Published online Oct 21, 2008. doi: 10.3748/wjg.14.6083
Revised: September 9, 2008
Accepted: September 16, 2008
Published online: October 21, 2008
A 76-year-old woman with a 5-mo history of recurrent diarrhea and generalized edema was admitted to our hospital. Colonoscopy revealed edematous mucosa, and histopathological examination was compatible with collagenous colitis. Protein leakage from the colon, particularly in the ascending portion, was identified on 99mTc-human serum albumin scintigraphy. Collagenous colitis associated with protein-losing enteropathy (PLE) without small bowel disease was diagnosed. Prednisolone treatment ameliorated diarrhea and hypoproteinemia. Collagenous colitis should be included in the differential diagnosis of chronic diarrhea with hypoproteinemia for appropriate management.
- Citation: Sano S, Yamagami K, Tanaka A, Nishio M, Nakamura T, Kubo Y, Inoue T, Ueda W, Okawa K, Yoshioka K. A unique case of collagenous colitis presenting as protein-losing enteropathy successfully treated with prednisolone. World J Gastroenterol 2008; 14(39): 6083-6086
- URL: https://www.wjgnet.com/1007-9327/full/v14/i39/6083.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6083
Since the first report in 1976[1], collagenous colitis has been found to be associated with a variety of conditions, including use of non-steroidal anti-inflammatory drugs[2] and proton pump inhibitors[3]. This condition is characterized by chronic watery diarrhea and abnormal deposition of collagen beneath the colonic epithelium[4]. Severe hypoproteinemia due to enteric protein loss is rare unless accompanied by small bowel malabsorption syndrome, such as celiac sprue. To the best of our knowledge, only 1 case of collagenous colitis associated with protein-losing enteropathy (PLE) in the absence of small bowel disease has been reported[5]. We report herein another case of collagenous colitis associated with PLE without small bowel disease, in which PLE was diagnosed by 99mTc-human albumin (HSA) scintigraphy.
A 76-year-old woman with a 5-mo history of recurrent diarrhea and generalized edema was admitted to our hospital. Repeated colonoscopies and gastrointestinal scope at a previous hospital had shown no abnormal changes in the gastrointestinal mucosa. The patient had been taking 180 mg of loxoprofen sodium and 30 mg of lansoprazole every day for the past 3 years, for osteoarthritis of the knees, but had otherwise been healthy with no prior history of gastrointestinal disease. Family history was unremarkable.
On admission, weight was 53 kg and height was 144 cm. She was afebrile, with a blood pressure of 128/84 mmHg and a heart rate of 82 beats/min. The right lower abdominal quadrant was slightly painful on palpation, the face was swollen, and pretibial pitting edema was also present. No superficial lymph nodes were palpable. Laboratory investigations revealed: white blood cells, 7960/mm3; C-reactive protein, 0.31 mg/dL; total protein, 4.8 g/dL; plasma albumin, 2.8 mg/dL; no abnormalities in liver, renal, thyroid and adrenal function tests; negative serology for rheumatoid factor; normal results of urinalysis and no proteinuria. Moreover, no steatorrhea was identified, indicating that malabsorption syndrome was unlikely.
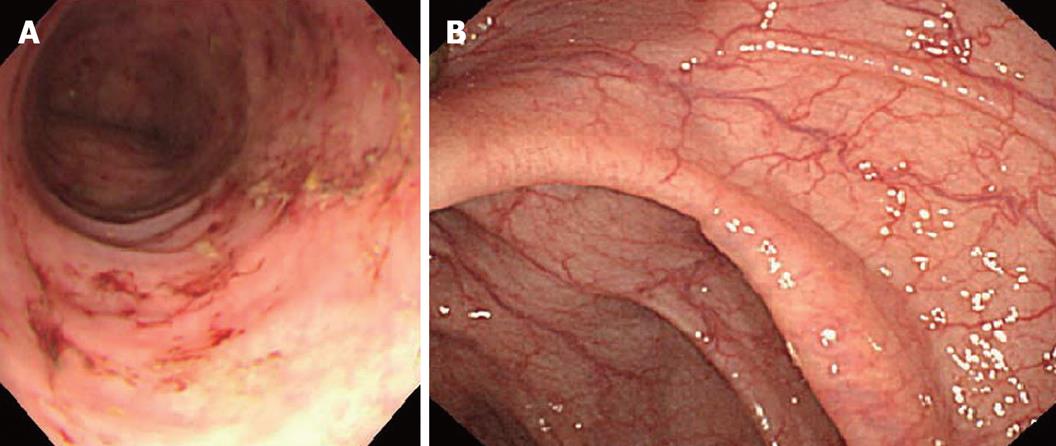
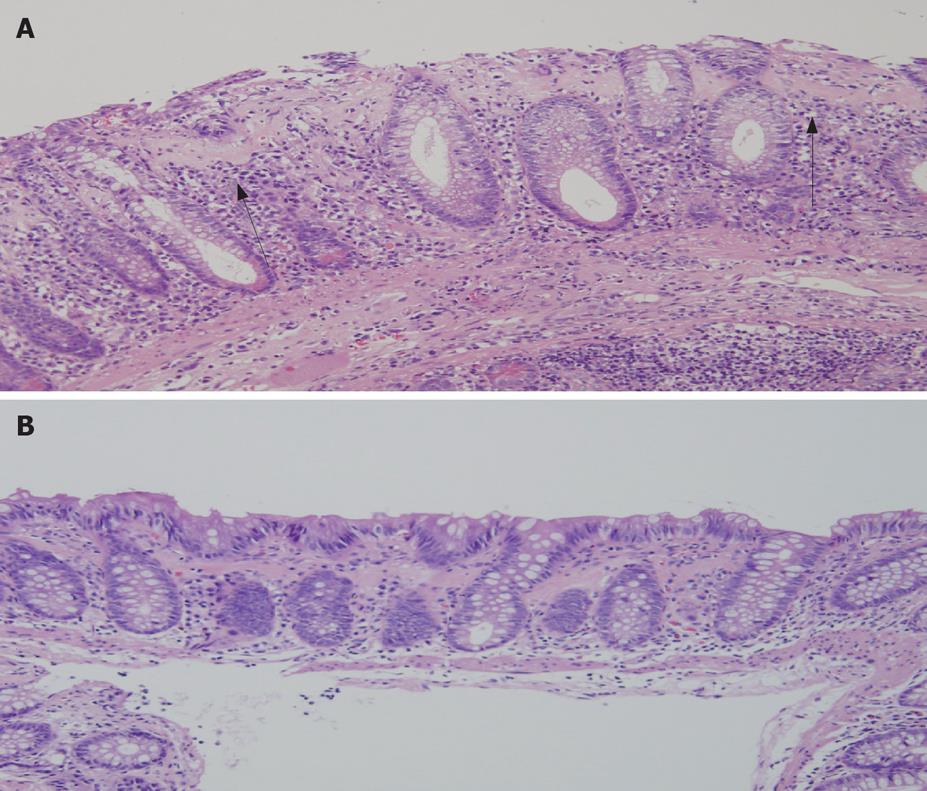
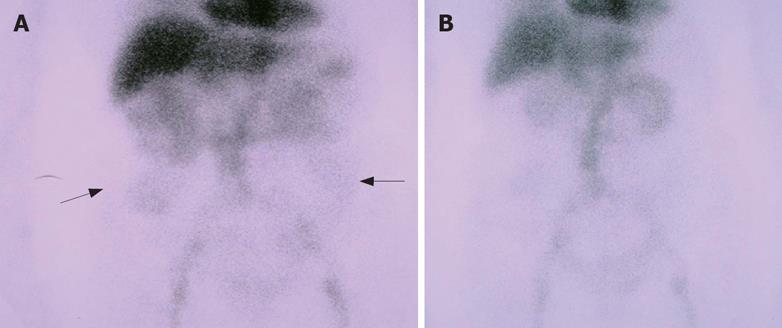
Endoscopic examination of the lower intestinal tracts showed edematous mucosa, diminished vascular transparency and multiple areas of erythema (Figure 1A). Multiple biopsies revealed changes consistent with collagenous colitis, showing prominent subepithelial eosinophilic band-like deposits with increased lymphocytes and plasma cells (Figure 2A). The distribution of the disease was whole colon and the findings were worse in the right compared to the left colon. The thickness of the collagen layer was 80-100 μm in the right and 40-50 μm in the left. There were no areas of cryptitis, crypt abscesses and no area of superimposed infection inflammatory bowel disease. Sloughing of surface epithelium was also identified. Endoscopic examination and biopsies of other portion of the gastrointestinal tract showed no obvious abnormalities in the stomach and the small intestine, and there was no evidence of celiac sprue. The duodenum showed normal villi and no obvious lymphocyte infiltration. Small bowel barium study showed no abnormalities. On 99mTc HSA scintigraphy, protein leakage was detected throughout the whole colon, particularly in the ascending portion (Figure 3A). No leakage was apparent from the stomach or small intestine. Neither chest/abdominal computed tomography (CT) nor 67Ga scintigraphy showed any evidence of malignancy. On the basis of these findings, collagenous colitis associated with PLE was diagnosed.
After diagnosis, loxoprofen sodium and lansoprazole were discontinued. However, general condition remained unimproved. Administration of 1.8 g polycarbophil calcium, 2 g natural aluminum silicate, 2 g bifidobacterium, 20 mg scopolamine butylbromide, 4 mg loperamide hydrochloride and 2 g albumin tannate likewise did not improve symptoms, and serum protein and albumin levels remained low despite administration of human serum albumin. Frequency of diarrhea increased and abdominal pain became extremely severe, and the condition of the patient deteriorated. We decided to start prednisolone therapy after hypovolemic shock developed. Soon after initiating prednisolone treatment at 30 mg/d, abdominal pain and diarrhea dramatically improved along with general condition. Total plasma protein and plasma albumin levels gradually increased to 5.4 g/dL and 3.4 g/dL, respectively, by 1 mo after starting prednisolone therapy. Follow-up endoscopy showed normal-appearing colonic mucosa (Figure 1B), and multiple biopsies showed decreased epithelial detachment and inflammatory cells, although the collagen band beneath the mucosa was not reduced (Figure 2B). Additional 99mTc HSA scintigraphy showed no accumulation of tracer in the large bowel, indicating remission of PLE (Figure 3B).
This patient presented with chronic diarrhea and anasarca with severe hypoproteinemia, and colonoscopic examination revealed collagenous colitis. We considered that hypoproteinemia was enteric in origin, as no proteinuria, liver disease, cardiac disease or other inflammatory disease was present. Severe enteric protein loss causing hypoproteinemia is reportedly rare in collagenous colitis unless accompanied by small bowel malabsorption syndrome. In the present case, coexistence of malabsorption syndrome was unlikely given the absence of steatorrhea, which is characteristic of malabsorption syndrome. Furthermore, histopathology of the duodenum revealed no evidence of celiac sprue.
The cause of hypoproteinemia was thus considered to be excessive enteric protein loss without malabsorption syndrome. Small bowel barium radiography showed no abnormality such as Crohn’s disease or malignant lymphoma, or other diseases that could cause PLE. Furthermore, 99mTc HSA scintigraphy revealed no accumulation of tracer in the small bowel. Considering that no obvious small bowel disease was present, collagenous colitis itself might have been the cause of PLE and 99mTc HSA scintigraphy is useful in this case[6,7].
Although the mechanisms of enteric protein loss in patients with collagenous colitis have not been clarified, abnormalities of the surface epithelium[8], superficial capillaries[9] and pericryptal fibroblasts[10] have been hypothesized. Long-term use of loxoprofen sodium and lansoprazole may be associated in the pathogenesis of severity of collagenous colitis in this patient. In the present case, histological examination revealed marked reductions in epithelial detachment together with clinical improvement after prednisolone therapy, suggesting that abnormalities of surface epithelium play an important role in the development of PLE. The endoscopic findings of collagenous colitis are thought to be normal and nonspecific[11]. In the present case, however, endoscopic examination revealed edematous mucosa, diminished vascular transparency and multiple red spots, and histological examination revealed sloughing of surface epithelium, suggesting this was a severe case of collagenous colitis. This may be one reason why the patient developed PLE.
No established treatments have yet been defined for PLE associated with collagenous colitis[12]. Corticosteroids are occasionally used for the treatment of collagenous colitis and some studies have shown that prednisolone treatment is ineffective[13] and budesonide is effective for collagenous colitis without PLE[14,15]. As oral budesonide is unavailable in Japan, prednisolone treatment was selected because prednisolone has been reported to ameliorate PLE caused by other diseases through the reduction of submucosal edema and inflammation in the gastrointestinal tract. In the present case, oral prednisolone was effective for refractory diarrhea and exudative enteropathy. Corticosteroid was provided at a dose of 30 mg/d, and general status of the patient immediately improved in parallel with a decrease in the frequency of diarrhea and an increase in serum total protein.
Abnormal protein leakage on 99mTc HSA scintigraphy was diminished and biopsy specimens from the colon after treatment histopathologically reflected the efficacy of this therapy in terms of reduced epithelial sloughing and inflammatory cells, although the collagen band under the mucosa was largely unchanged. These results suggest that treatment with prednisolone may be effective for PLE associated with collagenous colitis.
In summary, we have reported a patient with collagenous colitis who presented with PLE. Prednisolone treatment ameliorated diarrhea and hypoproteinemia. Collagenous colitis should be included in the differential diagnosis of chronic diarrhea with hypoproteinemia to achieve appropriate management.
Peer reviewer: Robert Daniel Odze, PhD, Department of Gastrointestinal Pathology, Brigham and Women's Hospital, 75 Francis St., Boston MA, United States
S- Editor Li DL L- Editor Ma JY E- Editor Yin DH
| 1. | Lindstrom CG. 'Collagenous colitis' with watery diarrhoea--a new entity? Pathol Eur. 1976;11:87-89. |
| 2. | Riddell RH, Tanaka M, Mazzoleni G. Non-steroidal anti-inflammatory drugs as a possible cause of collagenous colitis: a case-control study. Gut. 1992;33:683-686. |
| 3. | Rammer M, Kirchgatterer A, Hobling W, Knoflach P. Lansoprazole-associated collagenous colitis: a case report. Z Gastroenterol. 2005;43:657-660. |
| 4. | Mogensen AM, Olsen JH, Gudmand-Hoyer E. Collagenous colitis. Acta Med Scand. 1984;216:535-540. |
| 5. | Stark ME, Batts KP, Alexander GL. Protein-losing enteropathy with collagenous colitis. Am J Gastroenterol. 1992;87:780-783. |
| 6. | Chiu NT, Lee BF, Hwang SJ, Chang JM, Liu GC, Yu HS. Protein-losing enteropathy: diagnosis with (99m)Tc-labeled human serum albumin scintigraphy. Radiology. 2001;219:86-90. |
| 7. | Hubalewska-Hola A, Sowa-Staszczak A, Szczerbinski T, Lis G, Huszno B, Szybinski Z. [Protein losing enteropathy (PLE) detected by Tc99m-labelled human serum albumin abdominal scintigraphy--case report]. Przegl Lek. 2003;60:606-608. |
| 8. | Jessurun J, Yardley JH, Giardiello FM, Hamilton SR, Bayless TM. Chronic colitis with thickening of the subepithelial collagen layer (collagenous colitis): histopathologic findings in 15 patients. Hum Pathol. 1987;18:839-848. |
| 9. | Teglbjaerg PS, Thaysen EH. Collagenous colitis: an ultrastructural study of a case. Gastroenterology. 1982;82:561-563. |
| 10. | Hwang WS, Kelly JK, Shaffer EA, Hershfield NB. Collagenous colitis: a disease of pericryptal fibroblast sheath? J Pathol. 1986;149:33-40. |
| 11. | Freeman HJ. Collagenous mucosal inflammatory diseases of the gastrointestinal tract. Gastroenterology. 2005;129:338-350. |
| 12. | Chande N, McDonald JW, Macdonald JK. Interventions for treating collagenous colitis. Cochrane Database Syst Rev. 2008;CD003575. |
| 13. | Munck LK, Kjeldsen J, Philipsen E, Fischer Hansen B. Incomplete remission with short-term prednisolone treatment in collagenous colitis: a randomized study. Scand J Gastroenterol. 2003;38:606-610. |
| 14. | Bonderup OK, Hansen JB, Madsen P, Vestergaard V, Fallingborg J, Teglbjaerg PS. Budesonide treatment and expression of inducible nitric oxide synthase mRNA in colonic mucosa in collagenous colitis. Eur J Gastroenterol Hepatol. 2006;18:1095-1099. |
| 15. | Lanyi B, Dries V, Dienes HP, Kruis W. Therapy of prednisone-refractory collagenous colitis with budesonide. Int J Colorectal Dis. 1999;14:58-61. |