Published online Jan 21, 2008. doi: 10.3748/wjg.14.469
Revised: October 13, 2007
Published online: January 21, 2008
AIM: To compare the results from computed tomography (CT) colonography with conventional colonoscopy in symptomatic patients referred for colonoscopy.
METHODS: The study included 227 adult outpatients, mean age 60 years, with appropriate indications for colonoscopy. CT colonography and colonoscopy were performed on the same day in a metropolitan teaching hospital. Colonoscopists were initially blinded to the results of CT colonography but there was segmental unblinding during the procedure. The primary outcome measures were the sensitivity and specificity of CT colonography for the identification of polyps seen at colonoscopy (i.e. analysis by polyp). Secondary outcome measures included an analysis by patient, extracolonic findings at CT colonography, adverse events with both procedures and patient acceptance and preference.
RESULTS: Twenty-five patients (11%) were excluded from the analysis because of incomplete colonoscopy or poor bowel preparation that affected either CT colonography, colonoscopy or both procedures. Polyps and masses (usually cancers) were detected at colonoscopy and CT colonography in 35% and 42% of patients, respectively. Of nine patients with a final diagnosis of cancer, eight (89%) were identified by CT colonography as masses (5) or polyps (3). For polyps analyzed according to polyp, the overall sensitivity of CT colonography was 50% (95% CI, 39%-61%) but this increased to 71% (95% CI, 52%-85%) for polyps ≥ 6 mm in size. Similarly, specificity for all polyps was 48% (95% CI, 39%-58%) increasing to 67% (95% CI, 56%-76%) for polyps ≥ 6 mm. Adverse events were uncommon but included one colonic perforation at colonoscopy. Patient acceptance was high for both procedures but preference favoured CT colonography.
CONCLUSION: Although CT colonography was more sensitive in this study than in some previous studies, the procedure is not yet sensitive enough for widespread application in symptomatic patients.
- Citation: Roberts-Thomson IC, Tucker GR, Hewett PJ, Cheung P, Sebben RA, Khoo EW, Marker JD, Clapton WK. Single-center study comparing computed tomography colonography with conventional colonoscopy. World J Gastroenterol 2008; 14(3): 469-473
- URL: https://www.wjgnet.com/1007-9327/full/v14/i3/469.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.469
CT colonography is a newer radiological procedure that might be suitable for screening for colorectal lesions in symptomatic and asymptomatic individuals[1–6]. An obvious consideration is the sensitivity, specificity and accuracy of the investigation in different patient populations. A second consideration is the frequency of colorectal abnormalities on CT colonography that will require subsequent colono-scopy. Ideally, this percentage should be relatively low. Yet a third consideration is the cost of the procedure in money and time and the frequency of minor and more serious complications.
In previous studies that have compared CT colonography with colonoscopy, the sensitivity, specificity and accuracy of CT colonography has shown substantial variation. In one large screening study in asymptomatic adults, CT colonography had a similar sensitivity to colonoscopy for the detection of polyps greater than 6 mm in diameter[7]. In contrast, studies in symptomatic patients have shown a sensitivity for the detection of cancers of approximately 75% and lower sensitivities for the detection of polyps[89]. This variation may reflect differences in bowel preparation, colonic distension, CT scanners, collimation, software, scan evaluation and use of fecal tagging[10–13]. In this study, the comparison of CT colonography with colonoscopy included the routine use of hyoscine butylbromide (Buscopan) during CT colonography, unblinding of the results of CT colonography during colonoscopy and repeat colonoscopy for discrepant findings.
The study included 227 patients with appropriate indications for colonoscopy. Symptoms included rectal bleeding in 77 patients, abdominal pain in 56 and a change in bowel habit in 41. In addition, some patients had a family history of colorectal cancer (51), previous colonic polyps (43) and a recent positive fecal occult blood test (30). Exclusion criteria included inflammatory bowel disease and major coexisting medical disorders. Patients had a mean age of 60 years with an age range of 25 to 85 years. There were similar numbers of men (51%) and women (49%). All patients gave informed written consent and the study was approved by the local institutional Ethics Committee in 2003.
CT colonography and colonoscopy were performed on the same day. The type of bowel preparation was determined by the colonoscopist but most patients had Picolax, Colonlytely or both preparations. CT colonography was performed with a Toshiba multislice helical CT scanner with 2 mm collimation that was reconstructed into intervals of 1.0-1.5 mm. Colonic distension was achieved by insufflation of carbon dioxide and the use of intravenous Buscopan (20 mg). Patients were scanned in both supine and prone positions during a single breath hold (average scanning time, 25 s). With this technique, the radiation dose is lower than that of a barium enema X-ray. Images obtained with a Compaq® PC using ColonScreen (Voxcar Ltd., Edinburgh) were read in 2-dimensional format with use of a targeted 3-dimensional format when necessary. The CT images were reported by one of three radiologists within 60 min of completion of the scan. All had received previous training in CT colonography and had been reporting CT colonography on a routine basis prior to the study. The adequacy of the bowel preparation was recorded and the presence and size of polyps and masses were reported for eight segments (caecum, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon and rectum).
Colonoscopy was performed by a consultant gastroenterologist or colorectal surgeon. Patients were sedated with intravenous fentanyl and midazolam, sometimes supplemented with propofol. The colonoscope was passed to the caecum and then slowly withdrawn to the splenic flexure. At that point, CT colonography findings in the right colon were made available to the colonoscopist and colonoscopy was repeated if there were discrepant results. This also applied for CT colonography findings in the left colon after withdrawal of the colonoscope to the rectum. Masses and polyps detected at colonoscopy were reported in eight segments as above.
The quality of the bowel preparation was recorded on a scale of 1-5 using the system of Yee et al[14]. Patient discomfort with both CT colonography and colonoscopy were assessed by a questionnaire soon after CT colonography and during recovery after colonoscopy. Patients also completed a similar questionnaire 1 wk after the procedures that included a question on preference for CT colonography or colonoscopy. All adverse events were recorded.
Comparisons of CT colonography with colonoscopy were analyzed according to polyp and according to patient using Stata Version 9. In the more important analysis according to polyp, confidence intervals were produced using logistic regression and reflect an allowance for clustering of polyps within patients. Polyps were judged to be identical if they were located in the same or adjacent segments and if they were of similar size (± 50%). In the analysis according to patient, exact confidence intervals were calculated by the Stata contributed program “diagt”. Patients with at least one polyp identified by colonoscopy were a true positive if they had at least one polyp at CT colonography. It was not necessary for the lesions to be assessed as identical.
CT colonography was compared with colonoscopy in 202 of 227 patients. Twenty-five patients (11%) were excluded from the analysis because of incomplete colonoscopy or poor bowel preparation that largely affected CT colonography. Polyps and masses were detected at CT colonography and colonoscopy in 42% and 35% of patients, respectively.
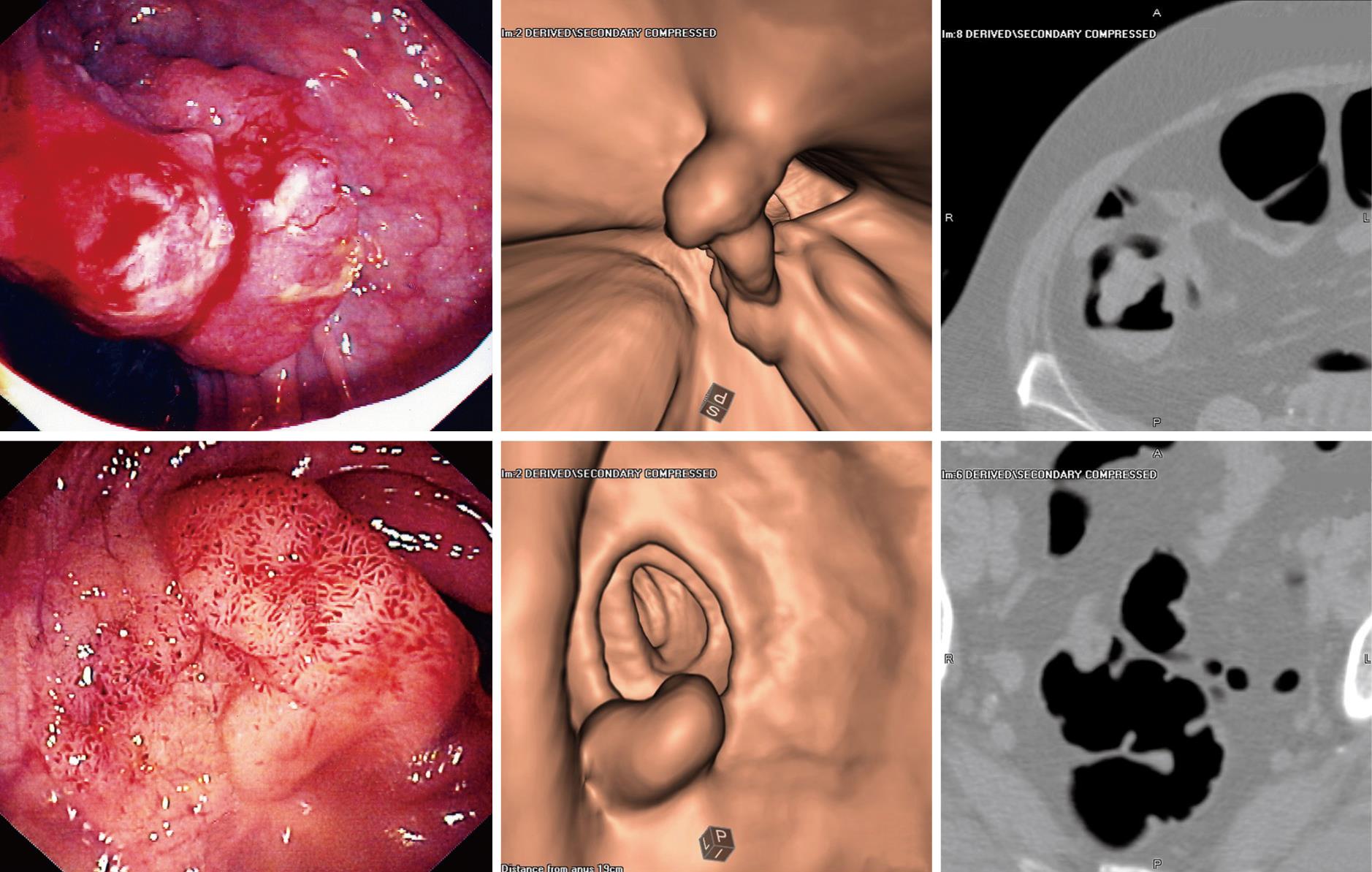
Of the 9 patients with a final diagnosis of cancer, 8 were diagnosed at colonoscopy and confirmed by biopsy while 1 patient had cancer within a polyp that was diagnosed histologically. Cancers were located in the sigmoid colon (3), rectum (3), ascending colon (2) and splenic flexure (1). All of these lesions were seen at CT colonography but only 5 were considered as probable cancers. The remaining lesions were interpreted as polyps (3) and fecal material (1). Three additional patients were diagnosed with probable cancer at CT colonography but only 1 had a corresponding polyp at colonoscopy. Polyps and cancers detected at both CT colonography and colonoscopy are shown in Figure 1.
At colonoscopy, 163 polyps were detected in 69 patients. The most common sites were the sigmoid colon (30%), rectum (27%), transverse colon (22%) and ascending colon (12%). Histologically, the majority of polyps were adenomatous (67%) while the remainder were hyperplastic, serrated or unspecified. In the analysis according to polyp, the sensitivity, specificity and accuracy of CT colonography for the detection of polyps of various sizes is shown in Table 1. The sensitivity for all polyps was 50% but this increased to 71% for polyps ≥ 6 mm in size. In the analysis according to patient, CT colonography had an overall sensitivity, specificity and accuracy of 62% (95% CI, 50%-74%), 76% (95% CI, 67%-83%), and 71% (95% CI, 64%-77%), respectively. For polyps ≥ 6 mm analyzed by patient, sensitivity, specificity and accuracy were 78% (95% CI, 58%-91%), 82% (95% CI, 76%-88%) and 82% (95% CI, 76%-87%). In relation to the sensitivity of colonoscopy, one polyp was detected by CT colonography that was missed at the initial colonoscopy but detected by repeat colonoscopy.
| Polyp size | n | Sensitivity | Specificity | Accuracy |
| < 6 mm | 125 | 42 (30-55) | 63 (52-73) | 54 (46-62) |
| 6-10 mm | 27 | 78 (52-92) | 75 (65-83) | 75 (66-83) |
| > 10 mm | 11 | 62 (39-81) | 86 (77-92) | 82 (73-89) |
| All polyps | 163 | 50 (39-61) | 48 (39-58) | 49 (42-56) |
| ≥ 6 mm | 38 | 71 (52-85) | 67 (56-76) | 68 (59-76) |
Data on extracolonic findings were available in 225 of 227 patients (99%). One patient had a renal mass and was subsequently diagnosed with renal cell cancer. Other findings of potential clinical significance included renal stones (7%), gallbladder stones (6%), adrenal masses (4%), ovarian cysts (3%), non-cystic liver lesions (2%), small aortic aneurysms (2%), lung nodules (1%) and calcific chronic pancreatitis (1%).
Only 33% of patients had a clean bowel (grade 1) while 62% had “pools of liquid” (grade 2) and 5% had “solid and liquid” or “collections of solid feces” (grades 3 and 4). Patients categorized as “impossible” (grade 5) were ex-cluded from the study.
These were reported by 4 patients after CT colonography and included nausea (2), dizziness (1) and significant abdominal pain (1). Adverse events after colonoscopy included rectal bleeding (1) and moderate or severe abdominal pain (2). One of these patients was subsequently diagnosed with colonic perforation and treated by resection of the sigmoid colon. There were no postoperative complications. Other recorded complications during colonoscopy included hypoxia (1), hypertension (1) and bradycardia (1).
Selected results from a questionnaire administered 1 wk after the procedures are included in this report. The questionnaire was completed by 195 of 202 patients (96%). The experience of CT colonography and colonoscopy was “better than expected” or “as expected” in 84% and 94% of patients, respectively. Overall, 87% of patients were “very satisfied” or “satisfied” with CT colonography while 90% were “very satisfied” or “satisfied” with colonoscopy. Furthermore, 89% of patients indicated that they “definitely would” or were “most likely” to have repeat CT colonography compared to 96% for colonoscopy. These differences were not statistically significant. However, when asked to choose between CT colonography and colonoscopy for a repeat procedure, 61% chose CT colonography and 39% chose colonoscopy (P = 0.005, Chi-square test).
CT colonography, also called virtual colonoscopy, is an evolving technology that may have a role in screening for colorectal polyps and cancer. However, using colonoscopy as the gold standard, concordance between the two investigations has varied widely in different studies. In relation to the patient population, better results have been achieved in screening studies in asymptomatic individuals than in patients with symptoms. This may reflect the younger age and better health of asymptomatic individuals who are more able or more motivated to comply with bowel preparation procedures. In any event, the quality of the bowel preparation is more important for CT colonography than for colonoscopy. In the present study, the adequacy of the bowel preparation was recorded by the reporting radiologist. Only 33% of patients had a “clean bowel” while the remainder had either “pools of liquid” (62%) or “solid and liquid” (5%). Whether bowel images can be improved by modified preparation protocols[15] or by “electronic cleansing”[16] remains unclear. Intravenous Buscopan is not routinely used during CT colonography but does enhance colonic distension[17].
Other factors that may contribute to variable results from CT colonography include the type and settings of CT scanners, the use of fecal tagging, the mode of imaging and the experience of the reporting radiologist. In one meta-analysis[10], better results were achieved with scanners with multiple detectors, thinner collimation and the standard use of three-dimensional (“fly-through”) technology. Fecal tagging using oral contrast did not appear to be a relevant factor and has the potential to impair the quality of colonoscopy. When images are reported by different radiologists, variation has ranged from “minimal”[7] to “substantial”[18], apparently independent of previous experience with the technique. There are also potential biases in comparative studies of this type with over-reporting in the investigation under study, specifically CT colonography.
The experience of both CT colonography and colonoscopy was widely accepted by patients. Although responses to specific questions about each technique showed a trend in favour of colonoscopy, more patients chose CT colonography when given a choice between the two procedures. These responses can be influenced by the structure of the questions but might also reflect real concerns about sedation, potential complications and the degree of “invasiveness”. In this study, complications were uncommon but one patient had a colonic perforation that required surgery. This complication has an overall frequency of approximately 1 in 1000 colonoscopies[1920] but can also occur after CT colonography, perhaps with a frequency of 1 in 1700 procedures[21].
In this study, CT colonography was more sensitive than in previous studies in symptomatic patients[89]. For example, CT colonography identified cancers as either masses or polyps in 8 of 9 patients (89%) in this study and in 6 of 8 (75%)[8] and 7 of 9 (78%)[9] in previous studies. For polyps analyzed by polyp, the overall sensitivity for detection of polyps was 50% in this study increasing to 71% for polyps 6 mm in size or greater. In previous studies, sensitivities for polyp detection (≥ 6 mm) were reported as 32%[8] and 47%[9]. The possibility that inaccurate localisation of polyps at colonoscopy contributed to low sensitivity rates seemed unlikely as sensitivities for polyps ≥ 6 mm analyzed by patient were only marginally higher (78%) than those analyzed by polyp (71%).
Criteria for the introduction of new technologies into clinical practice are difficult to establish. For example, issues such as sensitivity and specificity need to be considered in relation to direct and indirect costs, complications and the proportion of patients who will be referred for further investigation. In the present study, CT colonography identified polyps or masses in 42% of patients. This is not a cost-effective option if all patients with abnormalities are referred for colonoscopy[22]. However, CT colonography becomes increasingly cost-effective if colonoscopy is restricted to lesions that are ≥ 6 mm or ≥ 10 mm in size. Such recommendations, if introduced, would invite a new series of questions related to the frequency of repeat scans and the mutagenic effects of accumulating doses of radiation[23–25]. Although small polyps have a low frequency of features of advanced neoplasia, there is only limited data on the natural history of small polyps and the identification of those polyps that will eventually evolve into cancer[726].
Although CT colonography is not yet ready for widespread clinical application, it is likely that results will improve with better bowel preparation, technical developments and increasing familiarity with the technique. Results from this study highlight the importance of bowel preparation although, in the future, it may be possible to reliably differentiate fecal material from polyps using fecal tagging[10], “electronic cleansing” of colonic fluid[16] or contrast-enhanced studies[27]. Other helpful developments may also include new fecal subtraction algorithms[28], workstation modifications to facilitate polyp detection[29], improved software and new training programs for radiologists[30].
It is not yet clear whether computed tomography (CT) colonography will be widely adopted for the detection of colonic polyps and cancer. Current issues include the sensitivity and specificity of the investigation, direct and indirect costs and the longer-term effects of radiation.
This study indicates that residual liquid and solid material after bowel preparation limits the accuracy of the procedure. Whether this can be overcome by modified laxative preparations, fecal tagging or “electronic” bowel cleansing remains unclear.
In this study in symptomatic patients, CT colonography was more sensitive for the detection of polyps than in some previous studies. This study included the routine use of intravenous Buscopan but the study was not designed to determine whether this modification improved either sensitivity or specificity.
There is widespread interest in screening for colon cancer in symptomatic and asymptomatic individuals. Colonography, either using CT or magnetic resonance imaging, may play a central role if there are further improvements in sensitivity and specificity.
The paper by Roberts-Thomson IC et al is interesting. The selection of patients, sample size and the overall design of the study are fair, the results adequate to provide clinical evidence and to support valid conclusions.
| 2. | Regueiro CR. AGA Future Trends Committee report: Colorectal cancer: a qualitative review of emerging screening and diagnostic technologies. Gastroenterology. 2005;129:1083-1103. |
| 3. | Maglinte DD, Sandrasegaran K, Tann M. Advances in alimentary tract imaging. World J Gastroenterol. 2006;12:3139-3145. |
| 4. | Halligan S, Taylor SA. CT colonography: results and limitations. Eur J Radiol. 2007;61:400-408. |
| 5. | Deshpande N, Weinberg DS. The evolving role of CT colonography. Cancer Invest. 2007;25:127-133. |
| 6. | Rosman AS, Korsten MA. Meta-analysis comparing CT colonography, air contrast barium enema, and colonoscopy. Am J Med. 2007;120:203-210. |
| 7. | Pickhardt PJ, Choi JR, Hwang I, Butler JA, Puckett ML, Hildebrandt HA, Wong RK, Nugent PA, Mysliwiec PA, Schindler WR. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349:2191-2200. |
| 8. | Cotton PB, Durkalski VL, Pineau BC, Palesch YY, Mauldin PD, Hoffman B, Vining DJ, Small WC, Affronti J, Rex D. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA. 2004;291:1713-1719. |
| 9. | Rockey DC, Paulson E, Niedzwiecki D, Davis W, Bosworth HB, Sanders L, Yee J, Henderson J, Hatten P, Burdick S. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365:305-311. |
| 10. | Mulhall BP, Veerappan GR, Jackson JL. Meta-analysis: computed tomographic colonography. Ann Intern Med. 2005;142:635-650. |
| 11. | Landeras LA, Aslam R, Yee J. Virtual colonoscopy: technique and accuracy. Radiol Clin North Am. 2007;45:333-345. |
| 12. | Dachman AH, Lefere P, Gryspeerdt S, Morin M. CT colonography: visualization methods, interpretation, and pitfalls. Radiol Clin North Am. 2007;45:347-359. |
| 13. | Tolan DJ, Armstrong EM, Burling D, Taylor SA. Optimization of CT colonography technique: a practical guide. Clin Radiol. 2007;62:819-827. |
| 14. | Yee J, Akerkar GA, Hung RK, Steinauer-Gebauer AM, Wall SD, McQuaid KR. Colorectal neoplasia: performance characteristics of CT colonography for detection in 300 patients. Radiology. 2001;219:685-692. |
| 15. | Toledo TK, DiPalma JA. Review article: colon cleansing preparation for gastrointestinal procedures. Aliment Pharmacol Ther. 2001;15:605-611. |
| 16. | Pickhardt PJ, Choi JH. Electronic cleansing and stool tagging in CT colonography: advantages and pitfalls with primary three-dimensional evaluation. AJR Am J Roentgenol. 2003;181:799-805. |
| 17. | Taylor SA, Halligan S, Goh V, Morley S, Bassett P, Atkin W, Bartram CI. Optimizing colonic distention for multi-detector row CT colonography: effect of hyoscine butylbromide and rectal balloon catheter. Radiology. 2003;229:99-108. |
| 18. | Johnson CD, Harmsen WS, Wilson LA, Maccarty RL, Welch TJ, Ilstrup DM, Ahlquist DA. Prospective blinded evaluation of computed tomographic colonography for screen detection of colorectal polyps. Gastroenterology. 2003;125:311-319. |
| 19. | Dafnis G, Ekbom A, Pahlman L, Blomqvist P. Complications of diagnostic and therapeutic colonoscopy within a defined population in Sweden. Gastrointest Endosc. 2001;54:302-309. |
| 20. | Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230-236. |
| 21. | Sosna J, Blachar A, Amitai M, Barmeir E, Peled N, Goldberg SN, Bar-Ziv J. Colonic perforation at CT colonography: assessment of risk in a multicenter large cohort. Radiology. 2006;239:457-463. |
| 22. | Heitman S, Fong A, Dean S, Hilsden R, Manns B, Romagnuolo J. Cost-effectiveness study of CT colonography versus colonoscopy using decision analysis. Gastroenterology. 2004;126 Suppl 2:A202. |
| 23. | Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, Lubin JH, Preston DL, Preston RJ, Puskin JS. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA. 2003;100:13761-13766. |
| 24. | Berrington de Gonzalez A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345-351. |
| 25. | Newnham E, Hawkes E, Surender A, James SL, Gearry R, Gibson PR. Quantifying exposure to diagnostic medical radiation in patients with inflammatory bowel disease: are we contributing to malignancy? Aliment Pharmacol Ther. 2007;26:1019-1024. |
| 26. | Schoenfeld P. Small and diminutive polyps: implications for colorectal cancer screening with computed tomography colonography. Clin Gastroenterol Hepatol. 2006;4:293-295. |
| 27. | Lee SS, Park SH, Choi EK, Kim SY, Kim MJ, Lee KH, Kim YH. Colorectal polyps on portal phase contrast-enhanced CT colonography: lesion attenuation and distinction from tagged feces. AJR Am J Roentgenol. 2007;189:35-40. |
| 28. | Johnson KT, Carston MJ, Wentz RJ, Manduca A, Anderson SM, Johnson CD. Development of a cathartic-free colorectal cancer screening test using virtual colonoscopy: a feasibility study. AJR Am J Roentgenol. 2007;188:W29-W36. |
| 29. | Young BM, Fletcher JG, Paulsen SR, Booya F, Johnson CD, Johnson KT, Melton Z, Rodysill D, Mandrekar J. Polyp measurement with CT colonography: multiple-reader, multiple-workstation comparison. AJR Am J Roentgenol. 2007;188:122-129. |