Published online May 21, 2009. doi: 10.3748/wjg.15.2372
Revised: April 23, 2009
Accepted: April 30, 2009
Published online: May 21, 2009
AIM: To determine the correlation of Adjusted Blood Requirement Index (ABRI) with the 7th day outcome in patients presenting with acute variceal bleeding.
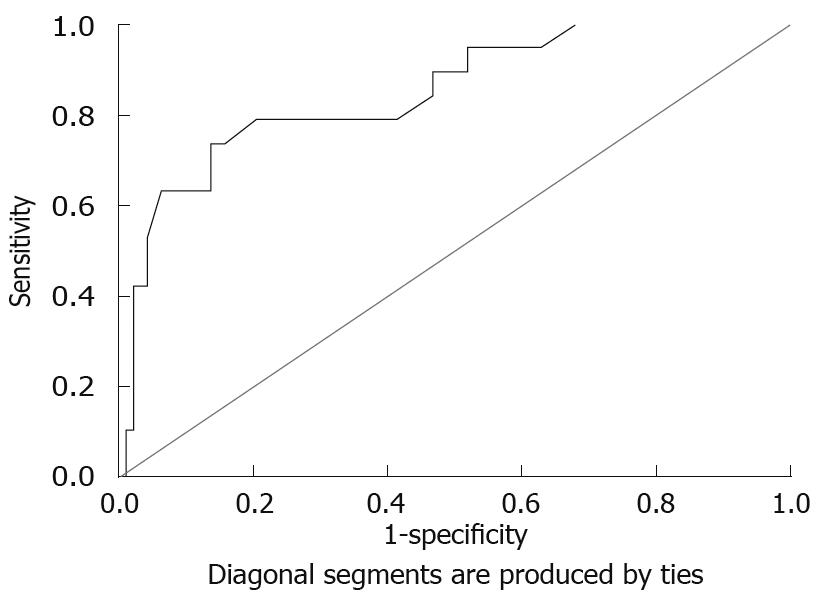
METHODS: All patients presenting with acute variceal hemorrhage (AVH) were included. Patients with previous band ligation, sclerotherapy, gastrointestinal or hepatic malignancies were excluded. Patients were managed as per standard protocol for AVH with terlipressin and band ligation. ABRI scores were calculated using the formula outcome of alive or expired up to the 7th day after treatment. The correlation between ABRI and mortality was estimated and a receiver operative characteristic (ROC) curve was plotted.
RESULTS: A total of 113 patients (76 male; 37 female) were included. On assessment, 18 were in Child’s Pugh Class A, 82 in Class B and 13 were in Class C. The median number of blood units transfused ± inter-quartile range was 3.0 ± 2.0. The median ± inter-quartile range for ABRI was 1.3 ± 1.1. The ROC curve of ABRI for expiry showed a significantly large area of 0.848 (P < 0.0001; 95% CI: 0.75-0.95). A significant correlation of log transformation of ABRI with an outcome of mortality was present (P < 0.0001).
CONCLUSION: ABRI correlates strongly with mortality.
- Citation: Akhtar N, Zuberi BF, Hasan SR, Kumar R, Afsar S. Determination of correlation of Adjusted Blood Requirement Index with outcome in patients presenting with acute variceal bleeding. World J Gastroenterol 2009; 15(19): 2372-2375
- URL: https://www.wjgnet.com/1007-9327/full/v15/i19/2372.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2372
Chronic liver diseases and cirrhosis are now being recognized as an important cause of morbidity and mortality worldwide. Acute variceal hemorrhage (AVH) secondary to cirrhosis is to date the most important cause of mortality in cirrhosis[1]. In Pakistan, hepatitis B and C are the most important causes of cirrhosis[2]. The frequency of varices is very high in cirrhotic patients, nearly 40% of patients with compensated cirrhosis and 60% with decompensated cirrhosis have varices[3]. Due to recent advancements, mortality from AVH has been reduced to 20% from the first variceal bleed[4]. Bleeding from AVH carries a high risk of mortality during the first 5 d, with a gradual decline in risk over the next 4-6 wk[5]. The prediction and evaluation of adequate hemostasis by non-endoscopic methods are desired by treating physicians. Many criteria and definitions to evaluate failure to control and prevent variceal bleeding were developed in the Baveno Consensus Workshops I-III but failed in clinical application due to cumbersome procedures and calculations[6–10]. Further developments in this subject identified an independent factor the “Adjusted Blood Requirement Index (ABRI)” in the Baveno Workshop IV[11]. ABRI was developed to determine adequate control or failure to control variceal hemorrhage. An ABRI value of ≥ 0.75 at any point time was defined as a failure to control variceal bleeding[11].
Failure of AVB control leads to increased mortality. Thus ABRI could be used to assess the risk of mortality. A correlation between ABRI and mortality has not been evaluated in a prospectively designed study. We have reported its correlation with outcome in a retrospective analysis previously[12]. As there are no reports of a prospective evaluation of ABRI and its relation to mortality, there is a need to assess this correlation in our settings.
This study was designed to evaluate the correlation between ABRI and outcome at the 7th day after hospital admission as improved or expired in acute variceal bleeding.
All cirrhotic patients who presented with AVB were included. Informed consent was obtained from all patients. Patients with a history of previous band ligation or sclerotherapy, hepatocellular carcinoma and the presence of peptic ulcer or gastrointestinal (GI) malignancy on endoscopy were excluded. Patients were managed as per standard protocol of acute variceal bleeding[10]. Blood samples were taken for Complete Blood Counts, Prothrombin Time, Liver Function Tests and albumin before the start of therapy. Child’s Pugh Class assessment was carried out. All patients were given terlipressin 2 mg iv initial dose and followed by 1 mg/6 h for 3 d. The number of blood units transfused was noted and endoscopic variceal band ligation (EVBL) was performed within 24 h of admission. Study endpoint was patient outcome (alive or expired at the 7th day after admission). The ABRI value was calculated using the following formula[11]: ABRI = blood units transfused/[(final hematocrit - initial hematocrit) + 0.01]. Child’s Pugh score was calculated using the formula[13] shown in Table 1.
| Parameter | Numerical score | ||
| 1 | 2 | 3 | |
| Ascites | None | Slight | Moderate to severe |
| Encephalopathy | None | Slight to moderate | Moderate to severe |
| Bilirubin (mg/dL) | < 2.0 | 2-3 | > 3.0 |
| Albumin (g/dL) | > 3.5 | 2.8-3.5 | < 2.8 |
| Prothrombin time (prolonged in seconds) | 1-3 s | 4-6 s | > 6.0 |
Sample size was estimated using the following parameters: Level of Significance (α) = 5%; Power of test (1-β) = 80%; Test value of population proportion (Po) = 20% (0.2); Anticipated value of population proportion (Pa) = 30% (0.3); Sample size (n) = 109.
mean ± SD was calculated for age. Median and inter-quartile range were calculated for the number of blood units transfused and ABRI. Frequencies of gender, Child’s Pugh Class and outcome were calculated. ABRI values ≥ 0.75 were recoded into a new variable as uncontrolled while ABRI values < 0.75 were recoded as controlled and their frequency estimated. χ2 test was performed for outcome with ABRI control status and Child’s Pugh Class was carried out with continuity correction and likelihood ratio applied where indicated. A receiver operative characteristic (ROC) curve of ABRI was plotted for expiry. Log transformation of variable ABRI was carried out as it was not normally distributed and then used for Pearson’s Bivariate correlation with outcome. The significance level was set at P≤ 0.05. SPSS version 17.0 was used for statistical analysis.
A total of 113 patients fulfilling the inclusion/exclusion criteria were inducted. These included 76 (67.3%) male (44.3 ± 11.8 years) and 37 (32.7%) female (44.1 ± 9.4 years). Terlipressin was given to 111 patients (98.2%) immediately on admission. EVBL was performed in 105 (92.9%) patients. The assessment on admission showed that 18 (15.9%) were in Child’s Pugh Class A; 82 (72.6%) in Child’s Pugh Class B and 13 (11.5%) were in Child’s Pugh Class C. The median number of blood transfusions given was 3.0 pints and the inter-quartile range was 2.0. The median ABRI was 1.3 with an inter-quartile range of 1.1. The number of patients with ABRI ≥ 0.75 was 86 (76.1%) showing a failure to control variceal bleeding according to ABRI criteria. Outcome at the 7th day after admission showed that 94 (83.2%) patients were alive while 19 (16.8%) patients had expired during this period. Cross tabulation of outcome (alive and expired) with ABRI status [controlled (< 0.75) and uncontrolled (≥ 0.75)] showed that no patients had expired in the ABRI controlled group (Table 2). χ2 test with continuity correction gave a significance value of P = 0.017. A similar cross tabulation with Child’s Pugh Class showed that the highest percentage of patients expired in Child’s Pugh Class C while no patients with Child’s Class A expired (Table 3). χ2 test with the Likelihood Ratio gave significant differences in the frequencies of expiry with Child’s Pugh Class (P < 0.0001). A ROC curve was plotted using expiry as a state variable (Figure 1). The area under the curve was significantly large at 0.848 (P < 0.0001; 95% CI: 0.75-0.95). The sensitivity and specificity of the ABRI cutoff value of 0.75 in our study was 100% and 73.4%, respectively. The correlation of ABRI with outcome was analyzed by Pearson’s Bivariate Correlation test. As the data of ABRI was skewed and not normally distributed its Log10 transformation was used. The results showed a significant correlation between ABRI and expiry with P < 0.0001.
| Outcome | Total | |||
| Alive | Expired | |||
| ABRI groups | Controlled | 27 | 0 | 27 |
| Uncontrolled | 67 | 19 | 86 | |
| Total | 94 | 19 | 113 | |
| Outcome | Total | ||||
| Alive | Expired | ||||
| Child's Pugh Class | Class A | Count | 18 | 0 | 18 |
| % within Child's Pugh Class | 100.0% | 0.0% | 100.0% | ||
| Class B | Count | 71 | 11 | 82 | |
| % within Child's Pugh Class | 86.6% | 13.4% | 100.0% | ||
| Class C | Count | 5 | 8 | 13 | |
| % within Child's Pugh Class | 38.5% | 61.5% | 100.0% | ||
| Total | Count | 94 | 19 | 113 | |
| % within Child's Pugh Class | 83.2% | 16.8% | 100.0% | ||
This study showed a significant correlation between ABRI and the 7th day outcome in patients with AVH. This is a very significant finding as it is important to predict the outcome at an initial stage of management and ABRI suggests whether the variceal hemorrhage has been arrested at any point during management. Our study also established its correlation with mortality. Earlier validation studies of ABRI were retrospective[1112]. The current study is prospective and designed more specifically to assess the correlation of ABRI with mortality which has not been previously studied. The correlation of higher ABRI scores with mortality was significant and this simple to use parameter should be used to assess failure to control bleeding and risk of mortality. The number of units of blood transfused and hematocrit levels, if used alone, are not good criteria to assess variceal bleeding control. We also used pharmacological and endoscopic interventions and the combined effect of these interventions was reflected in the outcome which was also observed in other reports from this region[14]. About 70% of patients rebleeding within 2 years, thus managing the index bleed properly and obliteration of varices can decrease rebleeding[1516].
Many scoring systems have been derived to predict the outcome of upper GI hemorrhage. The Rockall score is one such scoring system for predicting rebleeding and mortality which also showed good correlation[1718]. Limitations of the Rockall score are that it is rather difficult to use with the requirement of more parameters as compared to ABRI and it is not variceal bleeding specific, but designed for both variceal and non-variceal bleeding[1819]. Another popular scoring system, the Child’s Pugh score predicts all cause morbidity and mortality in cirrhotic patients but is not specific for variceal hemorrhage[20].
In conclusion, among the many predictive scoring systems in cirrhotic patients, ABRI is specific for variceal hemorrhage and correlates strongly with mortality and is a good indicator of the failure of variceal hemorrhage control.
In a developing country like Pakistan, hepatitis B and C are the most important causes of cirrhosis. The frequency of varices is very high in cirrhotic patients, nearly 40% of patients with compensated cirrhosis and 60% of patients with decompensated cirrhosis have varices. Mortality from variceal bleeding is still high at 20%. The prediction of mortality risk is difficult and available scores are difficult to calculate and thus do not enjoy wide acceptability and application.
Adjusted Blood Requirement Index (ABRI) is a score which is used to determine the failure to control variceal bleeding. In this study it was correlated with the outcome of mortality.
Many scoring systems are in use to predict the outcome of upper gastrointestinal hemorrhage. The Rockall score is one such scoring system for predicting rebleeding and mortality but it is rather difficult to use. Another scoring system, the Child’s Pugh score predicts all cause morbidity and mortality in cirrhotic patients but is not specific for variceal hemorrhage. The ABRI is a variceal hemorrhage-specific score and is easy to use.
ABRI: A validated tool to determine variceal bleeding control also correlates well with mortality in such patients.
Many scoring systems have been described to predict the prognosis of upper gastrointestinal hemorrhage like Rockall and Child’s Pugh but these have limitations. In practice, it is useful to predict the outcome at admission of patients with acute variceal hemorrhage. This study showed a significant correlation between ABRI and expiry. The methodology is correct. This work deserves to be published to stimulate other teams over the world to perform the same study with a large number of patients.
| 1. | Burroughs AK, Triantos CK, O'Beirne J, Patch D. Predictors of early rebleeding and mortality after acute variceal hemorrhage in patients with cirrhosis. Nat Clin Pract Gastroenterol Hepatol. 2009;6:72-73. |
| 2. | Mashud I, Khan H, Khattak AM. Relative frequency of hepatitis B and C viruses in patients with hepatic cirrhosis at DHQ Teaching Hospital D. I. Khan. J Ayub Med Coll Abbottabad. 2004;16:32-34. |
| 3. | Schepis F, Cammà C, Niceforo D, Magnano A, Pallio S, Cinquegrani M, D'amico G, Pasta L, Craxì A, Saitta A. Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection? Hepatology. 2001;33:333-338. |
| 4. | Turnes J, Garcia-Pagan JC, Abraldes JG, Hernandez-Guerra M, Dell'Era A, Bosch J. Pharmacological reduction of portal pressure and long-term risk of first variceal bleeding in patients with cirrhosis. Am J Gastroenterol. 2006;101:506-512. |
| 5. | Burroughs AK, Mezzanotte G, Phillips A, McCormick PA, McIntyre N. Cirrhotics with variceal hemorrhage: the importance of the time interval between admission and the start of analysis for survival and rebleeding rates. Hepatology. 1989;9:801-807. |
| 6. | North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983-989. |
| 8. | de Franchis R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol. 2000;33:846-852. |
| 9. | de Franchis R. Evaluation and follow-up of patients with cirrhosis and oesophageal varices. J Hepatol. 2003;38:361-363. |
| 10. | de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167-176. |
| 11. | Duvnjak M, Barsić N, Tomasić V, Jukić LV, Lerotić I, Pavić T. Adjusted blood requirement index as indicator of failure to control acute variceal bleeding. Croat Med J. 2006;47:398-403. |
| 12. | Zuberi BF, Riaz MF, Sultan BA, Gobindram P, Farooq A, Qadeer R, Memon AR, Afsar S. Correlation of adjusted blood requirement index with treatment intervention and outcome in patients presenting with acute variceal bleeding. J Dow Uni Health Sci. 2007;1:65-68. |
| 13. | D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231. |
| 14. | Varghese J, Cherian JV, Solomon R, Jayanthi V. Predictors of variceal bleed among patients with liver cirrhosis in the era of sclerotherapy. Singapore Med J. 2008;49:239-242. |
| 15. | Bureau C, Vinel JP. Management of failures of first line treatments. Dig Liver Dis. 2008;40:343-347. |
| 16. | Bosch J, Abraldes JG, Berzigotti A, Garcia-Pagan JC. Portal hypertension and gastrointestinal bleeding. Semin Liver Dis. 2008;28:3-25. |
| 17. | Sarwar S, Dilshad A, Khan AA, Alam A, Butt AK, Tariq S, Ahmad I. Predictive value of Rockall score for rebleeding and mortality in patients with variceal bleeding. J Coll Physicians Surg Pak. 2007;17:253-256. |
| 18. | Sanders DS, Carter MJ, Goodchap RJ, Cross SS, Gleeson DC, Lobo AJ. Prospective validation of the Rockall risk scoring system for upper GI hemorrhage in subgroups of patients with varices and peptic ulcers. Am J Gastroenterol. 2002;97:630-635. |
| 19. | Tham TC, James C, Kelly M. Predicting outcome of acute non-variceal upper gastrointestinal haemorrhage without endoscopy using the clinical Rockall Score. Postgrad Med J. 2006;82:757-759. |
| 20. | Sarwar S, Khan AA, Tarique S. Comparison of MELD, Child Pugh score and Rockall score for predicting rebleeding and in-hospital mortality in patients of variceal bleeding. J Coll Physicians Surg Pak. 2008;18:524-525. |