Published online Jul 21, 2009. doi: 10.3748/wjg.15.3437
Revised: May 19, 2009
Accepted: May 26, 2009
Published online: July 21, 2009
Hepatic hemangiomas need to be treated surgically in cases where they are accompanied with symptoms, have a risk of rupture, or are hardly distinguishable from malignancy. The present authors conducted embolization of the right hepatic artery one day before an operation for a huge hemangioma accompanied with symptoms and confirmed a decrease in its size. The authors performed a right trisegmentectomy through a J-shape incision, using a thoracoabdominal approach, and safely removed a giant hemangioma of 32.0 cm × 26.5 cm × 8.0 cm in size and 2300 g in weight. Even for inexperienced surgeons, a J-shape incision with a thoracoabdominal approach is considered a safe and useful method when right-side hepatectomy is required for a large mass in the right liver.
- Citation: Seo HI, Jo HJ, Sim MS, Kim S. Right trisegmentectomy with thoracoabdominal approach after transarterial embolization for giant hepatic hemangioma. World J Gastroenterol 2009; 15(27): 3437-3439
- URL: https://www.wjgnet.com/1007-9327/full/v15/i27/3437.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3437
Liver hemangiomas are the most common benign tumors occurring in the liver, and are believed to be slowly growing hamartomatous lesions or true vascular neoplasms[1]. They occur more frequently in women than in men, and are believed to be related to levels of female hormones because their size increases during pregnancy[2]. In most cases, the hemangioma is small in size and asymptomatic, and thus follow-up is considered enough, without treatment. However, a giant hemangioma, which is defined as a hemangioma over 4 cm in diameter, can cause symptoms and require intervention. Preoperative diagnosis is possible using ultrasound or helical CT, and the indications for surgical resection are the presence of symptoms, a high risk of rupture, and being indistinguishable from malignancy. Here, we report the successful removal of a giant hemangioma (over 30 cm) from the right side of the liver through a J-shaped incision, using a thoracoabdominal approach, after transarterial embolization (TAE).
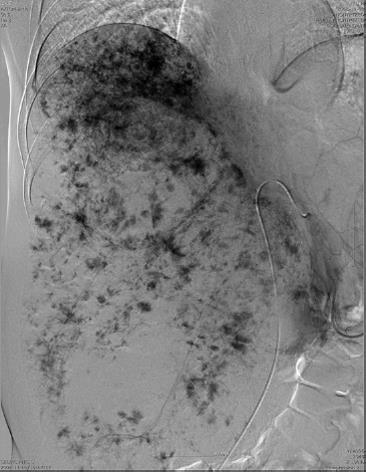
A 41-year-old female patient visited a secondary hospital for abdominal girth (which had not decreased since delivery a year ago), intermittent abdominal pain, and indigestion, as the chief complaints. Ultrasonography, performed during the visit, detected huge hyperechoic lesions, and under the diagnosis of giant hemangioma, she was recommended for surgery and transferred to the present hospital. During a physical examination upon admission, an abdominal mass was palpated from the right upper quadrant to the pelvic cavity. Preoperative serum biochemical studies revealed no abnormal findings, except for an increase of total bilirubin to 2.5 (normal < 1.20 mg/dL). Using helical CT, a non-contrast image showed a homogenous hypodense lesion contrasted with the surrounding liver parenchyma, the arterial image showed peripheral nodular enhancement, and the portal venous image showed progressive centripetal enhancement. These findings indicated a giant hemangioma (Figure 1). The indocyanine green clearance rate at 15 min was 13% (normal range < 15%). TAE of the right hepatic artery was conducted one day before the operation (Figure 2), and thereafter the size decreased by around 5 cm and no more.
Through a J-shaped skin incision using a thoracoabdominal approach, the incision was extended to the 10th intercostal space and the adjacent pleura and diaphragm were opened. Through the incision, the right liver was fully mobilized, and through the hanging method and Glissonian approach, a right trisegmentectomy was safely conducted. The duration of operation was 310 min and intraoperative blood loss was 250 mL. The resected tumor was 32.0 cm × 26.5 cm × 8.0 cm in size and 2300 g in weight. Upon histological examination, it was diagnosed as a cavernous-type hemangioma. The patient’s postoperative course was stable. The chest tube was removed on the fifth day and the patient was discharged on the 10th day. Follow-up has been continued for eight months without any particular findings.
Hemangiomas show specific features in imaging diagnosis, therefore most cases can be diagnosed preoperatively. As a hemangioma increases in size, it can cause congestion, bleeding, thrombosis and infarction (and consequent stomachache), Kasabach-Merritt syndrome, and spontaneous rupture. Out of the mass effect, it might show symptoms such as obstructive jaundice, biliary colic, and gastric outlet obstruction[3]. In our case, the patient complained of only non-specific symptoms such as mild abdominal pain and dyspepsia. Total bilirubin increased slightly but direct bilirubin was normal, which findings did not indicate obstructive jaundice. For the treatment of a giant hemangioma accompanied with symptoms, surgical resection is primarily recommended. Various other treatment methods have been reported but their long-term results have been poor[4]. TAE is suggested as an excellent therapy for easing the symptoms of a giant hemangioma, but recurrence is common because of vascular recanalization. However, there is a report that TAE for a giant hemangioma, performed prior to surgical resection, facilitated the mobilization of the right river by shrinking the hemangioma and, consequently, decreased intraoperative hemorrhage[5]. The authors also performed TAE one day before the operation, and experienced a decrease in the size of hemangioma, as in the previous report. Various complications can occur after embolization and they could postpone the operation and result in the loss of an opportunity for surgery due to vascular recanalization. Accordingly, it is desirable to perform the operation soon after embolization. Thus, the present authors performed the laparotomy within 24 h, and observed the shrinkage of hemangioma during the operation, as in the previous report. This helped minimize bleeding from the hepatic raw surface during the mobilization of the liver.
Preoperative TAE can decrease the risk of bleeding during resection of a hemangioma, but in the liver resection of a 30 cm large giant hemangioma, conventional approaches might cause difficulties. Lai et al[6] reported successful resection of a giant hemangioma using the anterior approach, but they recommended that it should be done by skillful and experienced surgeons because it can cause excessive bleeding from the middle hepatic vein during parenchymal resection. The thoracoabdominal approach is advantageous in that it provides a sufficiently large field of view in a partial hepatectomy or the resection of Couinaud’s Segment 7 and 8, and it has been reported as a useful method for right side hepatectomy by Japanese and European researchers since the 1990s[7]. Compared to conventional approaches, the thoracoabdominal approach is just as safe as a right-sided hepatectomy, but it seems not to be used frequently because the chest has to be opened and an intra-thoracic drainage tube has to be inserted. We think that pulmonary complications are caused by thoracotomy but they are not common in the thoracoabdominal approach, and the problem of pleural effusion can be controlled by the use of an intra-thoracic drainage tube and diuretics. The present authors inserted a postoperative intra-thoracic drainage tube, and did not observe intercostal pain or neurogenic pain caused by the insertion. In addition, the intra-thoracic drainage tube was removed early; therefore it did not affect the postoperative course. The thoracoabdominal approach is obviously a useful method for the safe resection of the right triangular ligament and mobilization of the right liver from the inferior vena cava. Accordingly, when a right-side hepatectomy is performed for a huge mass, such as a giant hemangioma in the right liver, a J-shaped incision using a thoracoabdominal approach is considered a safe and useful method. The addition of “sternotomy” to this incision might be considered of clinical value if the tumor is even larger than in this case.
| 1. | Giavroglou C, Economou H, Ioannidis I. Arterial embolization of giant hepatic hemangiomas. Cardiovasc Intervent Radiol. 2003;26:92-96. |
| 2. | Tuncer I, Arslan H, Harman M. Two giant cavernous hemangioma caused cavernous transformation of the portal vein in a pregnant woman. Turk J Gastroenterol. 2002;13:229-231. |
| 3. | Srivastava DN, Gandhi D, Seith A, Pande GK, Sahni P. Transcatheter arterial embolization in the treatment of symptomatic cavernous hemangiomas of the liver: a prospective study. Abdom Imaging. 2001;26:510-514. |
| 4. | Erdogan D, Busch OR, van Delden OM, Bennink RJ, ten Kate FJ, Gouma DJ, van Gulik TM. Management of liver hemangiomas according to size and symptoms. J Gastroenterol Hepatol. 2007;22:1953-1958. |
| 5. | Vassiou K, Rountas H, Liakou P, Arvanitis D, Fezoulidis I, Tepetes K. Embolization of a giant hepatic hemangioma prior to urgent liver resection. Case report and review of the literature. Cardiovasc Intervent Radiol. 2007;30:800-802. |
| 6. | Lai HJ, Yu JC, Liu YC, Shih ML, Hsieh CB. Anterior approach for a symptomatic giant hepatic haemangioma (>30 centimetre). ANZ J Surg. 2006;76:863-865. |
| 7. | Nanashima A, Sumida Y, Tobinaga S, Shindo H, Shibasaki S, Ide N, Tokunaga T, Tagawa T, Nakamura A, Nagayasu T. Advantages of thoracoabdominal approach by oblique incision for right-side hepatectomy. Hepatogastroenterology. 2007;54:148-151. |