Published online Apr 28, 2009. doi: 10.3748/wjg.15.2005
Revised: March 26, 2009
Accepted: April 2, 2009
Published online: April 28, 2009
AIM: To determine the efficacy of perioperative parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy.
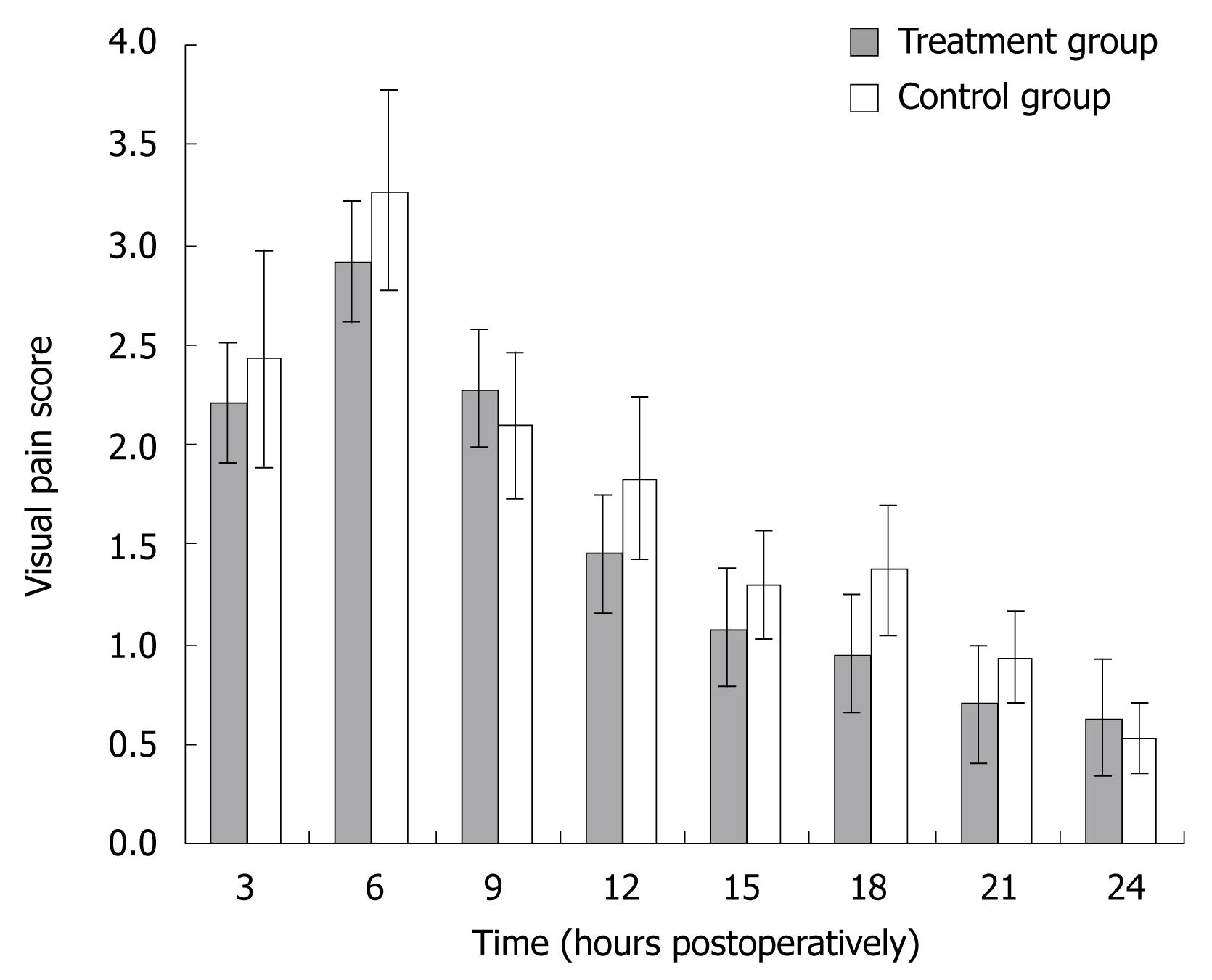
METHODS: A prospective, double-blind, randomized, placebo-controlled study was conducted on 70 patients who underwent elective laparoscopic cholecystectomy under general anesthesia at Siriraj Hospital, Bangkok, from January 2006 to December 2007. Patients were randomized to receive either 20 mg parecoxib infusion 30 min before induction of anesthesia and at 12 h after the first dose (treatment group), or normal saline infusion, in the same schedule, as a placebo (control group). The degree of the postoperative pain was assessed every 3 h in the first 24 h after surgery, and then every 12 h the following day, using a visual analog scale. The consumption of analgesics was also recorded.
RESULTS: There were 40 patients in the treatment group, and 30 patients in the control group. The pain scores at each time point, and analgesic consumption did not differ between the two groups. However, there were fewer patients in the treatment group than placebo group who required opioid infusion within the first 24 h (60% vs 37%, P = 0.053).
CONCLUSION: Perioperative administration of parecoxib provided no significant effect on postoperative pain relief after laparoscopic cholecystectomy. However, preoperative infusion 20 mg parecoxib could significantly reduce the postoperative opioid consumption.
- Citation: Akaraviputh T, Leelouhapong C, Lohsiriwat V, Aroonpruksakul S. Efficacy of perioperative parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy: A prospective, randomized study. World J Gastroenterol 2009; 15(16): 2005-2008
- URL: https://www.wjgnet.com/1007-9327/full/v15/i16/2005.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2005
Preemptive analgesia has become a popular adjunct to conventional postoperative pain control. The concept of preemptive analgesia is based on the hypothesis that the most effective way to eliminate or reduce postoperative pain is to prevent nociceptive input from afferent stimuli to the central nervous system so that central nervous system hyperexcitability does not occur[1]. Clinically, this strategy predicts not only less pain during the initial postoperative period but also a reduced intensity of pain during the days after the procedure[2]. A variety of preoperative or preemptive analgesic regimens have been used such as intravenous administration of opioids or non-steroidal anti-inflammatory drugs (NSAIDs), local anesthetic infiltration, nerve block, and epidural block[3].
Recent research indicates that cyclooxygenase-2 (COX-2) inhibitors, a selective class of NSAIDs, could play an important role in perioperative pain management by reducing the inflammatory response in the periphery, modulating nociceptors, and attenuating central sensitization[4]. The COX-2 inhibitors provide effective pain control, in addition to a lesser degree of platelet dysfunction and gastrointestinal toxicity compared to nonselective NSAIDs. Reuben et al[5] reported that patients receiving perioperative oral COX-2 inhibitors experienced less postoperative pain, required fewer analgesic drugs, and had a greater range of motion after total knee arthroplasty than those receiving placebo.
The injectable COX-2 inhibitor, parecoxib, could play an important role in pain control in the perioperative and immediate postoperative period, especially in those who cannot take an oral analgesic such as a patient about to undergo intraabdominal surgery under general anesthesia. Laparoscopic cholecystectomy is the most common laparoscopic procedure performed in a general surgical unit worldwide, and accounts for about two-thirds of total laparoscopic operations in the authors’ unit. However, the efficacy of perioperative parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy remains controversial[6–11].
The aim of this study was to determine the efficacy of perioperative parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy in a university hospital.
After obtaining approval from our Institutional Ethics Committee, a prospective double-blind, randomized, controlled study was conducted at the Department of Surgery, Faculty of Medicine Siriraj Hospital, Bangkok, Thailand, involving 70 consecutive ASA class I-III patients who underwent elective laparoscopic cholecystectomy from January 2006 to December 2007. All patients gave written informed consent.
Patients were excluded from the study for one of the following reasons: age under 18, hypersensitivity to NSAIDs, or conversion to open cholecystectomy. Patients were randomized into one of two groups by opening a sealed envelope in the operating theater: the treatment group received 20 mg parecoxib infusion 30 min before induction of anesthesia and at 12 h after the first dose; the control group received normal saline infusion as a placebo in a similar time schedule. All patients underwent laparoscopic cholecystectomy under a balanced general anesthetic technique, using fentanyl for premedication and during the intraoperative period. The procedures were performed by an experienced laparoscopist.
The degree of the postoperative pain was assessed every 3 h in the first 24 h after surgery and then every 12 h the following day, using a visual analog scale (0 = no pain, 10 = worst possible pain), by nursing staff who were unaware of the perioperative intervention. A standard postoperative analgesic regimen was administered to all patients. This consisted of intravenous pethidine 1 mg/kg prn for patients with a pain score = 5, every 3 h during the first 24 h after the operation, or until oral analgesics could be taken. The consumption of analgesics was also recorded.
All data were prepared and compiled using SPSS software. Mean and SD were assessed. The Kolmogorov-Smirnov test was used to test for the pattern of data distribution. The student’s unpaired t-test was used to compare data between the two groups when the data were in a normal distribution pattern. The Mann-Whitney U test was used to compare data between the two groups when the data were in a non-normal distribution. P < 0.05 was considered statistically significant.
There were 40 patients in the treatment group, and 30 patients in the control group. The patient’s characteristics, indication for surgery and operative details between the treatment group and control group were well matched (Table 1). The pain scores at each time point did not significantly differ between the two groups (Figure 1). However, there were fewer patients in the treatment group than in the placebo group who required opioid infusion within the first 24 h (60% vs 37%, P = 0.053).
| Treatment group (n = 40) | Control group (n = 30) | P-value | |
| Age (yr) | 57.6 ± 12.7 | 56.2 ± 15.1 | 0.67 |
| Female | 25 (63) | 16 (53) | 0.44 |
| Co-morbid diseases | 24 (60) | 15 (50) | 0.41 |
| Indication for surgery | 0.26 | ||
| Symptomatic gallstone | 28 (70) | 23 (77) | |
| Common bile duct stone | 6 (15) | 6 (20) | |
| Gallstone induced pancreatitis | 6 (15) | 1 (3) | |
| Operative time (min) | 63.7 ± 36.9 | 58.1 ± 31.5 | 0.51 |
Parecoxib, the first injectable COX-2 inhibitor, was introduced into clinical practice in 2001. It was found that preoperative administration of parecoxib was more effective than postoperative administration for postoperative pain relief in patients undergoing elective general surgical procedures such as appendectomy, open cholecystectomy and hernioplasty[12]. Parecoxib can be injected intravenously or intramuscularly with good patient tolerance. The lack of platelet inhibition allows COX-2 inhibitors such as parecoxib to be administered preoperatively. Parecoxib is now increasingly used in ambulatory or day-case surgery because it reduces opioid consumption, improves pain scores, and results in earlier hospital discharge and return to normal function[13].
In the present study, perioperative administration of parecoxib provided no significant effect on postoperative pain relief after laparoscopic cholecystectomy. One possible explanation for our observation is that administration of a total of 40 mg parecoxib is not an optimal dose for perioperative pain control. Puolakka et al[8] found that a single dose of 80 mg parecoxib resulted in the least pain intensity after laparoscopic cholecystectomy compared with 40 mg parecoxib or placebo. However, preoperative infusion of 40 mg parecoxib could significantly reduce the postoperative opioid requirement, and the incidence of opioid-related adverse effects if oral COX-2 inhibitors have been taken in the early postoperative period[9]. There is evidence that the administration of preoperative intravenous parecoxib followed by oral COX-2 inhibitors after laparoscopic cholecystectomy resulted in a shorter length of stay in the postoperative anesthesia care unit, a better quality of postoperative recovery, and a faster return to normal activity, with greater patient satisfaction[10].
It is also possible that pain after laparoscopic cholecystectomy has several components such as incisional and visceral pain; the latter type of pain seems to be more resistant to the analgesic effect of NSAIDs[8]. Therefore, systemic administration of COX-2 inhibitors alone is relatively ineffective. Several investigators have suggested that intraperitoneal administration of local anesthetics could improve postoperative pain control by means of attenuation of the visceral pain. Jabbour-Khoury et al[14] reported that intraperitoneal spray of an aliquot of bupivacaine and NSAIDs, or intraperitoneal spray of local anesthetics following by intravenous NSAIDs resulted in significantly lower abdominal pain scores and incidence of vomiting after laparoscopic cholecystectomy, compared to the non-treatment group. Meanwhile, Elhakim et al[15] revealed that a combination of intraperitoneal lidocaine and tenoxicam provided better analgesia on movement, and faster return of bowel function compared with intraperitoneal lidocaine and intravenous tenoxicam after laparoscopic cholecystectomy[15].
In conclusion, perioperative administration of intravenous parecoxib provided no significant effect on postoperative pain relief after laparoscopic chole-cystectomy. However, preoperative infusion of 20 mg parecoxib could significantly reduce the postoperative opioid consumption.
Preemptive analgesia has become a popular adjunct to conventional postoperative pain control. The concept is based on the hypothesis that the most effective way to reduce postoperative pain is to prevent nociceptive input from afferent stimuli to the central nervous system so that central nervous system hyperexcitability does not occur.
The injectable Cyclooxygenase-2 (COX-2) inhibitor, parecoxib, could play an important role in perioperative pain control and is increasingly used in day-case surgery because it reduces opioid consumption, improves pain scores, and results in earlier discharge and return to normal function.
This study determined the efficacy of perioperative 20 mg parecoxib injection on postoperative pain relief after laparoscopic cholecystectomy.
Perioperative administration of intravenous 20 mg parecoxib provided no significant effect on postoperative pain relief, but could significantly reduce the postoperative opioid consumption after laparoscopic cholecystectomy.
COX-2 inhibitors, a selective class of non-steroidal anti-inflammatory drugs (NSAIDs), could play an important role in perioperative pain management by reducing the inflammatory response in the periphery, modulating nociceptors, and attenuating central sensitization. The COX-2 inhibitors provide effective pain control, in addition to a lesser degree of platelet dysfunction and gastrointestinal toxicity compared to nonselective NSAIDs.
This is a well written manuscript with concise data. The concept of perioperative COX-2 infusion can make GI surgeons pay much attention.
| 1. | Woolf CJ. Generation of acute pain: central mechanisms. Br Med Bull. 1991;47:523-533. |
| 2. | Lohsiriwat V, Lert-akyamanee N, Rushatamukayanunt W. Efficacy of pre-incisional bupivacaine infiltration on postoperative pain relief after appendectomy: prospective double-blind randomized trial. World J Surg. 2004;28:947-950. |
| 3. | Gottschalk A, Smith DS. New concepts in acute pain therapy: preemptive analgesia. Am Fam Physician. 2001;63:1979-1984. |
| 4. | Reuben SS. Update on the role of nonsteroidal anti-inflammatory drugs and coxibs in the management of acute pain. Curr Opin Anaesthesiol. 2007;20:440-450. |
| 5. | Reuben SS, Buvenandran A, Katz B, Kroin JS. A prospective randomized trial on the role of perioperative celecoxib administration for total knee arthroplasty: improving clinical outcomes. Anesth Analg. 2008;106:1258-1264, table of contents. |
| 6. | Tiippana E, Bachmann M, Kalso E, Pere P. Effect of paracetamol and coxib with or without dexamethasone after laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2008;52:673-680. |
| 7. | Papadima A, Lagoudianakis EE, Antonakis PT, Pattas M, Kremastinou F, Katergiannakis V, Manouras A, Georgiou L. Parecoxib vs. lornoxicam in the treatment of postoperative pain after laparoscopic cholecystectomy: a prospective randomized placebo-controlled trial. Eur J Anaesthesiol. 2007;24:154-158. |
| 8. | Puolakka PA, Puura AI, Pirhonen RA, Ranta AU, Autio V, Lindgren L, Rorarius MG. Lack of analgesic effect of parecoxib following laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2006;50:1027-1032. |
| 9. | Gan TJ, Joshi GP, Zhao SZ, Hanna DB, Cheung RY, Chen C. Presurgical intravenous parecoxib sodium and follow-up oral valdecoxib for pain management after laparoscopic cholecystectomy surgery reduces opioid requirements and opioid-related adverse effects. Acta Anaesthesiol Scand. 2004;48:1194-1207. |
| 10. | Gan TJ, Joshi GP, Viscusi E, Cheung RY, Dodge W, Fort JG, Chen C. Preoperative parenteral parecoxib and follow-up oral valdecoxib reduce length of stay and improve quality of patient recovery after laparoscopic cholecystectomy surgery. Anesth Analg. 2004;98:1665-1673, table of contents. |
| 11. | Joshi GP, Viscusi ER, Gan TJ, Minkowitz H, Cippolle M, Schuller R, Cheung RY, Fort JG. Effective treatment of laparoscopic cholecystectomy pain with intravenous followed by oral COX-2 specific inhibitor. Anesth Analg. 2004;98:336-342, table of contents. |
| 12. | Bajaj P, Ballary CC, Dongre NA, Baliga VP, Desai AA. Role of parecoxib in pre-emptive analgesia: comparison of the efficacy and safety of pre- and postoperative parecoxib in patients undergoing general surgery. J Indian Med Assoc. 2004;102:272, 274, 276-278. |
| 13. | Joshi GP. Pain management after ambulatory surgery. Ambulatory Surg. 1999;7:3-12. |
| 14. | Jabbour-Khoury SI, Dabbous AS, Gerges FJ, Azar MS, Ayoub CM, Khoury GS. Intraperitoneal and intravenous routes for pain relief in laparoscopic cholecystectomy. JSLS. 2005;9:316-321. |
| 15. | Elhakim M, Amine H, Kamel S, Saad F. Effects of intraperitoneal lidocaine combined with intravenous or intraperitoneal tenoxicam on pain relief and bowel recovery after laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2000;44:929-933. |