Published online May 28, 2009. doi: 10.3748/wjg.15.2550
Revised: April 24, 2009
Accepted: May 1, 2009
Published online: May 28, 2009
Choledochal cyst is an uncommon disease usually seen in young women and can be divided into five types. We report a 66-year-old woman who was diagnosed with types I and III bile duct cyst simultaneously after surgery, which is a rare type of bile duct cyst.
- Citation: Wang QG, Zhang ST. A rare case of bile duct cyst. World J Gastroenterol 2009; 15(20): 2550-2551
- URL: https://www.wjgnet.com/1007-9327/full/v15/i20/2550.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2550
Choledochal cyst (CDC) is a rare type of bile duct cyst of uncertain origin, which was first described and classified by Todani et al[1] in 1977. The majority of cases reported are young women and children of Asian descent, especially in Japan and Taiwan. The most common symptoms of CDC are abdominal pain, jaundice and abdominal mass. We present a rare case of an elderly female patient with CDC.
A 66-year-old woman was admitted to our hospital because of epigastric pain and dark urine for 10 d. She had some fatty foods before the onset of pain and received antibiotic treatment in a local hospital. She had a 10-year medical history of abdominal pain, which was related to her high-fat diet. She was diagnosed with cholecystitis and quickly recovered after antibiotic treatment.
At physical examination, her blood pressure was 140/90 mmHg, her pulse was 80 beats/min, her body temperature was 37°C, her respiratory rate was 18 breaths/min, and her skin and sclera were yellow-stained. She had tenderness in the epigastric region, and was positive for Murphy’s sign.
Laboratory tests revealed 18.84 × 109/L white blood cells, 89.8% granulocytes, 983 IU/L (0-115 IU/L) blood amylase, 158.4 &mgr;mol/L total bilirubin and 130.23 &mgr;mol/L direct bilirubin.
Abdominal ultrasound showed that the diameter of her common bile duct was 1.3 cm, her intra-hepatic bile duct was dilated, and her gallbladder was enlarged. A primary diagnosis was thus made of acute biliary pancreatitis, obstructive jaundice and acute cholecystitis.
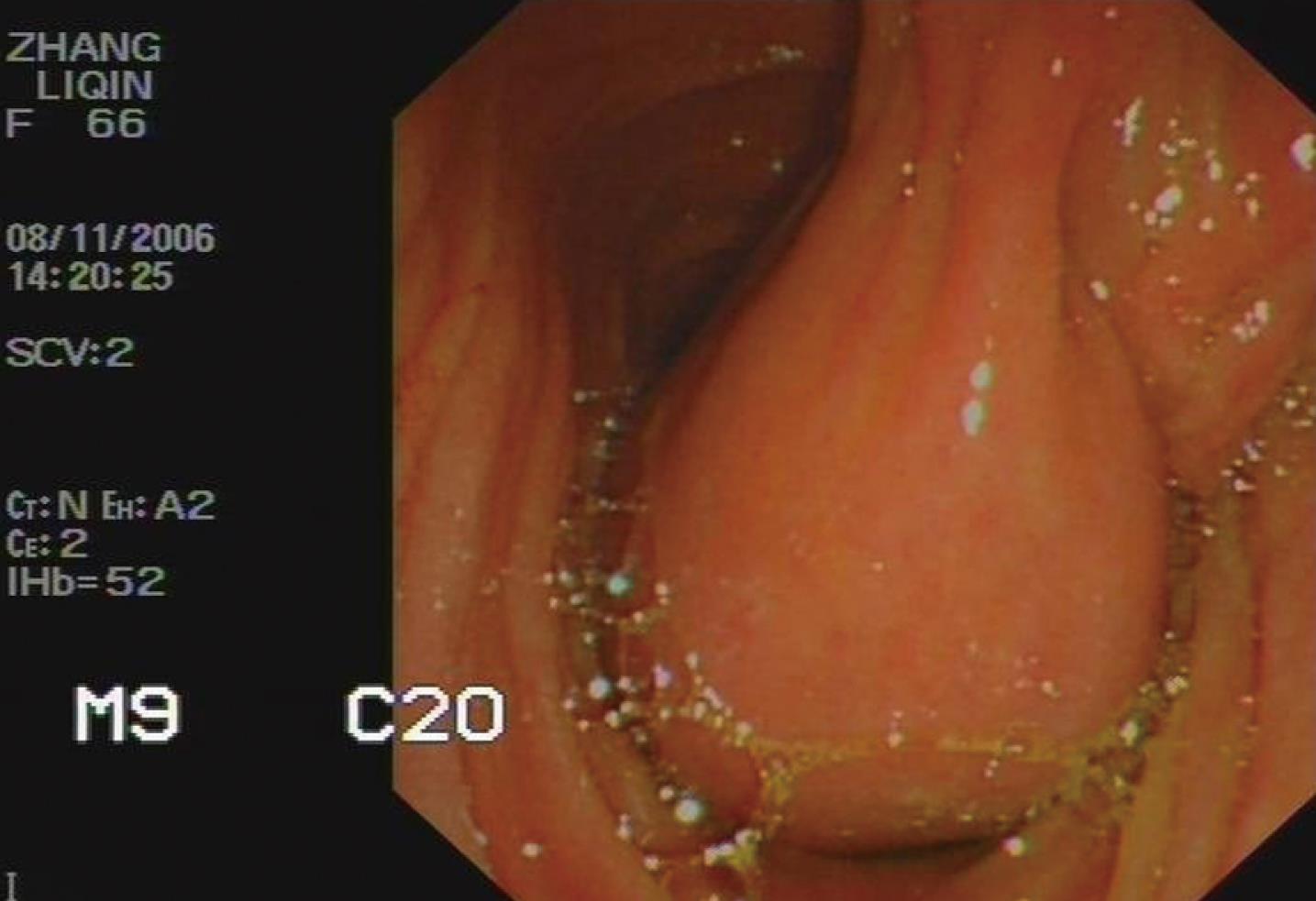
The patient received routine treatment for pancreatitis, and her clinical symptoms and objective signs improved, and her biochemical parameters subsequently returned to their normal levels. However, an abdominal computer tomography (CT) scan suggested that her common bile duct and pancreatic duct were dilated and her pancreatic head was enlarged (Figure 1). Endoscopic examination showed a cystic tumor connected to the papilla in the duodenum (Figure 2). An upper gastrointestinal contrast scan showed a filling defect in the horizontal part of the duodenum with a long pedicel in the intestinal canal (Figure 3).
The patient underwent an operation after consultation. The dilated common bile duct was like a shuttle, and a cyst was observed in the horizontal part of the duodenum connected to the duodenal papilla. Bile leakage was found at excision of the cyst. The cyst was completely removed. Cholecystectomy was performed with reconstruction by Roux-en-Y choledochojejunostomy. The patient recovered quickly and was discharged 20 d after surgery.
CDC, also known as congenital common bile duct cyst (BDC), is a rare type of bile duct cyst of uncertain origin. The majority of cases reported are young women and children of Asian descent. In North America, its incidence is estimated to be 1/150 000[2], but it is increasing in Western adults. The most common symptoms of CDC are abdominal pain, jaundice and abdominal mass.
CDC is graded based on Todani’s classification[1] and can be divided into five types, which are anomalies in the intra- or extra-hepatic bile ducts, or both. CDC can be diagnosed based on percutaneous and endoscopic ultrasound or endoscopic retrograde cholangiopancreatography. Magnetic resonance cholangiography may also contribute to its diagnosis.
Type IV cysts are more commonly observed in adults than in children[3], while type I cysts are more commonly observed in Asian patients[4]. Type III cyst, a cystic-like dilation of the terminal common bile duct, is rare[56]. Our patient had a CDC, consistent with types I and III grading. To the best of our knowledge, this is the first case of bile duct cyst in the English-language literature. Total excision of the diseased bile duct with reconstruction by Roux-en-Y choledochojejunostomy is a preferred treatment modality for CDC[7]. However, its long-term effects on CDC need to be proven in follow-up.
| 1. | Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269. |
| 2. | Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005;189:527-531; discussion 531. |
| 3. | Söreide K, Körner H, Havnen J, Söreide JA. Bile duct cysts in adults. Br J Surg. 2004;91:1538-1548. |
| 4. | Akaraviputh T, Boonnuch W, Watanapa P, Lert-Akayamanee N, Lohsiriwat D. Surgical management of adult choledochal cysts. J Med Assoc Thai. 2005;88:939-943. |
| 5. | Adamek HE, Schilling D, Weitz M, Riemann JF. Choledochocele imaged with magnetic resonance cholangiography. Am J Gastroenterol. 2000;95:1082-1083. |
| 6. | Jordan PH Jr, Goss JA Jr, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg. 2004;187:790-795. |
| 7. | Karrer FM, Hall RJ, Stewart BA, Lilly JR. Congenital biliary tract disease. Surg Clin North Am. 1990;70:1403-1418. |