Published online Jan 28, 2008. doi: 10.3748/wjg.14.638
Revised: September 29, 2007
Published online: January 28, 2008
Intussusception is rare in adults. We describe a 47-year-old man with ileal schwannoma that led to ileocolic intussusception. Abdominal ultrasonography, abdominal CT scan and barium enema confirmed an ileal tumor. Colonoscopy revealed a peduncular submucosal tumor (SMT) 75 mm long with an ulcerated apex at the ascending colon. The provisional diagnosis was a gastrointestinal stromal tumor of the terminal ileum. Ileocecal resection was carried out and the tumor was histologically diagnosed as schwannoma. Abdominal pain resolved postoperatively. This case reminds us that ileal schwannoma should be included in the differential diagnosis of intussusception caused by an SMT in the intestine.
- Citation: Hirasaki S, Kanzaki H, Fujita K, Suzuki S, Kobayashi K, Suzuki H, Saeki H. Ileal schwannoma developing into ileocolic intussusception. World J Gastroenterol 2008; 14(4): 638-640
- URL: https://www.wjgnet.com/1007-9327/full/v14/i4/638.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.638
Ileal schwannoma is an extremely rare disease, even among small intestine tumors. In Japan, there have been no more than eight cases reported in the literature[12]. There have been no reports describing adult cases of ileocolic intussusception due to ileal schwannoma. Here, we describe a rare case of ileal schwannoma that led to ileocolic intussusception.
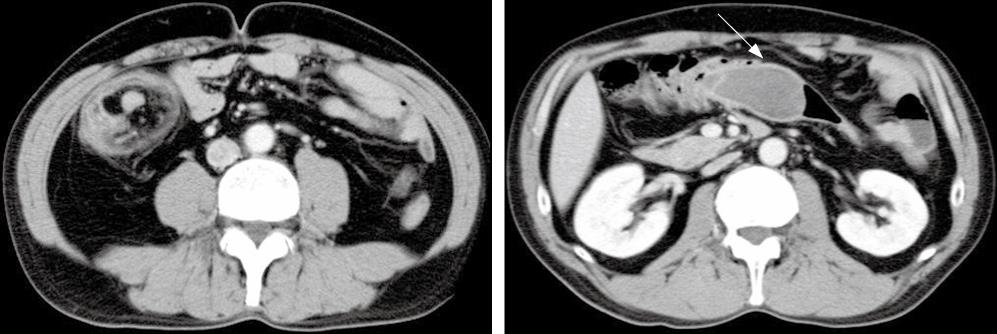
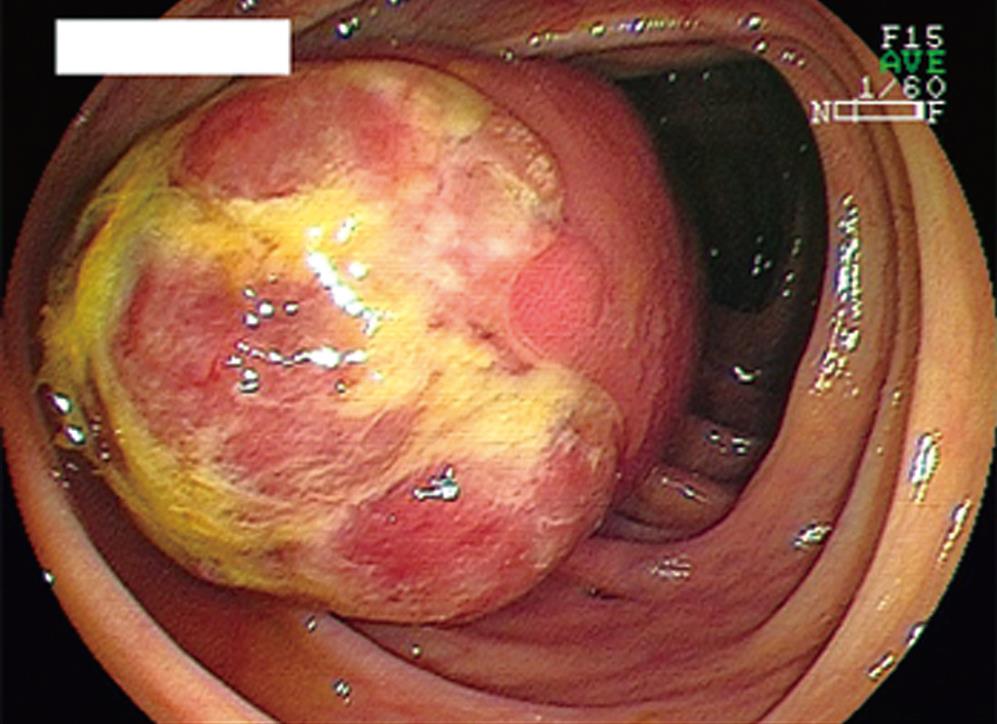
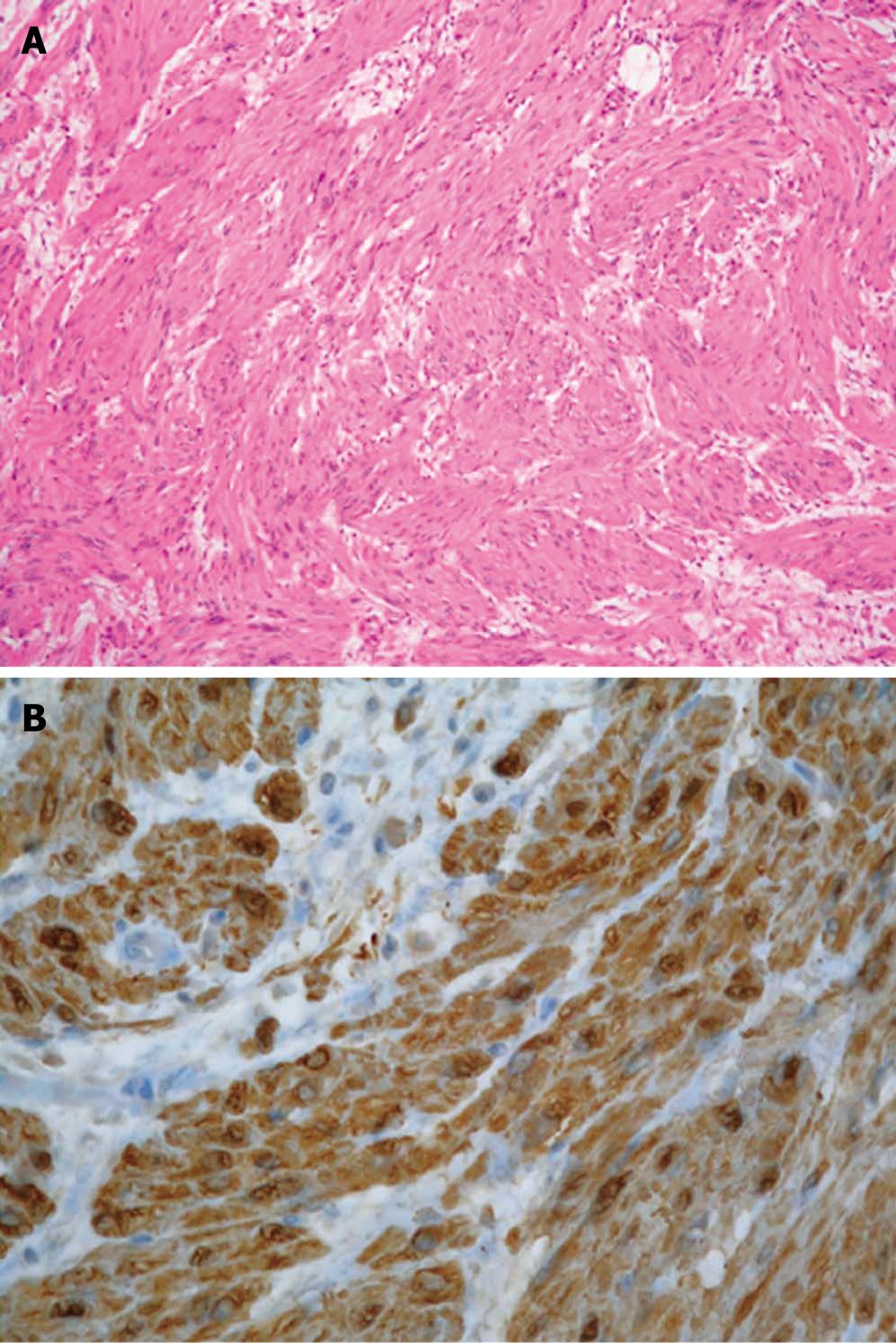
The patient was a 47-year-old Japanese man. He was admitted to our hospital complaining of intermittent abdominal pain of several months’ duration that was increasing in both magnitude and frequency. He had not had previous abdominal surgery and had been in good health. No specific family history was identified. His body temperature was 36.4°C, blood pressure was 126/78 mmHg, and radial pulse rate was 66 beats/min and regular. He had neither anemia nor jaundice. A neurological examination revealed no abnormal findings and there was no lymphadenopathy. Routine hematological examination and biochemical tests were within normal limits. Abdominal CT scan revealed a large, comparatively well-defined mass in the colon and intussusception (Figure 1). An air contrast barium enema also showed a large elevated mass 7 cm × 4 cm in diameter with a smooth surface in the ascending colon, which suggested a submucosal tumor (SMT). Colonoscopy revealed a large SMT with an ulcerated apex in the ascending colon (Figure 2). The SMT was peduncular, covered with normal ileal mucosa, and prolapsed from the ileocecal valve to the ascending colon. A biopsy specimen obtained from the lesion showed spindle-like cells. Based on these findings, the patient was diagnosed with intussusception due to intestinal SMT, which suggested a gastrointestinal stromal tumor (GIST). The patient underwent an urgent laparotomy (ileocecal resection) because of the increased frequency of abdominal pain after colonoscopy. The resected tumor, 75 mm × 43 mm × 34 mm in size, was covered with normal ileal mucosa (Figure 3). Histological examination of the resected specimen revealed interlaced bundles of large, bizarre, spindle-like tumor cells without mitotic figures (Figure 4). No fission images were evident. Immunohistological findings were negative for CD34 and α-smooth muscle actin (SMA), and positive for S-100 protein (Figure 4). Based on the above findings, this tumor was diagnosed as ileal schwannoma. The postoperative course was uneventful. No additional therapy was performed. As a result of this treatment, the patient’s abdominal pain resolved postoperatively.
Schwannomas are tumors derived from Schwann cells. These tumors are prone to occur peripherally in the head and limbs, and cause radiating pain or sensory paralysis[3]. Although schwannoma rarely occurs on the trunk, even a small one in the brain or spinal cord causes serious neurological symptoms. Manifestations in the gastrointestinal tract are rare, but when they do occur, the incidence is high in the stomach; a schwannoma originating in the small intestine is rare[4]. According to Nozu et al[1] and Nagai et al[2], a review of the Japanese literature has revealed only eight cases of ileal schwannoma in Japan up to 2003. Common symptoms are abdominal pain and melena[1256]; intestinal obstruction or intussusception is rare. In contrast with intussusception in children, nearly all adult cases have primary causes such as a polyp, an SMT or a malignant tumor that needs to be resected[7]. In the present case, the tumor prolapsed to the ascending colon due to intussusception.
The preoperative diagnosis of schwannoma appears to be difficult. According to Nagai et al[2], none of the reported cases of ileal schwannoma in Japan had been correctly diagnosed preoperatively. For preoperative diagnosis, CT, ultrasound (US), MRI, and angiography are useful for locating the tumor site. CT depicts the tumor growing outside the wall, and displays a high shadow effect[8]. Imaging of the small intestine shows findings suggestive of an SMT, such as extramural pressure or tumor shadow loss[9]. Angiography of the superior mesenteric artery shows hypervascular tumor vessels[10]. In the present case, CT, US and barium enema images were compatible with schwannoma. However, the diagnosis could not be confirmed despite endoscopy. Because of the increased frequency of abdominal pain after colonoscopy, the patient underwent urgent laparotomy; thus, angiography and MRI were not performed in the present case.
This disease is treated in principle by surgical resection. It is not possible to differentiate benign from malignant schwannoma confidently with imaging alone. Ileal benign schwannoma is not fatal and patients remain asymptomatic in their daily lives, except for bowel intussusception or obstruction; therefore, it is likely that there are patients with latent small bowel schwannoma, which may be incidentally discovered in the future as a result of advances in diagnostic imaging, such as improved CT and MRI.
In conclusion, we have reported a very rare case of ileal schwannoma that led to ileocolic intussusception. Thus, it is necessary to be aware that an ileal schwannoma may cause ileocolic intussusception and should be suspected in a patient with chronic atypical abdominal pain.
| 1. | Nozu T, Takahashi A, Asakawa H, Uehara A, Kohogo Y, Suzuki T. Malignant intestinal schwannoma: a case report and a review of the literature in Japan. Intern Med. 1995;34:1101-1105. |
| 2. | Nagai T, Fujiyoshi K, Takahashi K. Ileal schwannoma in which blood loss scintigraphy was useful for diagnosis. Intern Med. 2003;42:1178-1182. |
| 3. | Sivak MV Jr, Sullivan BH Jr, Farmer RG. Neurogenic tumors of the small intestine. Review of the literature and report of a case with endoscopic removed. Gastroenterology. 1975;68:374-380. |
| 4. | Sarlomo-Rikala M, Miettinen M. Gastric schwannoma-A clinico pathological analysis of six cases. Histopathology. 1995;27:355-360. |
| 5. | Gallo SH, Sagatelian MA. Benign schwannoma of the small intestine: an unusual cause of gastrointestinal bleeding. J Ky Med Assoc. 1995;93:291-294. |
| 6. | Hesselfeldt-Nielsen J, Geerdsen JP, Pedersen VM, et al Bleeding schwannoma of the small intestine: A diagnostic problem. Case report. Acta Chir Scand. 1987;153:623-625. |
| 7. | Hirasaki S, Hyodo I, Kajiwara T, Nishina T, Masumoto T. Malignant lymphoma with submucosal invasion in the terminal ileum diagnosed with colonoscopy and examined by endoscopic ultrasonography (in Japanese). Nippon Shokakibyo Gakkai Zasshi. 2004;101:41-46. |
| 8. | Quiroga S, Alvarez-Castells A, Pallisa E, Sebastia MC. Duodenal schwannoma causing gastrointestinal bleeding: helical CT findings. Abdom Imaging. 1997;22:154-155. |
| 9. | Gourtsoyiannis NC, Bays D, Papaioannou N, Theotokas J, Barouxis G, Karabelas T. Benign tumors of the small intestine: preoperative evaluation with a barium infusion technique. Eur J Radiol. 1993;16:115-125. |
| 10. | Zhou R, Popkin JH, Levey J. Jejunal schwannoma in neurofibromatosis. Am J Gastroenterol. 1999;94:275-276. |