Published online Oct 21, 2008. doi: 10.3748/wjg.14.6024
Revised: September 20, 2008
Accepted: September 27, 2008
Published online: October 21, 2008
AIM: To evaluate and present our experience with laparoscopic Roux en Y gastric bypass (RYGB) in a selected patient population.
METHODS: A cohort of 130 patients with a body mass index (BMI) between 35 and 50 kg/m2 were evaluated in relation to postoperative morbidity, weight loss and resolution of co-morbidities for a period of 4 years following laparoscopic RYGB.
RESULTS: Early morbidity was 10.0%, including 1 patient with peritonitis who was admitted to Intensive Care Unit (ICU) and 1 conversion to open RYGB early in the series. There was no early or late mortality. Maximum weight loss was achieved at 12 mo postoperatively, with mean BMI 30 kg/m2, mean percentage of excess weight loss (EWL%) 66.4% and mean percentage of initial weight loss (IWL%) 34.3% throughout the follow-up period. The majority of preexisting comorbidities were resolved after weight loss and no major metabolic disturbances or nutritional deficiencies were observed.
CONCLUSION: Laparoscopic RYGB appears to be a safe and effective procedure for patients with BMI 35-50 kg/m2 with results that are comparable to previously published data mostly from the USA but from Europe as well.
- Citation: Vagenas K, Panagiotopoulos S, Kehagias I, Karamanakos SN, Mead N, Kalfarentzos F. Prospective evaluation of laparoscopic Roux en Y gastric bypass in patients with clinically severe obesity. World J Gastroenterol 2008; 14(39): 6024-6029
- URL: https://www.wjgnet.com/1007-9327/full/v14/i39/6024.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6024
| Period of study | September 2003 to June 2008 |
| Number of patients | 130 |
| Male:Female | 21:109 |
| Age (yr) | 37 ± 9.4 (18-55) |
| Weight (kg) | 125 ± 13.4 (95-170) |
| Excess weight (kg) | 65 ± 9.7 (39-103) |
| % EBW | 208 ± 14.5 (160.9-253.7) |
| ΒΜΙ (kg/m2) | 46 ± 3.0 (37.5-50) |
| Comorbidities | No. of patients (%) |
| Hypertension | 21 (16.3) |
| COPD | 22 (17.0) |
| Sleep apnea | 13 (10.0) |
| Osteoarthritis | 21 (16.3) |
| Depression | 11 (8.5) |
| Diabetes Mellitus | 24 (18.6) |
| OGTT | 8 (6.2) |
| Hypercholesterolemia | 64 (49.6) |
| Hypertriglyceridemia | 36 (27.9) |
| Time | Complications | Treatment | % of patients |
| Early < 30 d | |||
| 3 gastrointestinal hemorrhages | Conservative (2) | 2.4 | |
| Operation (1) | |||
| 2 enterocutaneous fistulas | Operation | 1.6 | |
| 1 peritonitis | Operation, ICU admission | 0.8 | |
| 1 ileus due to volvulus | Operation | 0.8 | |
| 1 portal vein thrombosis | Anticoagulants | 0.8 | |
| 1 wound infection of port site | Antibiotics | 0.8 | |
| 2 orthopedic injuries | Immobilization | 1.6 | |
| 1 atelectasis | Antibiotics peros | 0.8 | |
| No incisional hernia | 0.0 | ||
| 1 anastomotic leak | Conservative | 0.8 | |
| Intermediate 30-90 d | |||
| 1 incisional hernia | No operation | 0.8 | |
| Late > 90 d | |||
| 5 incisional hernias | Operation (4) | 3.9 | |
| 4 episodes of ileus | Operation (1) | 3.1 | |
| Conservative (3) | |||
| 1 suicide attempt | 0.8 | ||
| 1 gastrojejunal anastomosis stenosis | Endoscopic dilatation | 0.8 | |
| 0 mo | 12 mo | 24 mo | 36 mo | 48 mo | |
| Patients | 130 | 110 | 85 | 51 | 16 |
| Weight (kg) | 125 | 81.6 | 81.4 | 84.1 | 79.2 |
| BMI | 46 | 30 | 31 | 32 | 31 |
| IWL % | 34.2 | 34.3 | 32.2 | 31.4 | |
| EWL % | 66.2 | 65.9 | 61.5 | 61.1 | |
| Pts > 50% EWL | 92 | 68 | 35 | 12 |
| Comorbidities | No. of patients | Follow- up period (mo) | Resolved (%) | Improved (%) | Without change (%) |
| Hypertension | 21 | 24 | 84 | 16 | |
| COPD | 22 | 12 | 100 | ||
| Sleep apnea | 13 | 12 | 100 | ||
| Osteoarthritis | 21 | 12 | 100 | ||
| Depression | 11 | 24 | 89 | 11 | |
| Diabetes Mellitus | 24 | 12 | 91.7 | 8.3 | |
| OGTT | 8 | 12 | 100 | ||
| Hypercholesterolemia | 64 | 36 | 94.4 | 5.6 | |
| Hypertriglyceridemia | 36 | 12 | 100 |
Obesity has reached epidemic proportions in society today[1] and it is associated with high rates of morbidity and mortality due to the presence of severe comorbidities, many of which show complete resolution after weight loss[2]. According to published data, surgery is the only reliable way of achieving both adequate and long-term weight loss in the morbidly obese population[3]. Roux en Y gastric bypass (RYGB), which was first described by Mason and Ito at the University of Iowa in 1967, is now considered the gold standard of bariatric procedures[4]. In 1994, Wittgrove et al[5] first introduced a totally laparoscopic approach to this procedure, which is now a routine practice for the majority of bariatric centers in United States and this trend seems to be spreading throughout Europe as well. However, there are few published studies to date regarding the implementation of this procedure in Europe[6].
The aim of this study, therefore, is to report the experience of a single centre in Greece with the laparoscopic RYGB.
Since 1994, 1095 surgical procedures for clinically severe obesity have been performed at our institution. The type of procedure performed is based on specific selection criteria according to an algorithm developed by our center, whereby patients with body mass index (BMI) over 50 kg/m2 undergo biliopancreatic diversion with RYGB (BPD-RYGB), as modified in our center[7], while patients with BMI < 50 kg/m2 undergo RYGB with long limb (RYGB-LL) or sleeve gastrectomy (SG) depending on comorbidities and eating habits. Sweet consumers and patients with diabetes mellitus undergo RYGB-LL whereas volume consumers may undergo SG. Since October 2003 in patients with BMI < 50 kg/m2 all procedures have been performed laparoscopically, and the present study refers to 130 of these patients who underwent RYGB-LL as their primary procedure.
All patients participated in a multistage educational and informational program to accomplish full disclosure preoperatively and to engage them in compliance with bariatric management postoperatively.
A multidisciplinary team including the surgeon, an endocrinologist, a cardiologist, a pneumonologist, a psychiatrist and a nutritionist-dietitian evaluate all patients preoperatively and postoperatively to assess and optimize their physical condition. Table 1 shows the patients’ preoperative characteristics and Table 2 shows the patients’ preoperative comorbidities.
At the operating room, during induction in anesthesia, a single dose of antibiotics (cephalosporin second generation 1.5 g and metronidazole 500 mg) was given and continued for 48 h postoperatively. Thromboembolic prophylaxis using low molecular weight heparin at a dose adapted to patients’ weight was started the day before operation and continued till the discharge. Complementary measures consisting of air compression boots and specially designed mattress were used.
The main characteristics of the RYGB-LL are a gastric pouch of 15 ± 5 mL, a biliopancreatic limb of 50 cm, an alimentary limb of 150 cm and the remainder of small intestine as the common limb. We prefer to pass the alimentary limb antecolic and antegastric and to create a gastrojejunostomy using a 25 mm circular stapler performing a circular end to end anastomosis (CEEA) by passing the anvil transorally. The gastrojejunostomy is reinforced with interrupted non-absorbable sutures. The proximal end of Roux limb is closed with application of linear stapler. A side to side jejunojejunostomy is performed using a linear stapler and the mesenteric defects are closed with non-absorbable running sutures.
Cholecystectomy is always added to the main procedure. Furthermore, because fatty liver and non-alcoholic steatohepatitis are common, liver biopsy is routinely performed to assess preoperatively liver histopathology and will be used as a baseline for comparison if a problem in hepatic function arises in the future.
Patients were mobilized in the evening of surgery. Pain management consisted of parecoxib 40 mg intravenously every 12 h and meperidine 50 mg intramuscularly as needed for 3 d.
On the fourth postoperative day, after an uneventful upper gastrointestinal evaluation, a clear liquid diet was begun with gradual progression to full liquids and blenderized food. High protein supplements were administered to all patients until 4 wk postoperatively when per os feeding was advanced by the nutritionist.
All patients received a daily multivitamin and mineral supplement and 1000 mg of calcium. An iron supplement was also prescribed for premenopausal women at a dose of 80 mg/d. After the 6th postoperative month, vitamin B12 supplementation was given intramuscularly at a dose of 1000-3000 μg depending upon the measured values.
Follow-up visits were scheduled at 1, 3, 6 and 12 mo postoperatively and annually thereafter. Each follow-up visit included complete medical and nutritional evaluation, with laboratory workup and evaluation by other specialists as needed.
The data presented are expressed as mean ± SD, unless otherwise stated. During the study comparisons of the observed values at various time periods were performed using ANOVA (one way analysis of variance). If there were any statistic significant differences, the Tukey post-test was used to determine the time points that contribute to this significance.
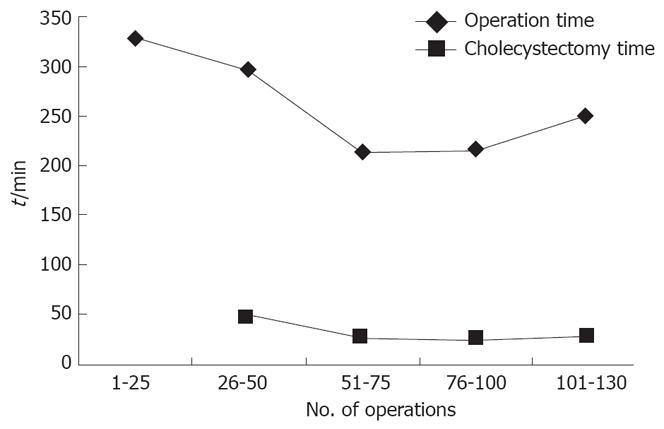
From October 2003 to June 2008, 130 patients with BMI 35-50 kg/m2 underwent laparoscopic RYGB-LL as their primary bariatric operation. In addition, cholecystectomy was performed in all but nine patients who had previously undergone this procedure elsewhere and other abdominal procedures were performed in five patients. The mean total operative time was 260 ± 87.4 min (range 120-270) and the mean operative time for cholecystectomy was 18 ± 17.2 min (range 15-70). The operative time decreased significantly over time, especially after the first 50 cases (P < 0.05) (Figure 1). Conversion to open RYGB was necessary in one patient (0.8%) early in the series.
The mean length of hospital stay was 9 d (range 8-29) primarily due to standard hospital protocol in Greece. The mean follow-up time was 24.3 mo (range 1-48). The number of patients who successfully completed follow-up was 110 of 112 patients (98.2%) at 12 mo, 85 of 90 patients (94.4%) at 24 mo, 51 of 55 patients (92.7%) at 36 mo and 16 of 18 patients (88.9%) at 48 mo. Four patients were lost to follow-up. Thus far there has been no need for revision surgery.
There was no early or late mortality.
Intraoperative period: One conversion to open RYGB was necessary early in the series, due to inability to construct the jejuno-jejuno anastomosis.
Early postoperative period (< 30 d): In the early postoperative period, as shown in Table 3, there were three gastrointestinal haemorrhages, one of which was intraluminal, probably from the jejunojejunal anastomosis, presenting as small obstruction and requiring reoperation, while the others were intrabdominal and treated conservatively. In addition, there were two enterocutaneous fistulas, caused by attachment of small intestine loop to mesh after simultaneous repair of incisional hernias, one episode of ileus due to volvulus and one case of peritonitis, all of which required surgical intervention. The last patient required admission to the Intensive Care Unit (ICU) after reoperation for peritonitis caused by leakage of the alimentary limb stump on the 6th postoperative day. The latter was caused by herniation of a small bowel limb to port site. The patient was finally discharged 168 d after surgery following a complicated and difficult postoperative course, including acute compartment syndrome requiring reoperation and development of acute renal insufficiency requiring dialysis. There was also one episode of portal vein thrombosis treated with anticoagulant medication, one wound infection of port site treated with antibiotics, one lung atelectasis, two orthopaedic injuries due to inappropriate patient positioning and securing intraoperatively. Finally, there was one anastomotic leakage from gastrojejunal anastomosis, which presented on the 6th postoperative day with severe sepsis without hemodynamic instability and was treated successfully conservatively with drainage under computer tomography (CT) guidance and total parenteral nutrition. The total early postoperative morbidity was 10.0% (13 patients).
Intermediate postoperative period (30-90 d): During the intermediate postoperative period there was one incisional hernia with no other major complications.
Late postoperative period (> 90 d): During the late postoperative period there were 5 incisional hernias, 4 of which were treated surgically, 4 episodes of small bowel obstruction, one of which was due to adhesions requiring surgical intervention, one episode of gastrojejunal anastomosal stenosis, which was treated with endoscopic dilation and one suicide attempt 5 mo after surgery due to undetected severe pre-existing depression.
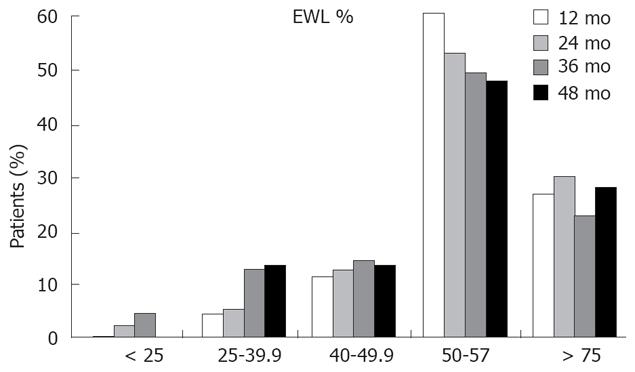
The results of weight loss expressed as actual weight, BMI, percentage of excess weight loss (EWL%) and percentage of initial weight loss (IWL%) at 12, 24, 36 and 48 mo, respectively, are shown in Table 4. Maximum weight loss was observed at 12 mo, with mean BMI 30 kg/m2, mean EWL 66.4% and mean IWL 34.3% which remained stable throughout the follow-up period. Ninety-two (83.6%) of 110 patients achieved an EWL of at least 50% at 12 mo which was maintained throughout the follow-up period (Figure 2). An EWL of 50% is considered successful.
Comorbidities were present in 117 (90.7%) patients preoperatively with an average of 3 ± 2.6 (range 0-10) per patient. The majority of these showed significant improvement during the 48 mo follow-up. Table 5 presents the postoperative results of relevant comorbidities.
Hypertension was present in 21 patients (16.3%) preoperatively, 16 of whom (76.2%) were on medication. After the 2nd postoperative year, only one patient (4.8%) remained on antihypertensive medication.
Preoperatively 24 patients had diabetes mellitus (blood glucose > 125 mg/dL), 14 of whom were on oral hypoglycemic agents while 2 were being treated with insulin. An additional 8 patients had impaired oral glucose tolerance test (OGTT) preoperatively. Postoperatively, diabetes mellitus was completely resolved in 22 patients (91.7%) by the 12 mo follow-up. Only one patient remained on insulin therapy throughout the study period.
Hypercholesterolemia (blood cholesterol > 200 mg/dL) was present in 64 patients preoperatively. Mean cholesterol levels were 230 ± 28.8 mg/dL preoperatively and had decreased to 179 ± 42 mg/dL by the 12 mo follow-up and remained at these levels for the rest of the follow-up period. Among the 52 of 64 patients who completed the 12 mo follow-up, 14 (26.9%) still had elevated blood cholesterol levels > 200 mg/dL. By the 36th month following surgery, only 6 of the 24 patients (25.0%) still had cholesterol levels > 200 mg/dL.
There were 34 patients with hypertriglyceridemia (TGs > 160 mg/dL) preoperatively, with mean levels 225 ± 64.8 mg/dL. Postoperatively, mean TGs levels dropped to 96 ± 33.2 mg/dL and 96 ± 37.7 mg/dL at 12 and 24 mo respectively and none of the patients had hypertriglyceridemia.
Anaemia: Anaemia, as defined by haemoglobin level < 13.5 mg/dL in men and < 12.5 mg/dL in women, was observed at mean rate of 20.1%. More specifically, a low haemoglobin level was seen in 14.8%, 20.2%, 22% and 26.7% of patients at 12, 24, 36 and 48 mo, respectively. Regarding other parameters associated with anaemia including iron (< 35 μg/dL), vitamin B12 (< 200 pg/mL) and ferritin (< 9 ng/mL), the mean rates of postoperative deficiency were 6.1%, 18.7% and 10.0%, respectively. No deficiency of folic acid was observed following surgery and none of the above deficiencies were clinically severe. All patients were treated successfully with oral supplementation.
Hypoalbuminemia: Hypoalbuminemia did not occur at any time during the postoperative follow-up. The mean levels of albumin were > 4 g/dL at all follow-up evaluation and no patient presented with albumin levels below the minimum normal level.
In this study, 130 patients underwent laparoscopic RYGB-LL with an acceptable total early complication rate (minor and major) 10.0%, a low conversion rate (0.8%) and no mortality.
The mean hospital stay was quite high (9 d) but this is due to the existing health care system in Greece, which lacks the services of early postoperative care for patients from distant places.
Maximum weight loss in our series was achieved at 12 mo, with a mean EWL of 66.4%, which was maintained through out the study period. However, 14% of patients did not achieve adequate weight loss (EWL < 50%) and the reason for these failures has not been clarified yet causing problems for the surgeons and the patients.
In addition to adequate weight loss, improvement of pre-existing comorbidities is one of the most important criteria for evaluating success of a bariatric procedure. In our study, as in others[1,2,6,8-10], that was achieved, as shown in Table 2. Diabetes mellitus was completely resolved in the majority of the patients, finding supported by other reports, which also proposed mechanisms that this can be achieved[11,12]. Hypercholesterolemia was resolved in the majority of patients and hypertriglyceridemia in all patients, results similar to those described for malabsorptive procedures[13,14]. Regarding metabolic complications the most significant were vitamin B12 and iron deficiency. However there was no clinical impact and all the patients were treated conservatively with intramuscular injections of vitamin B12 and oral iron supplements as necessary.
The surgical complications rate in our series was comparable to that described by others[6,15-20] and included primarily gastrointestinal haemorrhages, enterocutaneous fistulas and obstructive ileus. We had no internal hernias, which was probably due to the antecolic position of the Roux limb[21]. Furthermore, the low incidence of anastomotic gastrointestinal stricture (0.8%) may be attributed to the use of 25 mm circular stapler. The prevalence of wound infection and anastomotic leakage was similar to that reported by others[15,17,18].
The laparoscopic approach to bariatric surgery is technically challenging, but with experience it can be mastered. The learning curve is steep and long operating times are required[22]. As shown in Figure 2, our operating time decreased significantly as our experience accumulated, which was supported by Wittgrove et al[5]. Since practice makes perfection, we could also manage to improve our port-site closure technique and after the first 5 unfortunate incisional hernias there was no new case recorded. Furthermore, our 2 cases of enterocutaneous fistulas were attributed to simultaneous mesh placement and eventually this approach was abandoned.
Our results suggest that laparoscopic RYGB-LL as performed at our institution provides adequate weight loss and resolution or improvement of comorbidities up to 4 years. Recently, it has been increasingly recognised that RYGB may have an effect on appetite and eating behaviour, which, in turn, may improve long-term results. These effects may be related to changes in the circulating levels of the gastrointestinal hormones known to influence appetite including PYY[7,23-28], and this may play a role in the overall success of the procedure.
In our experience laparoscopic Roux-en-Y gastric bypass appears to be a safe and effective surgical procedure for patients with BMI 35-50 kg/m2 with results which are comparable to previously published data primarily from the USA, but some from Europe as well. It is associated with minor postoperative pain, early patient mobilization, low incidence of perioperative complications, improvement or complete resolution of preexisting comorbidities and weight loss results that are comparable to those seen following the open procedure. For all these reasons we consider laparoscopic RYGB-LL to be a procedure of choice for the treatment of clinically severe obesity in properly selected patients.
Obesity, has reached epidemic proportions in society today and it is associated with high rates of morbidity and mortality due to the presence of severe comorbidities. Surgery is the only reliable way of achieving adequate and long-term weight loss in the morbidly obese population. Nowadays, Roux en Y gastric bypass (RYGB) is considered as the gold standard of bariatric procedures. In the present study, the experience of a single centre in Greece with the laparoscopic RYGB is reported.
Laparoscopic RYGB-LL as performed at authors’ institution provides adequate weight loss and resolution or improvement of comorbidities up to 4 years. Apparently, RYGB seems to have an effect on appetite and eating behaviour, which, in turn, may improve long term results. These effects are related to changes in the circulating levels of the gastrointestinal hormones known to influence appetite including ghrelin, PYY and GLP-1. Further in depth research upon this topic is required in order to elucidate the precise mechanisms involved in weight loss.
According to authors’ experience, laparoscopic Roux-en-Y gastric bypass appears to be a safe and effective surgical procedure for patients with BMI 35-50 kg/m2. The vast majority of their complications occurred early at the learning curve. The authors were able to minimize their complication rate and further improve operation and shorten hospitalization.
Laparoscopic RYGB-LL is a safe and efficious bariatric procedure as it is associated with minor postoperative pain, early patient mobilization, low incidence of perioperative complications, improvement or complete resolution of preexisting comorbidities and durable weight loss. For these reasons, it should be a procedure of choice for the treatment of clinically severe obesity in properly selected patients.
A single institutional series of 130 patients with laparoscopic gastric bypass is presented. Although not a huge series the results are excellent and the series is from a European country where lap gastric bypass is less common. The manuscript is likely of interest.
Peer reviewer: Leonidas G Koniaris, Professor, Alan Livingstone Chair in Surgical Oncology, 3550 Sylvester Comprehensive Cancer Center (310T), 1475 NW 12th Ave, Miami, FL 33136, United States
S- Editor Li DL L- Editor Ma JY E- Editor Yin DH
| 1. | Elder KA, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132:2253-2271. |
| 2. | Deitel M. How much weight loss is sufficient to overcome major co-morbidities? Obes Surg. 2001;11:659. |
| 3. | Sugerman HJ. Treatment of obesity. J Gastrointest Surg. 2003;7:476-477. |
| 4. | DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176-2183. |
| 5. | Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic Gastric Bypass, Roux-en-Y: Preliminary Report of Five Cases. Obes Surg. 1994;4:353-357. |
| 6. | Suter M, Paroz A, Calmes JM, Giusti V. European experience with laparoscopic Roux-en-Y gastric bypass in 466 obese patients. Br J Surg. 2006;93:726-732. |
| 7. | Kalfarentzos F, Papadoulas S, Skroubis G, Kehagias I, Loukidi A, Mead N. Prospective evaluation of biliopancreatic diversion with Roux-en-Y gastric bypass in the super obese. J Gastrointest Surg. 2004;8:479-488. |
| 8. | O'Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032-1040. |
| 9. | Lujan JA, Frutos MD, Hernandez Q, Liron R, Cuenca JR, Valero G, Parrilla P. Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg. 2004;239:433-437. |
| 10. | Puzziferri N, Austrheim-Smith IT, Wolfe BM, Wilson SE, Nguyen NT. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg. 2006;243:181-188. |
| 11. | Polyzogopoulou EV, Kalfarentzos F, Vagenakis AG, Alexandrides TK. Restoration of euglycemia and normal acute insulin response to glucose in obese subjects with type 2 diabetes following bariatric surgery. Diabetes. 2003;52:1098-1103. |
| 12. | Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, Barakat HA, deRamon RA, Israel G, Dolezal JM. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339-350; discussion 350-352. |
| 13. | Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737. |
| 14. | Nguyen NT, Varela E, Sabio A, Tran CL, Stamos M, Wilson SE. Resolution of hyperlipidemia after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg. 2006;203:24-29. |
| 15. | Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ, Wolfe BM. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234:279-289; discussion 289-291. |
| 16. | Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232:515-529. |
| 17. | Westling A, Gustavsson S. Laparoscopic vs open Roux-en-Y gastric bypass: a prospective, randomized trial. Obes Surg. 2001;11:284-292. |
| 18. | Jones DB, Provost DA, DeMaria EJ, Smith CD, Morgenstern L, Schirmer B. Optimal management of the morbidly obese patient. SAGES appropriateness conference statement. Surg Endosc. 2004;18:1029-1037. |
| 19. | Brolin RE, Kenler HA, Gorman JH, Cody RP. Long-limb gastric bypass in the superobese. A prospective randomized study. Ann Surg. 1992;215:387-395. |
| 20. | Nguyen NT, Longoria M, Chalifoux S, Wilson SE. Gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2004;14:1308-1312. |
| 21. | Iannelli A, Facchiano E, Gugenheim J. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-1271. |
| 22. | Schauer P, Ikramuddin S, Hamad G, Gourash W. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc. 2003;17:212-215. |
| 23. | le Roux CW, Aylwin SJ, Batterham RL, Borg CM, Coyle F, Prasad V, Shurey S, Ghatei MA, Patel AG, Bloom SR. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243:108-114. |
| 24. | Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 2002;418:650-654. |
| 25. | Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, Ghatei MA, Bloom SR. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. 2003;349:941-948. |
| 26. | Stock S, Leichner P, Wong AC, Ghatei MA, Kieffer TJ, Bloom SR, Chanoine JP. Ghrelin, peptide YY, glucose-dependent insulinotropic polypeptide, and hunger responses to a mixed meal in anorexic, obese, and control female adolescents. J Clin Endocrinol Metab. 2005;90:2161-2168. |
| 27. | le Roux CW, Batterham RL, Aylwin SJ, Patterson M, Borg CM, Wynne KJ, Kent A, Vincent RP, Gardiner J, Ghatei MA. Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology. 2006;147:3-8. |