Published online Nov 7, 2008. doi: 10.3748/wjg.14.6425
Revised: October 21, 2008
Accepted: October 28, 2008
Published online: November 7, 2008
We report a rare case of acute pulmonary and cerebral complication after transarterial chemoembolization (TACE) for inoperable hepatocellular carcinoma. The case involved a large tumor and hepatic vein invasion. Nonspecific pulmonary and cerebral symptoms such as acute dyspnoea and transient consciousness loss developed in the patient, a 49-year-old woman, following the TACE due to pulmonary and cerebral oil embolism. The chest and brain conditions of this patient improved after some supportive therapies and nursing interventions. She also subsequently completed the other three procedures of TACE.
- Citation: Zhao H, Wang HQ, Fan QQ, Chen XX, Lou JY. Rare pulmonary and cerebral complications after transarterial chemoembolization for hepatocellular carcinoma: A case report. World J Gastroenterol 2008; 14(41): 6425-6427
- URL: https://www.wjgnet.com/1007-9327/full/v14/i41/6425.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6425
Hepatocellular carcinoma (HCC) is one of the leading causes of cancer-related death in China where the majority of HCC patients have underlying hepatic B virus (HBV) infection and cirrhosis, and most cases are unresectable due to late stage and multifocali. Transarterial chemoembolization (TACE) is one of the most common treatment modalities as a palliative and preoperative method for patients with advanced HCC, which can improve the resection rate of HCC and prolong the survival time of patients. HCC has a tendency to invade the portal and hepatic veins, which may result in formation of hepatic arterio-venous shunts. Some rare complications such as remote ectopic embolism can be caused by this kind of abnormal shunts. In this paper, we report a rare pulmonary and cerebral complication of HCC, which is probably associated with hepatic vein invasion.
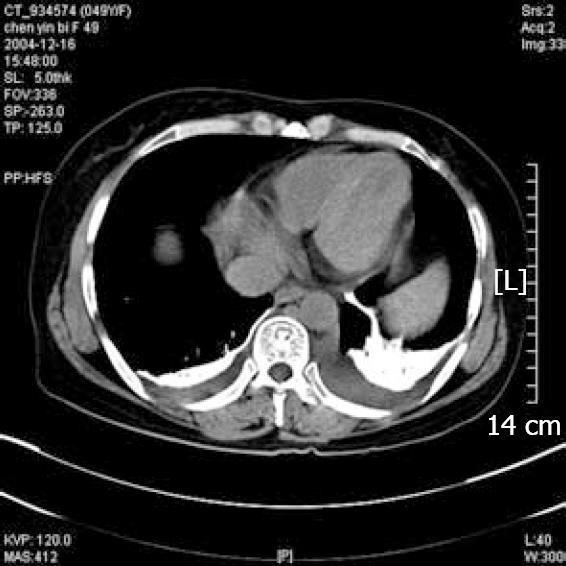
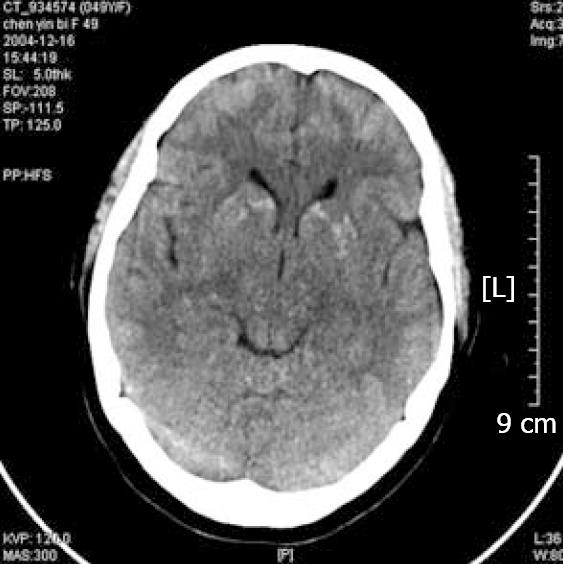
A 49-year-old woman was admitted to the Department of Radiology of the Second Affiliated Hospital of Zhejiang University in October 2004 with right upper quadrant pain and weight loss. She was a hepatitis B virus carrier. Her α-fetoprotein level was 1185.3 ng/mL. Ultrasonography and computed tomography (CT) revealed a 10-cm mass in the posterior segments of the right liver lobe. A 1.5-cm mass was also found in the left lateral segment. These clinical signs indicated that the patient had inoperable HCC and Child-Pugh class A cirrhosis. TACE was offered to the patient. Angiogram demonstrated no obvious hepatic arterio-venous shunt, but multiple smaller masses in both lobes of the liver. An emulsion of oxaliplatin, pirarubicin, hydroxycamptothecin and lipiodol were prepared, 35 mL and 3 mL of the mixture were administered intra-arterially to the right and left hepatic artery, respectively. The patient experienced right upper quadrant pain after TACE and had an uneventful recovery. One month later, a second TACE procedure was performed via the right hepatic artery and 40 mL of the mixture was administered. On the next day, she experienced sudden acute dyspnoea and the peripheral oxygen saturation decreased to 90%. The chest X-ray showed some increased reticular shadows in the left lung, especially in the lower zones, and a chest CT scan revealed multiple iodized oil-like high-density materials in parenchyma of the lung (Figure 1). After 10 mg dexamethasone i.v. and other supportive therapies were administered, the respiratory symptom was attenuated. Two days later, the patient suffered from a serious headache and transient consciousness loss, accompanying nausea and vomiting followed by confusion, lower extremity weakness. Non-contrast enhanced CT scanning showed multiple disseminated hyper-intense lesions in the brain, consistent with deposition of iodized oil (Figure 2). One week later, her respiratory and neurologic symptoms disappeared completely, and she was discharged. The patient also consequently completed the other three TACE procedures, during which no similar symptoms occurred.
TACE has various severe complications, including acute hepatic failure, intrahepatic biloma, pseudoaneurysm formation, and ectopic infarction, which occur in less than 1% of patients. Pulmonary embolism is a rare complication of TACE. Xia et al[1] reported a total of 2012 TACE procedures in 1348 patients, but pulmonary embolism occurred only in case. Sporadic cases of cerebral embolism after TACE have also been reported[2-5]. No reports are available on pulmonary embolism accompanying cerebral embolism after TACE. We encountered a rare pulmonary and cerebral complication of HCC, which was probably associated with hepatic vein invasion. The patient had nonspecific respiratory and neurological symptoms, including cough, dyspnoea, headache, transient loss of consciousness, confusion, and weak extremities. Chest X-ray and CT scanning showed some positive findings, indicating deposition of iodized oil, and the diagnosis of pulmonary and cerebral embolism was confirmed clinically.
The underlying mechanisms of pulmonary and cerebral embolism after TACE are still obscure. Hepatic arterio-venous shunt, which is associated with hepatic vein invasion of HCC, may be the reasonable explanation for pulmonary embolism. Vascular abnormalities, referred to as pulmonary arterio-venous shunt, can be found in patients with advanced liver disease[6]. If patients have pulmonary embolism after TACE, the oil emboli may also pass through the pulmonary arterio-venous shunt and enter the systemic circulation. In this case, the patient suffered from pulmonary and cerebral embolism subsequently. Thus, we hypothesize that iodized oil passed through the hepatic arterio-venous shunt, and then traveled to the cerebral artery through intrapulmonary arterio-venous shunt There are also some other hypotheses including intracardiac right-to-left shunt (e.g. patent foramen ovale) and right-to-left shunt via the arteriovenous anastomosis between the right inferior phrenic artery (IPA) and the intrapulmonary vasculature. However, there is no evidence to support the theory of intracardiac or IPA shunts in this patient.
Although pulmonary and cerebral embolism or infarctions are rare complications of TACE in patients with HCC, we should be aware of this kind of situations when we observe complications of TACE. When angiogram shows any hepatic arterio-venous shunts, we should decrease the dose of lipiodol during the procedure and pay great attentions to the respiratory and neurological symptoms post-operatively, which may be caused by ectopic embolism. The manifestations caused by lipiodol are different from those caused by thrombus, because lipiodol diffuses to peripheral blood vessels while thrombus usually obstructs the main branch of arteries.
A thorough patient assessment should be performed by nurses before the procedure. Some risk factors including a large size of HCC, hepatic vein invasion of HCC, live cirrhosis, congenital cardiovascular disease, and chronic pulmonary disease should be noticed before the procedure. If the patients have risk factors for pulmonary and cerebral complications of TACE, nurses should give a reassessment, extra education, psychological support.
In addition to post-embolization syndrome (PES), with its symptoms manifested as fever, pain, nausea, and vomiting, there are also some severe or rare complications of TACE, including acute hepatic failure, intrahepatic biloma, pseudoaneurysm formation, ectopic infarction, etc. Nurses should keep in mind that a small number of patients after TACE will suffer from some severe or rare complications. Our patient developed a dry cough and dyspnea in the first day after TACE, followed by severe headache, nausea, vomiting, weak extremities and lost consciousness transiently in the third day. Nurses immediately provided nursing interventions such as semi-reclining position, inhaling oxygen, administration of steroids and dehydrating agents, and intensive monitoring of the patient’s vital signs. She had a good recovery and was discharged. If some symptoms such as cough, chest pain, chest distress, headache, nausea, and vomiting occur in patients after TACE, nurses should make physical examination and notify the physician to exclude pulmonary and cerebral complications.
When the diagnosis of pulmonary embolism is confirmed, some nursing actions must be taken immediately. Nurses should keep the patient’s airway open, and have oxygen inhaled to maintain the patient’s basic respiratory function. Vital signs, blood oxygen saturation, mental status, and some laboratory values must be monitored and documented. If the patient has signs of respiratory failure, intensive care and mechanical ventilation must be provided promptly. Tiny lipiodol particles usually diffuse and stay in the peripheral bronchus and alveoli, which can damage gas exchange and cause special inflammations. Steroids, bronchodiators and prophylactic antibiotics should also be given.
The aim of nursing care during an acute phase of cerebral embolism after TACE is to minimize cerebral damage. Nurses should frequently observe the level of consciousness, pupil size and reaction to light, patient’s response to commands, movement and strength, patient’s vital signs, etc. To reduce the intracranial pressure, some nursing routines must be given such as keeping the head of bed above 30º, restriction of fluids, oxygen inhaling and administration of steroids and dehydrating agents. Sedatives and tranquilizers, which can depress the respiratory center and obscure neurological observations, should not be given except for some specific situations such as epileptic seizure attack.
In summary, even though pulmonary embolism and cerebral embolism are rare complications of TACE, we should be aware of these rare complications in patients with high risk factors and reduce the dose of iodized oil or stop the procedure.
Peer reviewer: Dr. Bandar Abdulmohsen Al Knawy, Division of Gastroenterology & Hepatology, Department of Medicine, King Abdulaziz Medical City, Riyadh 22490, Saudi Arabia
S- Editor Zhong XY L- Editor Wang XL E- Editor Yin DH
| 1. | Xia J, Ren Z, Ye S, Sharma D, Lin Z, Gan Y, Chen Y, Ge N, Ma Z, Wu Z. Study of severe and rare complications of transarterial chemoembolization (TACE) for liver cancer. Eur J Radiol. 2006;59:407-412. |
| 2. | Yoo KM, Yoo BG, Kim KS, Lee SU, Han BH. Cerebral lipiodol embolism during transcatheter arterial chemoembolization. Neurology. 2004;63:181-183. |
| 3. | Wu RH, Tzeng WS, Chang CM. Iodized oil embolization to brain following transcatheter arterial embolization of liver. J Gastroenterol Hepatol. 2005;20:1465-1467. |
| 4. | Takao H, Makita K, Doi I, Watanabe T. Cerebral lipiodol embolism after transcatheter arterial chemoembolization of hepatocellular carcinoma. J Comput Assist Tomogr. 2005;29:680-682. |
| 5. | Matsumoto K, Nojiri J, Takase Y, Egashira Y, Azama S, Kato A, Kitahara K, Miyazaki K, Kudo S. Cerebral lipiodol embolism: a complication of transcatheter arterial chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2007;30:512-514. |
| 6. | Lange PA, Stoller JK. The hepatopulmonary syndrome. Ann Intern Med. 1995;122:521-529. |