INTRODUCTION
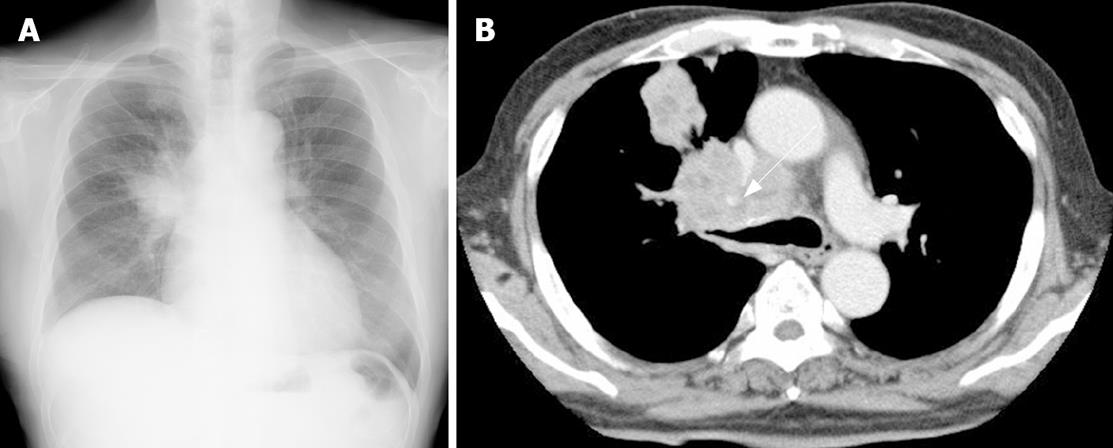
Figure 1 A: Chest X-ray revealed a large abnormal shadow in the right upper lobe; B: A computed tomography (CT) of the chest demonstrated a large lung tumor in the right upper lobe obstructing the right upper bronchus.
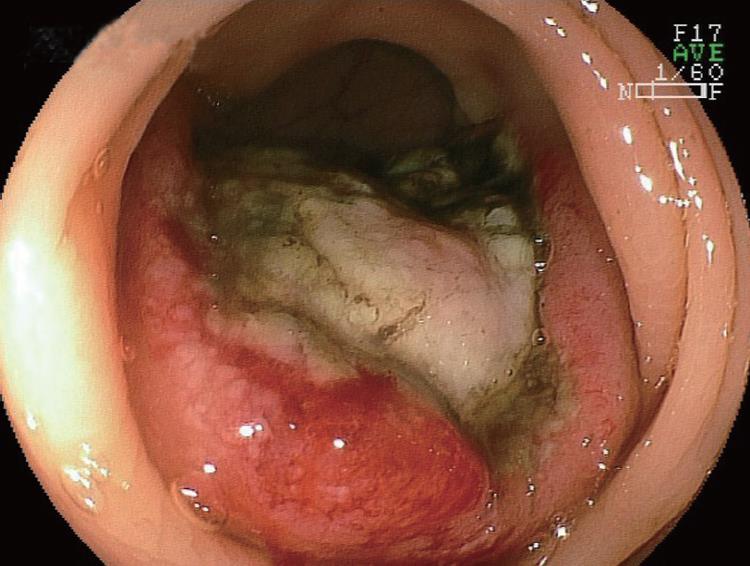
Figure 2 Endoscopic appearance of the descending colon.
A large protruding lesion with central ulceration, about 40 mm in diameter, was seen.
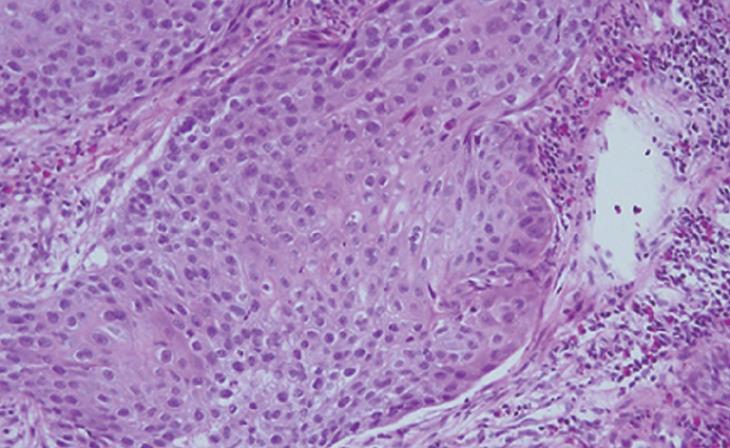
Figure 3 Histological examination of the biopsy specimen obtained from the colonic protruding lesion revealed tumor cells diagnosed as SCC (× 50).
Primary lung cancer is a common neoplasm, and frequently metastasizes to internal organs such as the lung, liver and adrenal gland; however, it is relatively rare for lung cancer to metastasize to the gastrointestinal (GI) tract. Colonic metastasis from primary carcinoma of the lung has rarely been described. Clinically, patients may present with symptoms of colonic obstruction, lower GI bleeding, bowel perforation, or GI fistula[1-4]. Herein, we describe a rare case of metastatic colonic squamous cell carcinoma (SCC) from the lung.
CASE REPORT
A 74-year-old man presented with the symptom of shoulder pain. His chest X-ray revealed an abnormal shadow in the right upper lobe (Figure 1A). He was in good health with no specific family or past medical history. His body temperature was 36.7°C, blood pressure was 148/82 mmHg, radial pulse rate was 72 beats/min and regular. He had anemia, but no jaundice. Neurological examination revealed no abnormal findings or lymphadenopathy. Abdominal palpation revealed tenderness in the left lower quadrant. Laboratory tests showed a red blood cell count of 318 × 104/μL [normal range (NR), 430-570 × 104/μL], a white blood cell count of 7600 /μL, and a platelet count of 30.8 × 104/μL, and a hemoglobin concentration of 8.9 g/dL (NR, 14-18 g/dL). Liver function tests were normal except for lactate dehydrogenase (LDH) of 340 IU/L (NR, 106-211 IU/L). A test for C reactive protein revealed a level of 0.8 mg/dL (NR, < 0.5 mg/dL). Renal function tests showed that blood urea nitrogen and creatinine were normal. Computed tomography (CT) of the chest demonstrated a large lung tumor in the right upper lobe obstructing the right upper bronchus (Figure 1B). Bronchoscopy revealed an easy-bleeding tumor in the right upper bronchus. Poorly differentiated SCC was diagnosed by punch biopsy.
Colonoscopy revealed a large protruding lesion with central ulceration in the descending colon (Figure 2). This finding suggested a clinical diagnosis of metastatic colonic tumor. Biopsy specimens obtained from the lesion showed SCC (Figure 3). Based on these findings, the patient was diagnosed with metastatic colonic SCC from primary lung cancer. Subsequent positron emission tomography (PET) with radiolabeled-18 fluorine fluorodeoxyglucose (FDG) imaging revealed an abnormal lesion in the descending colon. The patient underwent chemotherapy with an infusion of cisplatin 130 mg i.v. day 1, and docetaxel hydrate 100 mg i.v. day 1, repeated every 4 wk, followed by 4 courses of chemotherapy. The primary lesion shrank by less than 10% and was judged to be “Partial Response” (PR) after 3 courses of treatment. The patient still lived 23 wk after the diagnosis of metastatic colonic SCC.
DISCUSSION
GI metastasis from lung cancer is considered to be rare, although there is about 4.7%-14% prevalence at autopsy[5-7]. A recent report described by Kim et al[8] revealed that GI metastases were detected in 10 (0.19%) of 5239 lung cancer patients. In an autopsy study from Japan, the rate of GI tract metastasis, excluding the esophagus, was 1.8% and the colonic metastasis rate was only 0.5%[6]. The histological type of lung cancer that causes colonic metastasis varies according to different studies. The most common types were large cell or SCC[5,9,10]. We believe that it is hard to pinpoint the type of primary lung cancer causing colon metastasis because of the small number of cases. Reviewing the English literature, there are several reports on colonic metastasis[11-14]. Patients with GI metastasis of lung cancer are often asymptomatic, as in the present case. Yang et al[14] reported that the clinical prevalence of symptomatic GI metastasis of lung cancer is 1.77% (6/339). Habesoglu et al described that about 1/3 of colonic metastases from lung cancer are asymptomatic and the diagnosis is made at autopsy[4]. The most common symptoms are abdominal pain, nausea, vomiting, anemia, and weight loss[1,5]. Other symptoms of colonic obstruction, lower GI bleeding, bowel perforation, or GI fistula may occur[1-4]. These findings generally present after the diagnosis of primary disease but can occur synchronously or before diagnosis of the primary lesion[1,4,10].
Lung cancer with intestinal metastasis has been reported to have a poor prognosis of less than 16 wk in several studies[4,6,12,14]; however, because of advanced improvement in chemotherapy, supportive care for lung cancer, and extending life expectancy, we may come across an increasing number of GI metastasis in the future. Thus, we should pay attention to GI metastatic signs such as GI bleeding, abdominal pain, nausea, vomiting, or less commonly, ileus. Development of GI symptoms after chemotherapy should be carefully managed in patients with GI metastasis because of the possibility of chemotherapy-induced perforation. The present patient underwent colonoscopy for further evaluation of a positive fecal occult blood test, and a metastatic colonic lesion was detected before chemotherapy. He has been receiving chemotherapy without chemotherapy-induced perforation or abdominal symptoms. If we aggressively examine lung cancer patients with a positive fecal occult blood test by colonoscopy, more latent patients with metastatic colonic tumor from the lung might be discovered in the future.
Recently, PET-FDG imaging has become useful to diagnose the extent of GI metastasis[13]. Cases of small intestinal[15] and large intestinal metastasis[13] from lung cancer have been reported. In the present case, we could also detect colonic metastatic lesions with PET-FDG; however, the definite role of PET-FDG in the diagnosis of GI metastasis from primary lung cancer is still controversial because of the few cases and lack of clinical data. To clarify the usefulness of PET-FDG for the diagnosis of GI metastasis from lung cancer, we should accumulate and analyze more cases of GI metastasis from primary lung cancer.
In conclusion, we reported a rare case of metastatic colonic SCC from the lung with a positive fecal occult blood test. It is necessary to be aware that primary SCC of the lung may cause colonic metastasis, although lung SCC rarely causes colonic metastasis.