INTRODUCTION
Figure 1 Endoscopic lesions compatible with severe colitis.
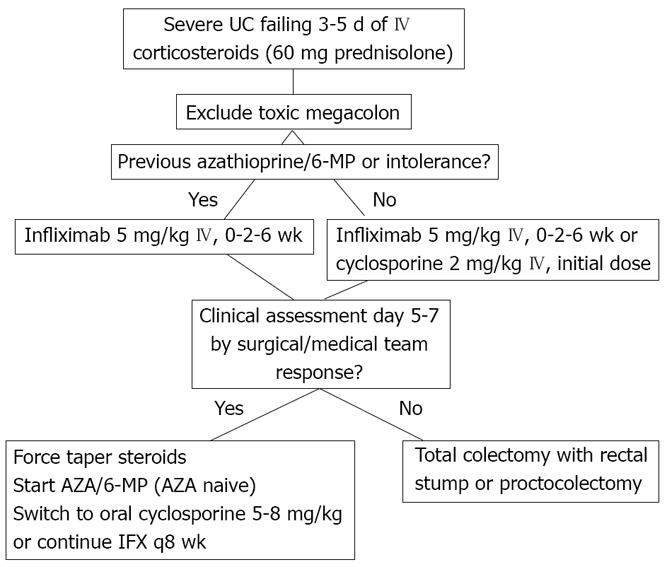
Figure 2 Proposed treatment algorithm for the management of severe steroid refractory ulcerative colitis.
Some patients with ulcerative colitis (UC) remain symptomatic despite optimal doses of oral 5-aminosalicylic acid (5-ASA) drugs, topical therapy with either 5-ASA or steroids, and systemic corticosteroids. This can occur regardless of the extent of colonic involvement. However, steroids are highly efficacious in UC. Failure to induce remission will occur in only 40% of patients after a first course of oral systemic steroids and only 20% will have no improvement of symptoms whatsoever[1,2]. In patients with early relapse after an initial successful course of systemic steroids, subsequent courses of steroids are probably less efficacious, but this has never been studied in a controlled trial. The term “steroid refractory” has been used to define patients whose symptoms never responded to corticosteroids and those who respond initially but developed recurrence while continuing treatment. The distinction can be important since treatment options in the two settings may differ. In patients who have initially responded, the dose of oral steroids can be temporarily increased to the dose level that controlled symptoms before, whereas patients never responding need alternative options on the short term.
GENERAL TREATMENT RECOMMENDATIONS
The approach to treatment should be based on the severity of the disease flare. Moderately ill patients can usually be managed in an outpatient setting with the approaches summarized below. Disease flares are considered to be moderate or moderate-to-severe when symptoms impair with activities of daily life, but are not necessitating immediate hospitalization. Fulminant UC necessitates IV therapy in hospital as described below and regardless of previous oral steroid use[3].
APPROACH TO SEVERE ATTACKS OF ULCERATIVE COLITIS
Only 15 to 20 percent of patients with UC will ever experience an attack of fulminant colitis[4]. Patients with pancolitis appear to be predisposed to severe flares (Figure 1). Severe UC is a serious, potentially life threatening condition and hospitalization should be considered in all patients who have more than 6-10 bloody stools per day, associated with fever, dehydration, tachycardia malaise and/or increased C-reactive Proteine (CRP)[3,4,5]. Patients entering hospital with fulminant colitis should be evaluated for other causes of severe colitis. We always perform an un-prepped sigmoidoscopy to assess disease severity, to obtain mucosal biopsies, and to provide a baseline assessment. Total colonoscopy and ileoscopy should not be attempted as it carries the risk of inducing toxic megacolon. As a rule sigmoidoscopy in fulminant colitis should be performed by an experienced endoscopist with minimal inflation and at the first sign of discomfort from the patient no further proximal progression should be attempted. Infectious colitis should be excluded with stool culture for bacterial pathogens, C. difficile toxin test in stools and ova/parasites in a fresh stool sample and careful assessment of the mucosal biopsies. The likelihood of infectious colitis is geographically determined but should be considered in all patients. Although the precise role of active cyto-megalo virus (CMV) replication in fulminant colitis is still debated, the presence of CMV inclusions in a colonic biopsy should be ruled out. In the recent patient history foreign travel and non steroidal anti inflammatory drugs (NSAID) use should be recorded. Clinically disease severity should be assessed using the criteria in the Lichtiger score including stool frequency, nocturnal diarrhea and fecal incontinence, rectal bleeding, abdominal cramping and tenderness and general well being. Others signs of fulminant colitis include fever, lethargy and dehydration. Blood analysis should include: serum albumine, electrolytes, hemoglobin, white blood cell count (WBD) and differential, CRP, blood urea nitrogen (creatinine) (BUN) and liver tests[2]. A plain abdominal X-ray should be obtained initially and at regular intervals during the hospitalization. We generally treat those patients with IV prednisolone (60 mg daily) or equivalent as a continuous infusion regardless of prior oral corticosteroid therapy. Pioneering studies by Truelove et al[1] have shown that applying this strategy 64 percent of patients will enter clinical remission and only 23 percent require rescue total procto-colectomy. Doses higher than 60 mg or 1 mg/kg prednisolone equivalent are not recom-mended. Although recent controlled evidence failed to show superiority of a continuous infusion of methyl-prednisolone 1 mg/kg IV daily over and IV bolus therapy at the same dose, most centers still prefer continuous infusion. Supportive therapy for this condition includes relative bowel rest and parenteral nutrition if needed. The value of antibiotics as a prophylactic or adjuvant therapy in the setting of fulminant colitis has not been established. However, patients with high fever, signs of peritonitis or high CRP levels should receive broad spectrum antibiotics (e.g. ciprofloxacin + metronidazole). Even so, initiation of antibiotics should never postpone the decision for procto-colectomy.
If patients fail to respond to three to five days of IV steroids, they should be considered for intensified medical therapy (described below) or colectomy[3,4]. Daily clinical follow up of these patients by both an expert surgeon and physician is required from that stage on and colectomy should be considered if the clinical condition of a patient worsens. Addition of rectal hydrocortisone drips or mesalamine enemas can be considered at this stage particularly in patients with symptoms secondary to left sided colitis.
THERAPY OPTIONS FOR PATIENTS FAILING IV CORTICOSTEROIDS
When patients fail three to five days of IV cortico-steroids at adequate doses and continue to report frequent bloody diarrhea with fever or high CRP levels, they should be considered for surgical colectomy or rescue medical treatment[3,4]. Complications such as toxic megacolon or uncontrolled bleeding should favor the decision towards surgical intervention.
Intravenous cyclosporine has been shown to be an effective rescue therapy for severe UC attacks in two controlled trials[6,7]. In the trial by Lichtiger et al, 9 out of 11 IV 4 mg/kg cyclosporine treated patients avoided colectomy versus none of the 9 placebo treated patients. Data from one mono center controlled trial in 73 patients indicate that 2 mg/kg per day IV cyclosporine initial treatment may prove as effective for severe attacks of UC, although not all of these patients were failing intravenous corticosteroids[8]. When results from controlled and non-controlled trials are pooled 76 to 85 percent of patients will respond to IV cyclosporine and avoid colectomy short term. Before the initiation of IV cyclosporine hypomagnesemia and hypocholesterolemia should be corrected to decrease the risk neurologic toxicity. After an initial dose of 2 mg/kg, daily cyclosporine doses should be adjusted to achieve therapeutic blood levels from day two onwards. Therapeutic ranges for cyclosporine blood levels may vary based on the assay used. The median time to response for IV cyclosporine is four to five days and in patients responding, initiation of oral cyclosporine therapy at 5-8 mg/kg divided in two doses should be considered along with gradual steroid tapering and initiation of azathioprine or 6-mercaptopurine. While patients are on a triple immunosuppressive regimen prophylaxis against Pneumocystis carinii pneumonia should be given and alertness for opportunistic infections in general should be high. Cyclosporine use in UC has been associated with mortality and most of the fatalities were due to opportunistic infections[9]. Other complications of cyclosporine therapy include nephrotoxicity, tremor and convulsions, hypertension, gingival hyperplasia and hypertrichosis. Rare cases of anaphylaxis are contributed to the solvent in Sandimmun, the commercially available formulation of cyclosporine, and occurrence of anaphylaxis allows treatment with oral cyclosporine.
Following initial response to cyclosporine for fulminant UC about 50 percent of patients avoid colectomy at three years[9-12]. Lower colectomy free rates have been recently reported with follow up extending to seven years[11]. The patient population already failing adequate courses of azathioprine or 6-MP is most prone to colectomy following initial response to cyclosporine[10,11].
Tacrolimus an oral cyclosporine can be considered to treat severe attacks of ulcerative colitis but only retrospective uncontrolled data are available[13-15].
INFLIXIMAB
The efficacy of infliximab in the setting of severe UC not responding to therapy with intravenous steroids has been demonstrated recently in a small placebo controlled trial. Significantly more patients treated with placebo (14/21) required surgical colectomy by three months as compared to those treated with a single dose of infliximab 5 mg/kg IV (7/24)[16]. Open label experience in patients with severe UC attacks has been inconsistent[17,18]. In a recent publication from the colorectal surgery group at the Mayo Clinic, Rochester, MN, an increased risk of infectious postoperative complications was found in a group of infliximab treated patients as compared to controls[19]. It should be noted however, that disease severity, use of immunosuppressives and IV steroids was higher in the infliximab group. Other retrospective cohorts and the controlled Scandinavian trial have not confirmed this increased complication risk. However, preliminary results from a cohort of patients treated at the Mount Sinai hospital in New York suggest that patients receiving infliximab followed by cyclosporine or vice versa have a substantial risk of serious adverse events including mortality[20]. Data on long term avoidance of colectomy with infliximab are as of yet not available, but there is no indication that infliximab would increase surgical complications.
SURGICAL COLECTOMY
Surgical proctocolectomy with ileo-anal pouch anastomosis is a valid option for patients with moderate to severe UC failing medical therapy. Patients should be counseled about the option of surgery, short term complication and long term outcomes of pouch surgery, early in the course of a severe flare of UC. Also from the first day of hospitalization the surgical team should be involved in the management of the patient with fulminant UC.
EXPERT OPINION
Patients with severe attacks of UC should be hospitalized and closely monitored. After failing three to five days of intravenous corticosteroids, patients should be considered for intravenous cyclosporine (2 mg/kg per day), for infliximab (5 mg/kg IV) or for surgical colectomy. Cyclosporine is most useful as a bridge to the effect of azathioprine or 6-MP and should be considered particularly in this setting. Long term colectomy free survival rates after initial response to cyclosporine are far from optimal and we have no long term data with infliximab yet. However, in patients with a dramatic response to any of the two immune therapies a delayed elective colectomy later in the disease course may be a noble goal per se. In patients failing IV steroids, he risk of, even fatal, serious infections with cyclosporine is clearly increased and also patients responding to infliximab should be closely monitored for opportunistic infections. Finally, only a head to head comparison of cyclosporine and infliximab in a prospective trial will be able to conclusively guide us in immediate decision making (Figure 2).
S- Editor Xiao LL E- Editor Yin DH