CASE REPORT
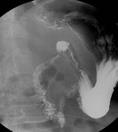
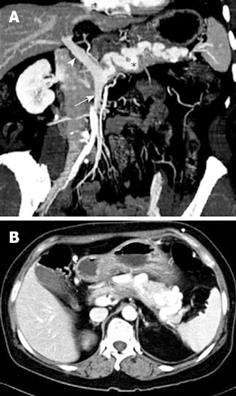
A 61-year-old woman was admitted to our hospital with postprandial epigastric discomfort of 15 d duration. The patient had no significant medical background and family history of disease. The patient had no history of alcohol intake or use of non-steroidal anti-inflammatory medications or tobacco. No abnormal findings were seen after a physical examination and laboratory testing. Upper gastrointestinal endoscopy showed a meandering, dilated, pulsatile vessel in the fundus (Figure 1), and severe stenosis with an active ulcer in the proximal part of the second portion of the duodenum, without active mucosal inflammation seen at other sites of the stomach and bulb. The endoscope (H-260; Olympus Optical, Tokyo, Japan) could not pass beyond the stenosis, and the duodenal second portion was observed by the use of a small-caliber upper endoscope (XP-260; Olympus Optical, Tokyo, Japan). There were no abnormalities in the other area of the second portion of the duodenum. Helicobacter pylori (H pylori) infection was discovered using the rapid urease test. Double contrast gastrography showed acute angulation and an approximately 1-cm long focal stenosis located between the duodenal bulb and second portion of the duodenum (Figure 2). The use of abdominal computed tomography (CT) revealed the absence of the splenic vein as seen on a normal pancreatic and splenic image. The presence of a tortuously engorged, gastroepiploic vein located in the anterior portion of the pancreas was seen (Figure 3). Three-dimensional CT imaging demonstrated the presence of a tortuously dilated left gastric artery and left gastroepiploic artery with non-visualization of the splenic artery (Figure 4). It was concluded that the abnormally dilated vessel in the gastric fundus was the dilated left gastric artery. The patient was treated with 20 mg oral rabeprazole once a day. As the abdominal symptoms of the patient were gradually improving, the patient was discharged from the hospital and has been monitored with the use of regular check-ups. Three months later, follow-up endoscopy showed decreased activity of the duodenal ulcer, but the duodenal stenosis was sustained. The patient has remained asymptomatic for 10 mo.
Figure 1 Upper gastrointestinal endoscopy showing a meandering, dilated, pulsatile vessel in the fundus.
Figure 2 Double contrast view of the duodenum show-ing the acute angulation and stenosis between the duodenal bulb and second portion of the duodenum.
Figure 3 Abdominal CT findings.
A: Oblique sagittal view demonstrates the absence of the splenic vein with confluence of the superior mesenteric vein (arrow) and the presence of the tortuously engorged gastroepiploic vein in the pancreas (asterisk), forming the main portal vein (arrowhead); B: Axial image of the abdomen shows the tortuously engorged gastroepiploic vein in the pancreas.
Figure 4 Three dimensional CT image demonstrates the tortuously dilated left gastric artery (arrow) and the left gastroepiploic artery (arrowhead) with non-visualization of the splenic artery.
DISCUSSION
A splenic artery that originates from the celiac trunk is the most common form according to the classic anatomical description of the splenic artery as described by Michels[3]. Occasionally the splenic artery may arise from the aorta or the superior mesenteric artery, and a double splenic artery may rarely form[4]. However, congenital absence of the splenic artery is an extremely rare occurrence.
The splenic vein follows a course located along the posterior aspect of the pancreas, and the splenic vein is encircled by pancreatic tissue. The hilum of the spleen receives both the short gastric and left gastroepiploic veins. The splenic vein may also receive the coronary and inferior mesenteric vein at the junction with the superior mesenteric vein to form the portal vein[56]. When obstruction to normal flow occurs, venous blood returns to the portal vein by several collateral routes, including the short gastric vein and left gastroepiploic vein[7–9].
Two cases of congenital absence of the splenic artery[12] and only one case of congenital absence of the splenic vein[10] have been reported to date. However, the present case is believed to be the first case of congenital absence of the splenic artery and congenital absence of the splenic vein together. In the two previous cases of congenital absence of the splenic artery, gastrointestinal bleeding from a gastric mucosal lesion secondary to abnormally formed collateral blood flow was determined on arteriograms. Non-visualization of the splenic artery and filling of the intrasplenic branches via the collateral vessels was demonstrated. The two cases were treated with surgery due to repeated hematemesis[12]. The previous case of congenital absence of the splenic vein showed gastric bleeding due to the presence of isolated gastric varices, which was diagnosed by the use of abdominal CT angiography. Marked torturous engorgement of the gastroepiploic vein was seen and the patient was treated with the use of conservative therapy[10]. In the present case, there was a prominent vessel in the fundus without an overlying mucosal abnormality and hemorrhage. The differential diagnosis of the prominent fundal vessel included gastric varices resulting from cirrhosis, pancreatitis, cancer, a splenic vein thrombosis, splenic vein stenosis, a splenic artery aneurysm, surgery, coagulopathy[11–13] and the presence of collateral arterial vessels resulting from congenital absence of the splenic artery or the presence of an occluded splenic artery[14]. This patient had no evidence of cirrhosis, pancreatitis, a pancreatic neoplasm or coagulopathy, but the patient had a prominent, pulsatile vessel suggesting the presence of an artery.
In the present case, CT angiography demonstrated the presence of a dilated left gastric artery and left gastroepiploic artery without visualization of the splenic artery. The splenic vein is located at the posterior portion of the pancreas[56], but in this case, abdominal CT images revealed absence of the splenic vein and the presence of a tortuously engorged, gastroepiploic vein at the anterior portion of the pancreas. Therefore, we diagnosed the case as a congenital absence of the splenic artery and congenital absence of the splenic vein. This patient complained of postprandial epigastric discomfort and the symptoms were caused by duodenal stenosis and acute angulation complicated by the presence of a chronic duodenal ulcer. The cause of the duodenal ulcer and deformity was not clear. This patient had no history of excessive alcohol intake, use of nonsteroidal anti-inflammatory drugs or tobacco use, and had a normal gastrin level, but the patient showed a positive result in a rapid urease test. Undoubtedly, H pylori infection is a major cause of duodenal ulcers[15], but there is the possibility that a duodenal ulcer may have repeatedly developed due to other causes in this patient. We hypothesized that the duodenal ulcer resulted from sustained pressure and ischemia in the duodenal mucosa by the presence of abnormally dilated collateral submucosal vessels secondary to absence of the splenic artery, and inadequate venous drainage through the collateral veins secondary to the absence of the splenic vein, which subsequently caused a duodenal deformity.
In conclusion, absence of the splenic artery and vein accompanied with a duodenal ulcer and deformity is a unique and very rare condition. When gastroduodenal mucosal lesions with prominent pulsatile gastric vessels in the fundus are present, although rare, the congenital absence of the splenic artery with or without the accompanying absence of the splenic vein should be considered for the differential diagnosis.