INTRODUCTION
Although lymphomas are malignant neoplasms which are usually confined to the lymph nodes, one fifth of lymphomas present with extranodal localization[1]. The esophagus is an uncommon localization accounting for less than 1% of patients with lymphoma and is usually seen secondary to mediastinal nodes or gastric lymphoma[23]. Isolated primary lymphoma of the esophagus is exceptionally rare, and when seen, is usually the non-Hodgkin’s type[4].
The imaging findings of esophageal lymphoma have shown a diverse spectrum of abnormalities, similar to those of lymphoma elsewhere in the gastrointestinal tract. We present a distinctly rare case of primary diffuse non-Hodgkin’s lymphoma of the esophagus with a unique, to our knowledge, endoscopic ultrasonographic appearance, of a mainly hyperechoic mass.
CASE REPORT
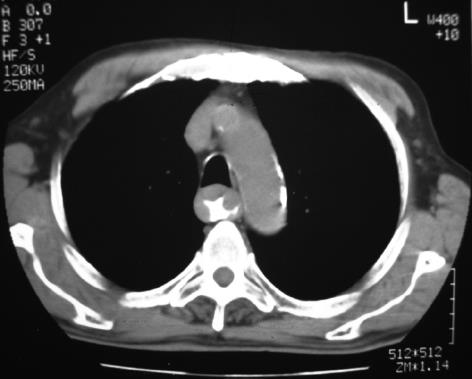
A 77-year old man was admitted because of paroxysmal atrial fibrillation and epigastric pain. His physical examination was normal without clinical evidence of lymph node enlargement or hepatomegaly. Complete blood cell count and routine serum chemistry levels were also normal. A double-contrast barium swallow showed enlargement of the mucosal folds and mild dilatation of the esophageal lumen below the level of the aortic arch (Figure 1); the stomach and duodenum were normal. Chest CT showed extensive thickening of the esophagus wall extending from the middle to the lower portion, without enlargement of mediastinal lymph nodes (Figure 2). CT of the abdomen and pelvis were negative.
Figure 1 Double-contrast barium swallow, showing enlargement of the mucosal folds and mild dilation of the esophageal lumen below the level of the aortic arch.
Figure 2 CT of the chest shows marked thickening of the wall of the esophagus from the aortic arch to the gastrointestinal junction.
There was no enlargement of the mediastinal or hilar lymph nodes.
Endoscopic ultrasonography (EUS) was performed in order to evaluate the esophageal wall thickening. EUS showed a transmural wall thickening along the middle and lower portion of the esophagus with a heterogeneous, mainly hyperechoic mass confined to the sub-mucosal layer, without erosions or ulcers. There was no enlargement of adjacent lymph nodes (Figure 3).
Figure 3 Endoscopic ultrasonography shows a transmural thickening of the esophageal wall and a heterogeneous, mainly hyperechoic, submucosal lesion.
A: Thoracic aorta, B: Water-filled balloon, T: Tumor.
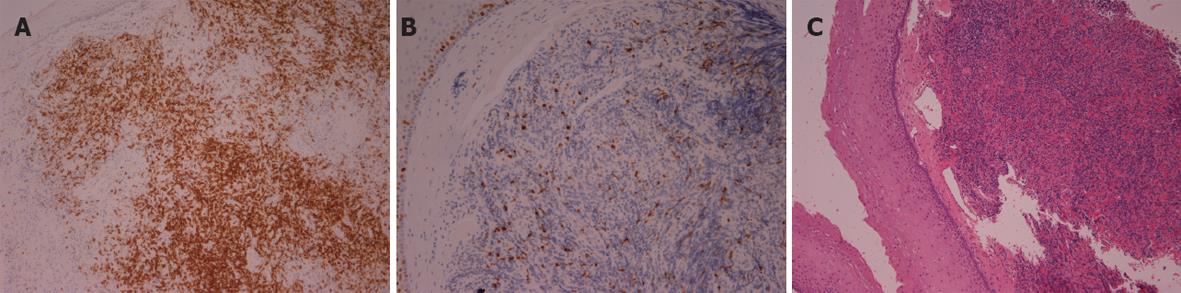
Endoscopy showed excessive rigid folds extending 20-30 cm from the incisors, along the length of the middle and lower esophagus. The stomach and duodenum were normal. Biopsy of the lesion was performed. Histologic examination revealed the presence of a B-cell non-Hodgkin’s lymphoma (Figure 4A-C).
Figure 4 Histologic examination shows the presence of a B-cell non-Hodgkin’s lymphoma (A) infiltration of the esophageal mucosa by lymphoplasmatoid cells; (B) expression of CD20 antigen by lymphoid cells; (C) Ki-67 antigen (index of proliferation) in lymphoma cells.
Bone marrow biopsy specimens showed no evidence of lymphoma; hence, the patient was diagnosed as isolated B-cell lymphoma with diffuse primary involvement of the esophagus.
DISCUSSION
The gastrointestinal tract is the most common extranodal site of non-Hodgkin’s lymphoma accounting for 5%-20% of all cases[156]. Non-Hodgkin’s lymphoma of the esophagus is an extremely uncommon localization of non-Hodgkin’s disease, accounting for less than 1% of patients with lymphoma and occurs more often in the distal esophagus[147]. In a review of the literature, Okerbloom et al[8] found only 4 primary lymphomas of the esophagus in a large series of 1235 cases of non-Hodgkin’s lymphoma, representing an incidence of 0.3%. Freeman et al[1], in another large series found only 3 esophageal lymphomas. Taal et al[9] found 37 cases of esophageal non-Hodgkin’s lymphoma and only two were primary lymphomas. Isolated primary lymphoma of the esophagus without an extra-esophageal location is very rare and only about 20 cases have been described in the literature[1011].
Although lymphoma of the esophagus is often asymptomatic, most patients present with dysphagia. Other less common clinical manifestations of esophageal lymphoma are odynophagia, fever and weight loss[12–15]. Although this disease is extremely rare, it should be considered in the differential diagnosis of patients with acquired immunodeficiency syndrome presenting with dysphagia and weight loss. In our case, the patient complained of epigastric pain. This symptom is nonspecific and should be differentiated from other esophageal or gastric diseases. Our patient had no fever, dysphagia or odynophagia and he was not immunocompromised. Furthermore, our patient fulfilled all Dawson’s criteria to identify primary gastrointestinal lymphoma, such as, no palpable superficial lymphadenopathy, no enlargement of mediastinal or hilar lymph nodes and no splenic involvement[16].
Previously described cases have reported a variety of radiographic appearances for primary esophageal lymphoma. The most common include polypoid masses with or without erosions, stricture with ulceration mimicking esophageal cancer, thickening of the mucosal folds producing a varicoid appearance, narrowed distal segments (achalasia-like appearance), or submucosal nodules[5121718]. Given such a diverse spectrum of radiographic appearance, EUS and CT must be performed and biopsy of the esophageal wall are needed in order to confirm the diagnosis.
In our case double-contrast esophagography showed diffuse mucosal fold thickening, without luminal narrowing, suggesting an intramural, benign lesion. CT revealed the precise extent of the lesion, involving the middle and lower third of the esophagus and the absence of mediastinal lymph nodes. With the clinical application of EUS, great progress has been made in the diagnostic accuracy of structural abnormalities and depth of invasion in various gastrointestinal diseases, including lymphoma[19]. EUS provides more accurate information on the involvement of the wall layers by such an intrinsic process. In our case, all layers were thickened, but not disrupted. Furthermore, a submucosal-located heterogeneous, mainly hyperechoic mass was imaged, which had gradually elevated margins.
In a previous study esophageal lymphoma was described to involve the whole length of the esophagus[20]. However, in this study, EUS showed lymphomatous involvement of the gastrointestinal wall to produce a typical hypo-echogenic transmural thickening. To our knowledge, our case of primary diffuse esophageal lymphoma is the first described in the literature to have a mainly hyperechoic appearance on EUS.
Given the non-specific clinical and radiological appearances, endoscopic biopsy of the lesion was necessary. Endoscopy showed extensive rigid folds without erosions and biopsy was performed. Pathologic evaluation of the endoscopic biopsy showed a B-cell non-Hodgkin’s lymphoma. The treatment of esophageal lymphoma depends on the histological tumor type and its initial location. Because of the extent of the lesion, our patient was treated with chemotherapy and showed clinical improvement. The chemotherapy regimen was a combination of chemotherapeutic agents. The cycle was repeated every 28 d. The patient received six cycles and achieved complete remission (CT scan of thorax and barium swallow did not reveal any residual lesion).
In summary, esophageal lymphomatous involvement should be considered in the differential diagnosis of immunocompetent patients presenting with epigastric pain. A transmural, mainly hyperechoic, diffuse thickening of the esophageal wall in the EUS is another possible appearance of gastrointestinal lymphoma.