Published online Feb 28, 2008. doi: 10.3748/wjg.14.1299
Revised: December 12, 2007
Published online: February 28, 2008
Von Hippel-Lindau syndrome (VHL) is a rare autosomal-dominant, inherited familial cancer syndrome. Hemangioblastomas, pheochromocytomas and renal carcinoma are the frequent reported VHL tumors. Neuroendocrine tumors have also been described, mostly in the pancreas and rarely in the biliary trees. We report the second case of bile duct carcinoid in a 31-year-old VHL woman. She underwent right adrenalectomy for a pheochromocytoma in the past. She also had a positive family history of phenotypic expression of VHL syndrome. The patient presented with biliary colic. Endoscopic retrograde cholangio-pancreatography showed intra-luminal bile duct mass. Surgical exploration identified a beige nodular lesion that was a carcinoid tumor on histology. This new association should be clarified by further genetic investigations.
- Citation: Nafidi O, Nguyen BN, Roy A. Carcinoid tumor of the common bile duct: A rare complication of von Hippel-Lindau syndrome. World J Gastroenterol 2008; 14(8): 1299-1301
- URL: https://www.wjgnet.com/1007-9327/full/v14/i8/1299.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1299
Von Hippel-Lindau syndrome (VHL) syndrome is a rare autosomal-dominant, inherited familial cancer syndrome. It is caused by germline alterations in the VHL tumor suppressor gene (3p25)[1]. It has a reported incidence of 1/36 000 births. Twenty percent of patients have no familial history[1]. This germline mutation is associated with a significant variability in the expression of the different tumor associated with the syndrome[1]. The VHL gene codes a protein whose physiological function is the down-regulation of transcription activity of cell growth and cell cycle[2]. VHL gene inactivation may contribute to VHL tumorigenesis[2]. Most frequent VHL tumors include hemangioblastomas of the central nervous system and/or retina, pheochromocytomas (often bilateral), renal carcinoma and pancreatic cystic tumors[1]. Neuroendocrine tumors (NETs) have been reported in VHL patients, mostly of the pancreas[3]. In the bile duct, only one case of NET has been described in VHL patients[4]; we report the third case over the last 16 years.
A 31-year-old woman was routinely screened for von Hippel-Lindau (VHL) syndrome since 1998 after undergoing partial right adrenalectomy for a pheochromocytoma. She had a positive family history of phenotypic expression of VHL syndrome. Her mother was asymptomatic, but her brother was submitted to bilateral adrenalectomy for pheochromocytoma. In 2005, she underwent right adrenalectomy for recurrent pheochromocytoma. A few months later, she also underwent cholecystectomy for symptomatic cholelithiasis.
Six months post cholecystectomy, she presented with biliary colic. Abdominal ultrasound showed normal liver architecture and non dilated bile ducts. Endoscopic retrograde cholangio-pancreatography (ERCP) showed a distal partial filling defect compatible with an intra-luminal bile duct mass (Figure 1). No evidence of recurrence of pheochromocytoma was identified on abdominal CT scan.
The patient was then referred for complementary management. At the time of assessment, she was totally asymptomatic. Her weight was stable. Physical examination was unremarkable. The liver function tests as well as the CA19-9 level were completely normal. Urinary catecholamine level was normal. Endoscopic ultrasound revealed an intra-luminal bile duct polypoid solid mass of 16 mm in diameter. Fine needle aspiration biopsy as well as brush cytology were negative twice.
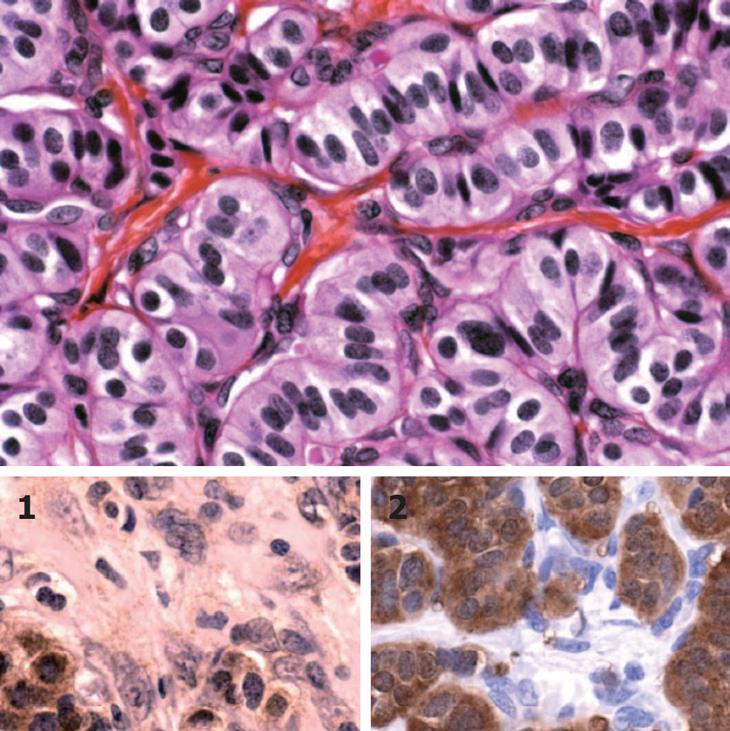
Based on these findings, surgical exploration was considered. At laparotomy, an intra-luminal bile duct lesion was palpated. Bile duct resection, hilar node dissection and hepatico-jejunostomy bile duct reconstruction was performed. The post operative course was uneventful. Macroscopically, the lesion was a beige nodular lesion measuring 1.2 cm × 1 cm. Pathological analysis reported a well-differentiated carcinoid tumour of the common bile duct. It is considered to be a complication of VHL syndrome (Figure 2).
VHL syndrome is a rare autosomal-dominant, inherited familial cancer syndrome. It is caused by germline alterations in the VHL tumor suppressor gene (3p25). It has a reported incidence of 1/36 000 births. Twenty percent of patients have no familial history[1]. This germline mutation is associated with a significant variability in the expression of the different tumors associated with the syndrome[1]. The VHL gene codes a protein whose physiological function is the down-regulation of transcription activity of cell growth and cell cycle[2]. VHL gene inactivation may contribute to VHL tumorigenesis[2]. Most frequent VHL tumors include hemangioblastomas of the central nervous system and/or retina, pheochromocytomas (often bilateral), renal carcinoma and pancreatic cystic tumors[1]. The lifetime risk for developing these tumors is about 70%. It varies according to the nature of the germline mutation[1]. Globally, tumors in VHL syndrome occur at an earlier age than usual and are often multifocal[2]. Neuroendocrine tumors (NETs) have been reported in VHL patients, mostly of the pancreas[3]. NETs are derived embryologically from enterochromaffin cells. Hammel found hormonally non-functional pancreatic NETs in 12.3% of VHL patients[3]. Lubensky associated NETs with VHL syndrome on the basis of an allelic deletion of the VHL gene[5]. NETs in the bile duct and gallbladder have been described in only two patients with VHL syndrome[46]. The rarity of enterochromaffin cells in the biliary tree could explain this observation. Their number increases with intestinal metaplasia of the biliary mucosa consequent to chronic inflammation[7]. In VHL syndrome, the biliary complications are usually associated with pancreatic cystic lesions[8].
Only 49 cases of extrahepatic biliary carcinoid have been reported so far. These tumors occurred mostly in the common bile duct, were non-functional in the majority of cases and affected mostly women in their fifth decade of life. Jaundice was the predominant symptom. Less than one-third of patients present with metastases. Most of them are suitable for curative resection with prolonged disease-free survival[9–11].
Biliary NETs in VHL patients could be an independent tumor type of the syndrome or may only be related by chance. This relationship has been clearly established by genetic investigations for pancreatic NETs. Therefore, the next step in the determination of VHL biliary NET pathogenesis should be the identification of genetic changes at this level.
| 1. | Woodward ER, Maher ER. Von Hippel-Lindau disease and endocrine tumour susceptibility. Endocr Relat Cancer. 2006;13:415-425. |
| 2. | Sano T, Horiguchi H. Von Hippel-Lindau disease. Microsc Res Tech. 2003;60:159-164. |
| 3. | Hammel PR, Vilgrain V, Terris B, Penfornis A, Sauvanet A, Correas JM, Chauveau D, Balian A, Beigelman C, O'Toole D. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d'Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087-1095. |
| 4. | Fellows IW, Leach IH, Smith PG, Toghill PJ, Doran J. Carcinoid tumour of the common bile duct--a novel complication of von Hippel-Lindau syndrome. Gut. 1990;31:728-729. |
| 5. | Lubensky IA, Pack S, Ault D, Vortmeyer AO, Libutti SK, Choyke PL, Walther MM, Linehan WM, Zhuang Z. Multiple neuroendocrine tumors of the pancreas in von Hippel-Lindau disease patients: histopathological and molecular genetic analysis. Am J Pathol. 1998;153:223-231. |
| 6. | Sinkre PA, Murakata L, Rabin L, Hoang MP, Albores-Saavedra J. Clear cell carcinoid tumor of the gallbladder: another distinctive manifestation of von Hippel-Lindau disease. Am J Surg Pathol. 2001;25:1334-1339. |
| 7. | Barron-Rodriguez LP, Manivel JC, Mendez-Sanchez N, Jessurun J. Carcinoid tumor of the common bile duct: evidence for its origin in metaplastic endocrine cells. Am J Gastroenterol. 1991;86:1073-1076. |
| 8. | Deboever G, Dewulf P, Maertens J. Common bile duct obstruction due to pancreatic involvement in the von Hippel-Lindau syndrome. Am J Gastroenterol. 1992;87:1866-1868. |
| 9. | Kim DH, Song MH, Kim DH. Malignant carcinoid tumor of the common bile duct: report of a case. Surg Today. 2006;36:485-489. |
| 10. | Caglikulekci M, Dirlik M, Aydin O, Ozer C, Colak T, Dag A, Canbaz H, Aydin S. Carcinoid tmour of the common bile duct: report of a case and a review of the literature. Acta Chir Belg. 2006;106:112-115. |
| 11. | John BM, Song MH, Park YS, Jo YJ, Kim SH, Lee HH, Kim SK, Jung SH, Kim DH, Kim DH. A case of carcinoid tumor of the common bile duct. Korean J Gastroenterol. 2006;47:320-323. |