CASE REPORT
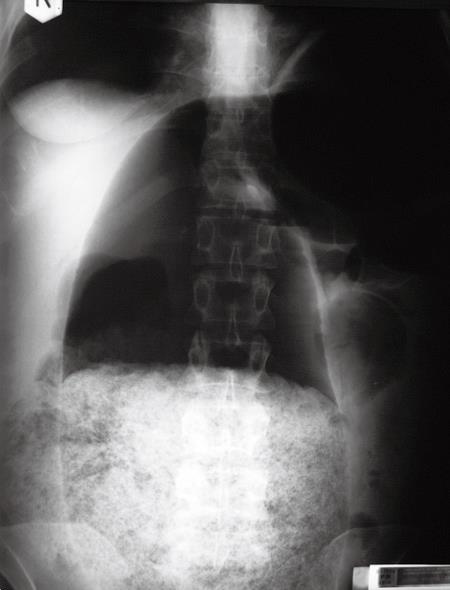
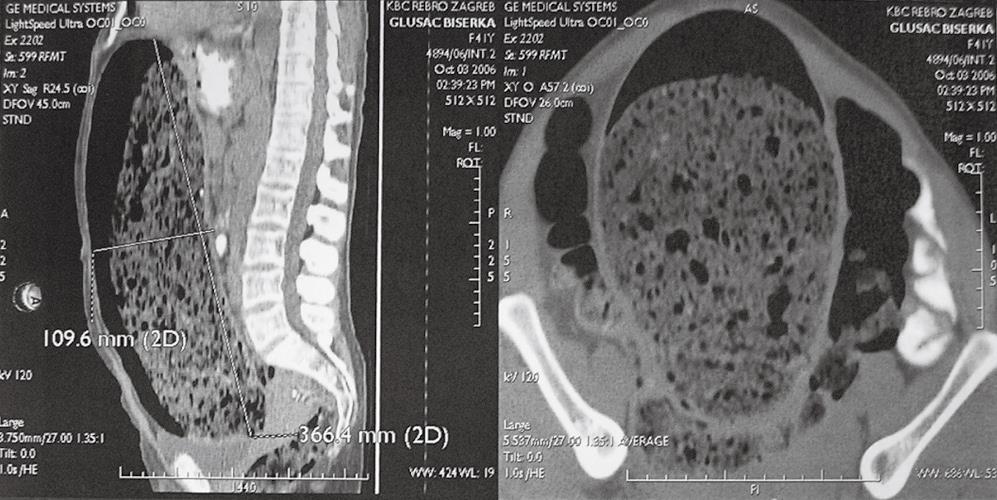
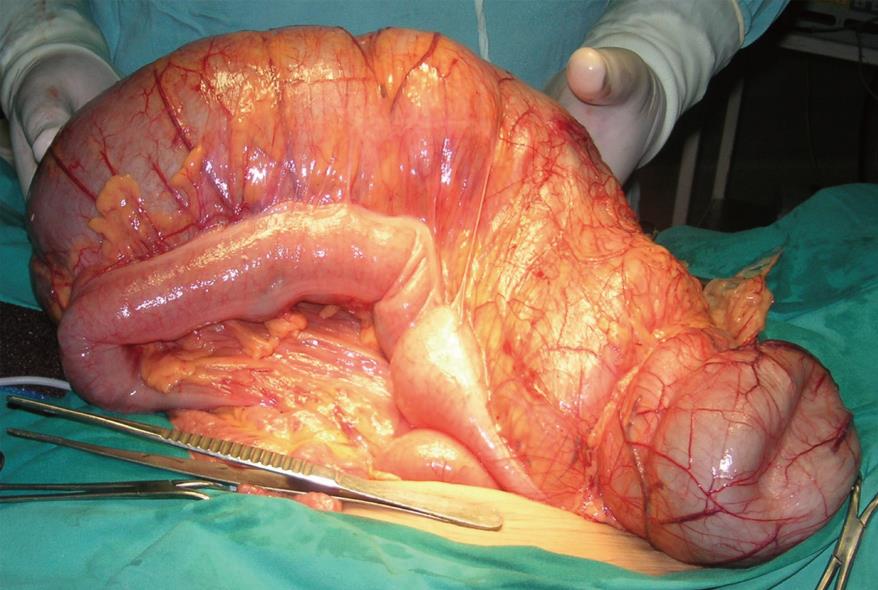
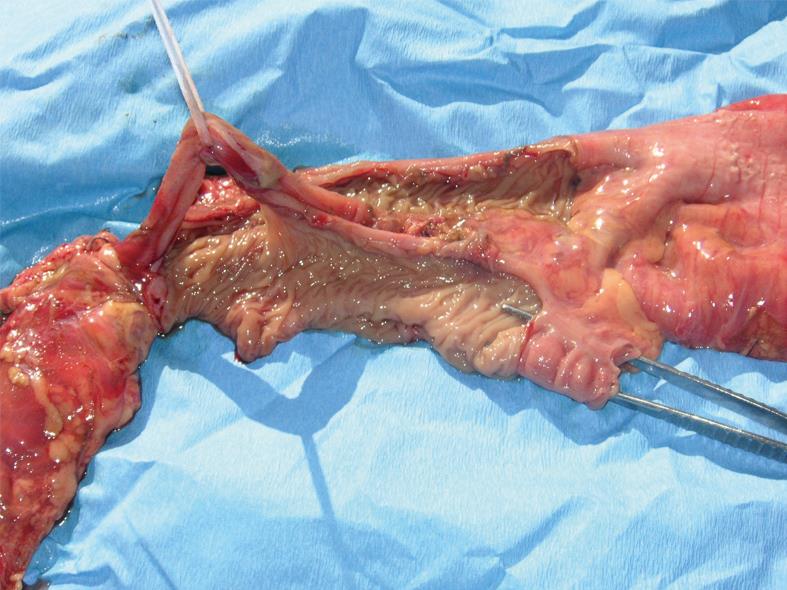
A 42-year-old woman was admitted to the division of gastroenterology with symptoms of significant abdominal distension and chronic constipation. The patient had a medical history of chronic constipation from the early childhood which was not striking until 1991 when, during gestation, significant gaseous bowel distention was found. Complete diagnostic workup was made to find the cause of the constipation but all findings were normal. The constipation was attributed to hypothyroidism caused by long standing Hashimoto thyroiditis treated with thyroid hormone replacement. In 1999 the symptoms progressed and again complete diagnostic workup was made. The diagnosis was elongated colon (dolichocolon). During these eight years the patient used cathartics, different types of tea and manual stool evacuation. There were periods of seven days without stool evacuation. The patient got used to irregular bowel habits and after 1999 did not go to regular controls. Finally in the last few months in 2006 she noticed significant abdominal distension and consulted the gastroenterologist. Complete laboratory findings, including proteins, albumins, IgA, IgM, IgG, T3, T4 and TSH were normal. ECG and esophagogastroduodenoscopy were normal. Plain X-rays of the abdomen showed an extremely dilated intestinal loop, presumably colon with fecal masses without signs of obstruction (Figure 1). Colonoscopy revealed normal mucosa with few biopsies showing chronic nonspecific colitis. Anal manometry showed: lower mean resting pressure (50 mmHg), normal squeeze pressure (200 mmHg), normal rectal sensation, rectal compliance and recto-anal inhibitory reflex. The conclusion was that there were no elements for Hirschsprung’s disease and that the internal anal sphincter showed slight hypofunction. Multislice CT with peroral contrast showed an enormously dilated intestinal loop from diaphragm to pelvis, measuring 36 cm in length with the diameter of 11 cm occupying the complete abdominal cavity in the midline (Figure 2). The stomach, rectum and genitourinary tract were normal. There were no enlarged lymph nodes. The patient was transferred to the department of surgery and the exploratory laparotomy revealed colonic duplication of the transversal colon with no other intra-abdominal pathology (Figure 3). Duplication was separated by a sharp dissection from the left half of the transversal colon but shared common wall with the right half of the transversal colon. The duplication ended blindly at the splenic flexure and had an opening that communicated with the normal colon at the hepatic flexure (Figure 4). Finally, right hemicolectomy was performed. The patient functioned well postoperatively and a few months after the procedure did not have any stool evacuation difficulties as encountered preoperatively.
Figure 1 Plain X-ray of the abdomen showing a dilated intestinal loop occupying more than half of the abdominal cavity filled with fecal masses.
Figure 2 Abdominal CT showing a dilated intestine from the diaphargm to the pelvis, measuring 36 cm in length with a diameter of 11 cm dislocating normal intestine laterally.
Figure 3 Operative view of normal transversal colon and the distended tubular colonic duplication.
Figure 4 Surgical specimen showing part of the normal ascending and transversal colon together with a tubular duplication with all layers of the colonic wall dividing these structures.
DISCUSSION
Gastrointestinal duplications are rare congenital anomalies which in 80% of cases are detected prenatally or in the first two years of life, although they can remain undetected until older age[6]. The clinical picture varies according to their location, size, and other factors such as the presence of ectopic mucosa within the duplication, communication with adjacent bowel, or inflammation. The duplications are classified according to their location (ileum 30%, ileocecal valve 30%, duodenum 10%, stomach 8%, jejunum 8%, colon 7%, rectum 5%), shape: cystic (≥ 80%) or tubular[7]. The most common clinical manifestations are abdominal pain and intestinal obstruction. Rarely, such duplications present with signs of acute abdomen or acute bleeding[8]. Pyloric and duodenal duplications can mimic hypertrophic pyloric stenosis or a choledochal cyst[5910]. An ovarian cyst should be considered in female patients, and adolescent patients can sometimes have a presumptive diagnosis of Crohn’s disease. Ultrasound is the imaging modality of choice for the evaluation of an abdominal mass in the neonate. Approximately 30% of the intestinal duplications are diagnosed prenatally[11]. Additional imaging procedures are often required: barium enema, CT scan, radionuclide scan (HIDA scan for choledochal cyst and pertechnetate scan for Meckel’s diverticulum). However, gastric, duodenal, and rectal duplications can lead to a diagnostic dilemma.
Chronic constipation as a presenting symptom of intestinal duplication in adults present specific diagnostic problems because of a wide variety of etiologic factors. The cause of constipation is usually multifactorial. Secondary constipation could be caused by low fibre diet, anal fissures, thrombosed hemorrhoids, strictures, and tumors, hypercalcemia, hypokalemia, hypothyroidism, diabetes mellitus, pregnancy, stroke, Hirschsprung disease, Parkinson's disease, multiple sclerosis, spinal cord lesion, Chagas disease, familial dysautonomia, scleroderma, amyloidosis, mixed connective-tissue disease and use of different drugs. Functional constipation could be caused by repressed defecatory urge, irritable bowel syndrome, idiopathic megacolon or megarectum, idiopathic slow transit constipation, chronic intestinal obstruction, anismus, solitary rectal ulcer, intussusception, descending perineum, rectocele or ineffective straining.
Intestinal duplications often require urgent surgical intervention. Secretion of ectopic gastric mucosa causes ulceration of the intestinal mucosa, which can lead to massive bleeding or bowel perforation[12]. Gastric mucosa was found in 50.8% of cystic duplications and was present in all locations, including the colon and rectum with somewhat lower frequency of 33%[3].
Colorectal duplications represent 13% of all duplications[3]. Tubular duplications of the colon, may appear in a double-barreled or Y-shaped form[1314]. These congenital anomalies have a double muscular layer and epithelium similar to the rest of the colon[1315]. The clinical signs include constipation, vomiting, volvulus, perforation, and, most commonly, intestinal obstruction owing to the blind end of the duplication compressing the normal bowel[131416]. If there are no other associated malformations, tubular duplications of the colon are often not discovered until there is surgical treatment for the complications.
Most authors recommend that once the diagnosis is made, an elective surgical procedure should be performed to avoid complications and to perform the procedure in an optimal state of the patient, but few think that only symptomatic duplications should be surgically treated. The recommended surgical procedure is excision of the duplication. Intestinal duplications are located on the mesenteric side adjacent to normal bowel. Some duplications and the adjacent normal bowel share part of the muscular coat and the intestinal straight arteries. Thus, resection of both normal and duplicated bowels with intestinal anastomosis is a usual surgical treatment[17]. Sometimes it is possible to resect them without compromising the adjacent bowel vascularization. Although there have been some malignant changes reported in adults[18], colorectal duplications are in themselves benign lesions. For this reason, surgical excision should not be radical but should involve complete resection of the duplication along with the relevant part of the colon[4]. Although rare, colorectal duplications are one possible cause of chronic constipation and, when discovered, should be treated surgically before complications arise. According to previous studies, surgical resection should extend at least 2 cm from the opening of the duplication; because substantial fibrotic changes near the opening of the duplication have been found[413]. Prognosis is good because of localized disease and the benign nature of the disease[4].