gastrointest Endosc. 2007;66:475-482. |
| 9. | van Vliet EP, Heijenbrok-Kal MH, Hunink MG, Kuipers EJ, Siersema PD. Staging investigations for oesophageal cancer: a meta-analysis. Br J Cancer. 2008;98:547-557. |