Published online Nov 21, 2008. doi: 10.3748/wjg.14.6748
Revised: September 23, 2008
Accepted: September 30, 2008
Published online: November 21, 2008
This case report describes the unusual presentation of a patient who had findings which were initially suggestive of a type IV choledochal cyst. Her liver biopsy demonstrated biliary cirrhosis. She was treated with endoscopic retrograde cholangiopancreatography and biliary stent exchanges over one year. Her cholangiogram one year later demonstrated resolution of the biliary cystic dilation which led to her initial diagnosis, with beading and stricturing of the hepatic ducts consistent with primary sclerosing cholangitis. Liver-associated enzymes and physical findings also improved. A liver biopsy one year later demonstrated a marked improvement in hepatic fibrosis with no evidence of cirrhosis.
- Citation: Goldwire FW, Norris WE, Koff JM, Goodman ZD, Smith MT. An unusual presentation of primary sclerosing cholangitis. World J Gastroenterol 2008; 14(43): 6748-6749
- URL: https://www.wjgnet.com/1007-9327/full/v14/i43/6748.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6748
Primary sclerosing cholangitis (PSC) is a chronic progressive disorder characterized by diffuse intrahepatic and extrahepatic bile duct inflammation, stricturing, and fibrosis; progressing to cirrhosis and hepatic failure. PSC occurs more commonly in men, is frequently associated with ulcerative colitis (73%) and is a risk factor for cholangiocarcinoma[1]. We report an unusual case of PSC, which was initially diagnosed as a choledochal cyst.
A 30-year-old female presented with a 6-mo history of yellow eyes, dark urine and clay-colored stools. Two years earlier, evaluation at another facility revealed elevated liver-associated enzymes (LAEs). She was diagnosed with Caroli’s disease on the basis of non-invasive imaging.
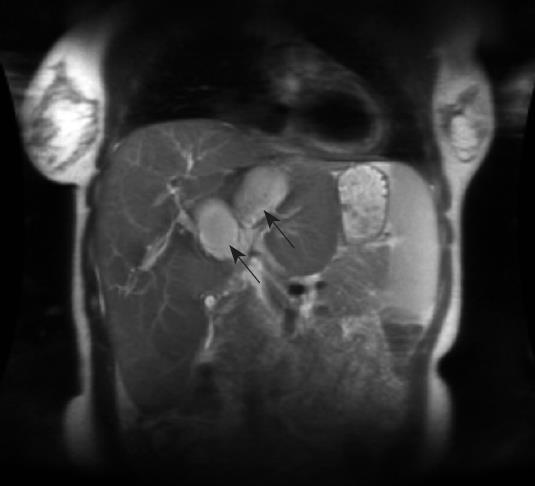
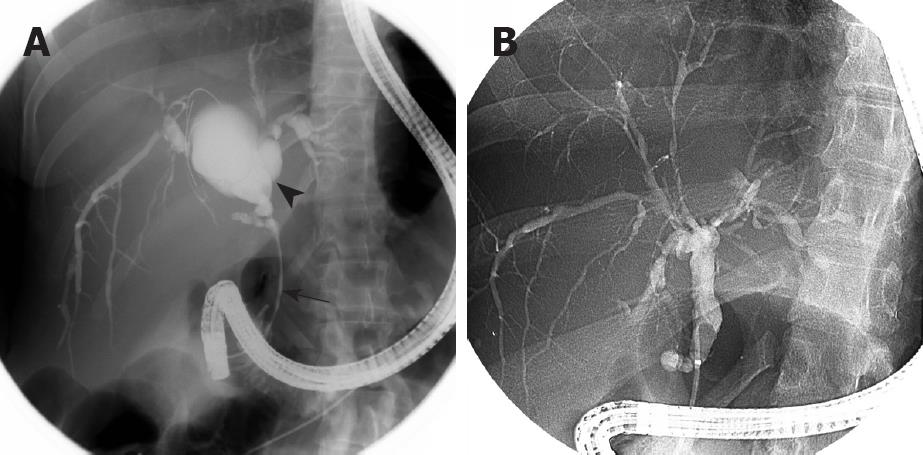
On our evaluation, scleral icterus and hepatos-plenomegaly were found on physical examination. Her total bilirubin was 20.9 mg/dL (normal 0.2-1.3 mg/dL), direct bilirubin 18.0 mg/dL (0.0-0.4 mg/dL), alkaline phosphatase (ALK) 957 U/L (38-126 U/L), aspartate aminotransferase (AST) 104 U/L (14-50 U/L) and alanine aminotransferase (ALT) 56 U/L (9-52 U/L). Abdominal computed tomography (CT) scanning showed dilation of the biliary ducts involving the right and left lobes (Figure 1). The common bile duct appeared normal. Magnetic resonance cholangiopancreatography (MRCP) showed intrahepatic biliary ductal dilation including the right and left hepatic ducts consistent with choledochal cysts (Figure 2). Endoscopic retrograde cholangiopancreatography (ERCP) revealed cystic dilation of the left and right hepatic ducts and a common duct stricture (Figure 3A). The intrahepatic ducts appeared irregular and had focal areas of dilation. A 10 FR 7 cm biliary stent was placed with good drainage of bile and contrast. Cytologic specimens of the stricture were benign.
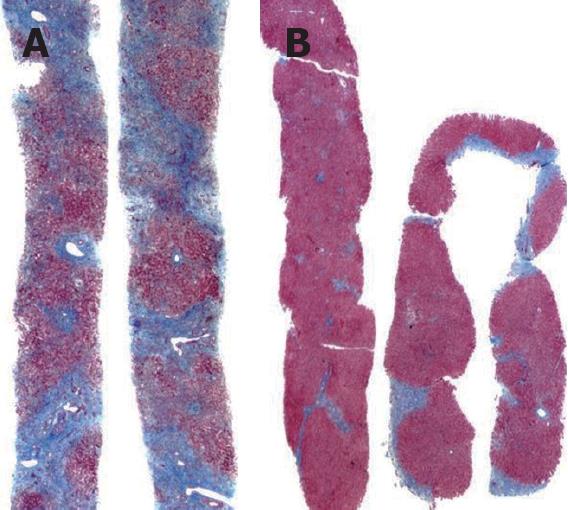
Liver biopsy demonstrated biliary-type cirrhosis with cholestasis and bile ductular proliferation. Based upon cholangiography and histological findings, we diagnosed type IVB choledochal cyst and biliary cirrhosis. Biliary stent exchanges were performed over the following year with gradual improvement in LAEs. ERCP performed one year after our evaluation revealed diffusely irregular intrahepatic and extrahepatic bile ducts and total resolution of the cystic dilation and common duct stricture (Figure 3B). Her bilirubin was 0.6 mg/dL, ALK 220 U/L, ALT 36 U/L, and AST 38 U/L. Liver biopsy showed only focal cholestasis, mild portal inflammation, and irregular portal and bridging fibrosis. There was a marked improvement in the degree of fibrosis when compared to her initial liver biopsy (Figure 4), and there was no longer evidence of cirrhosis.
We present a patient with an unusual presentation of PSC, with imaging and histological findings which initially led to a diagnosis of a type IVB choledochal cyst and biliary cirrhosis. The diagnosis of PSC was made after her subsequent cholangiogram demonstrated pruning and stenosis of the intrahepatic ducts, with resolution of the cystic biliary dilation. PSC is a slow progressive disease, which ultimately leads to hepatic failure. Cholangiography is the gold standard for the diagnosis of PSC[2]. Orthotopic liver transplantation may be used for patients with PSC with end stage liver disease[3].
Hepatic fibrosis is triggered by recurrent liver injury, which results in the activation of perivascular stellate cells and other myofibroblasts[4]. This process may be reversible in its early stages, and there are reports of regression of liver fibrosis after biliary drainage in patients with chronic pancreatitis[5]. However, it is unusual to have significant improvement in hepatic fibrosis after years of liver injury. In our patient, pre- and post-treatment liver biopsies documented a regression in hepatic fibrosis. It is our belief that the histologic improvement in our patient can be attributed to relief of mechanical obstruction by stenting and drainage of the common bile duct. We acknowledge the possibility of liver sampling error; however, the overall improvement in her clinical picture supports a cause and effect relationship between biliary stricture therapy and regression of fibrosis.
Peer reviewer: Pietro Invernizzi, PhD, Division of Internal Medicine, Department of Medicine, Surgery, Dentistry, San Paolo School of Medicine, University of Milan, Via Di Rudinfi 8, Milan 20142, Italy
S- Editor Li DL L- Editor Kerr C E- Editor Lin YP
| 1. | Matsuda T, Matsutani T, Tsuchiya Y, Okihama Y, Egami K, Yoshioka M, Maeda S, Onda M. A clinical evaluation of lymphangioma of the large intestine: a case presentation of lymphangioma of the descending colon and a review of 279 Japanese cases. J Nippon Med Sch. 2001;68:262-265. |
| 2. | Kim J, Han D, Hong CH, Lee HL, Kim JP, Sohn JH, Hahm JS. Colonic lymphangiomatosis associated with protein-losing enteropathy. Dig Dis Sci. 2005;50:1747-1753. |
| 3. | Watanabe T, Kato K, Sugitani M, Hasunuma O, Sawada T, Hoshino N, Kaneda N, Kawamura F, Arakawa Y, Hirota T. A case of multiple lymphangiomas of the colon suggesting colonic lymphangiomatosis. Gastrointest Endosc. 2000;52:781-784. |
| 4. | Wildhaber BE, Chardot C, Coultre CL, Genin B. Total Laparoscopic Excision of Retroperitoneal Cystic Lymphangioma. J Laparoendosc Adv Surg Tech A. 2006;16:530-533. |
| 5. | Sato K, Maekawa T, Yabuki K, Tomita N, Eguchi M, Matsumoto M, Sugiyama N. Cystic lymphangiomas of the colon. J Gastroenterol. 1999;34:520-524. |