Published online Jul 21, 2008. doi: 10.3748/wjg.14.4413
Revised: June 2, 2008
Accepted: June 9, 2008
Published online: July 21, 2008
Super-imposed infection with intestinal organisms can mimic a flare-up of underlying disease in patients with inflammatory bowel disease (IBD). We report a case of patient with long standing ulcerative colitis (UC), who presented with abdominal pain, diarrhea and low-grade fever after receiving systemic corticosteroids for an unrelated disorder. Despite a negative stool examination, a peripheral eosinophilia reappeared upon tapering down of a corticosteroid dose. Subsequently, duodenal biopsies showed evidence for Strongyloides, presumably acquired 20 years ago when the patient was residing in Brazil. The patient fully recovered following anti-helmintic therapy. This case underscores the importance of considering Strongyloides in the work-up of flaring-up IBD patients, even if a history of residing or traveling to endemic areas is in the distant past.
- Citation: Ben-Horin S, Barshack I, Chowers Y, Mouallem M. Flare-up of ulcerative colitis after systemic corticosteroids: A strong case for Strongyloides. World J Gastroenterol 2008; 14(27): 4413-4415
- URL: https://www.wjgnet.com/1007-9327/full/v14/i27/4413.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4413
Although exacerbation of ulcerative colitis (UC) usually poses a little diagnostic dilemma, physicians should remain cognizant to the possibility of an alternative cause for patient symptoms.
A 54-year-old practicing physician, native of Brazil who immigrated to Israel 20 years ago, was hospitalized in the Neurology Department with severe cluster headache attack, which responded to oral dexamethasone at 16 mg/d. History was also notable for left-sided UC controlled by 5-aminosalycilates (5-ASA) over the past 11 years. In the previous 2 years, the patient was lost to follow-up but reported he was in clinical remission. Two weeks after his hospital discharge from the Neurology Department, he presented again with non-bloody diarrhea, abdominal pain and muscle pain.
Upon examination a fever of 37.7°C was noted, and right abdominal tenderness was appreciated. The rest of the physical examination was unremarkable. Complete blood count showed that his white blood cell count was 8.4 K/mcl, with a normal differential count. Hemoglobin level was 14.6 g/dL. Chemistry results were all normal except for an albumin of 2.6 g/dL. Urinalysis showed leukocyturia and urine culture-yielded E.coli. Abdominal plain film showed small fluid levels.
Although the patient's abdominal pain and diarrhea suggested a possible UC flare-up, the lack of rectal bleeding, the right-sided abdominal tenderness and the muscular complaints raised the suspicion of a super-imposed infectious process in addition to a urinary tract infection. Steroid myopathy causing muscles’ pain was also considered. Prednisone was tapered to 5 mg over 4 d and ofloxacin was started, but the patients’ symptoms persisted and a fever up to 38°C was noted. Stool culture, examination for ova & parasites and C. difficile toxin assay were all negative. Following steroid tapering, an elevation of eosinophil count to 15.5% of white blood cells was noted, with an absolute count of 980/mcl. Re-inspection of the blood count obtained in the Neurology Department before initiation of dexamethasone revealed peripheral eosinophilia (1240/mcl), which went unnoticed. The patient underwent gastroduodenoscopy, which showed a hyperemic edematous duodenal wall. Colonoscopy showed edematous mucosa and punctate submucosal hemorrhages extending along the colon from the descending colon to the cecum. The rectum appeared relatively spared.
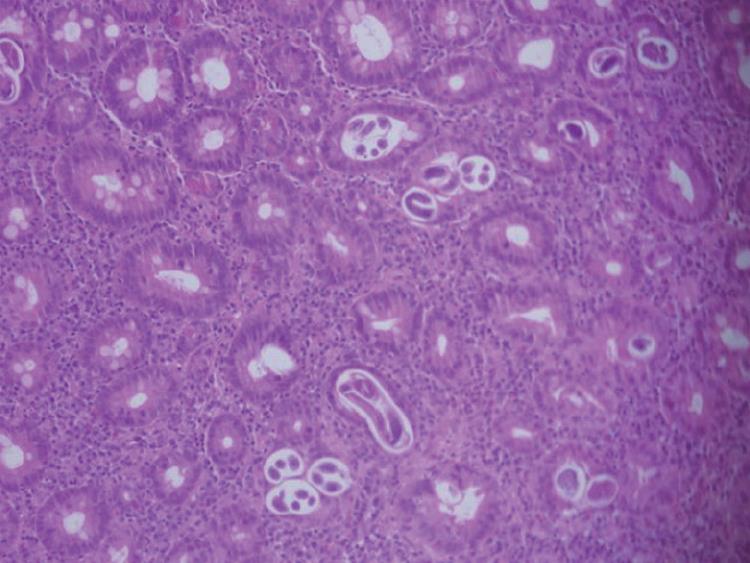
Histology from the colon revealed chronic eosino-philic inflammation and formation of eosinophilic abscesses. Duodenal histology revealed Strongyloides larva (Figure 1). CMV PCR in blood and tissue CMV immunohistochemistry were negative.
Ivermectin at a dose of 12 mg once daily was initiated with prompt resolution of all symptoms. During the 4-year follow-up, the patient was well, but experienced several mild flare-ups of UC, controlled with 5-ASA therapy. Repeat colonoscopies showed left sided colitis, and histology was compatible with UC. Two subsequent gastoduodenoscopies with biopsies did not disclose evidence of strongyloides
Strongyloides stercoralis is endemic in tropic and sub-tropic areas of the world, but has also been reported in residents of certain regions of the US and in coal miners in non-endemic areas[12]. Most cases present with pulmonary and/or upper gastrointestinal symptoms[3]. However, Strongyloides-associated colitis can occur as part of hyperinfestation following altered host immune status[45]. In this situation, larvae traveling down from the duodenum penetrate the colon wall rather than continue to be excreted in the stool[4]. The ensuing eosinophilic-predominant colitis may mimic new onset of UC[24]. Alternatively, it can emerge after corticosteroid treatment of a patient with well established UC, and can be mistaken for a refractory exacerbation[136].
The diagnosis of Strongyloides is often problematic. Stool examination is negative in 50%-70%[78] of patients. Eosinophilia was present in 84% of patients in one series[7], but in only 32% of corticosteroids-treated patients in another series[9]. Our patient had eosinophilia upon his prior admission to the Neurology Department that went unnoticed. Serology testing for Strongyloides-specific antibodies is also helpful, although not widely available. Upper endoscopy usually reveals hyperemic edematous duodenal mucosa with white villi[10] and colonoscopy may show mucosal edema, erosions and ulcerations[11], but none of these findings is specific. Duodenal aspirates and/or biopsy can assist the diagnosis, but are dependent upon worm burden and amenable to sample error[7]. Moreover, even when larvae are present in the intestinal or colonic wall, the diagnosis can be over-looked by the inexperienced or unsuspecting pathologist[112], or may be mistaken for eosinophilic gastroenteritis[13].
Strongyloides can persist in the host for his or her entire life-time[14]. Indeed, in our patient, infection was probably acquired in Brazil, twenty years prior to clinical presentation. Thus, albeit rare, the potential fatal consequences of untreated strongyloidiasis, make it imperative to consider this diagnosis in flaring inflammatory bowel disease (IBD) patients with even a distant history of residence or travel in endemic areas, or in patients failing to respond to standard therapy[15]. Eosinophilia should be excluded before initiation of immunosuppression, given the hazards of over-looking a dormant parasitic infection.
| 1. | Gutierrez Y, Bhatia P, Garbadawala ST, Dobson JR, Wallace TM, Carey TE. Strongyloides stercoralis eosinophilic granulomatous enterocolitis. Am J Surg Pathol. 1996;20:603-612. |
| 2. | de Goede E, Martens M, Van Rooy S, VanMoerkerke I. A case of systemic strongyloidiasis in an ex-coal miner with idiopathic colitis. Eur J Gastroenterol Hepatol. 1995;7:807-809. |
| 3. | Ghoshal UC, Alexender G, Ghoshal U, Tripathi S, Krishnani N. Strongyloides stercoralis infestation in a patient with severe ulcerative colitis. Indian J Med Sci. 2006;60:106-110. |
| 4. | Al Samman M, Haque S, Long JD. Strongyloidiasis colitis: a case report and review of the literature. J Clin Gastroenterol. 1999;28:77-80. |
| 5. | Concha R, Harrington W Jr, Rogers AI. Intestinal strongyloidiasis: recognition, management, and determinants of outcome. J Clin Gastroenterol. 2005;39:203-211. |
| 6. | Leung VK, Liew CT, Sung JJ. Fatal strongyloidiasis in a patient with ulcerative colitis after corticosteroid therapy. Am J Gastroenterol. 1997;92:1383-1384. |
| 7. | Boulware DR, Stauffer WM, Hendel-Paterson BR, Rocha JL, Seet RC, Summer AP, Nield LS, Supparatpinyo K, Chaiwarith R, Walker PF. Maltreatment of Strongyloides infection: case series and worldwide physicians-in-training survey. Am J Med. 2007;120:545.e1-e8. |
| 8. | Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis. 2001;33:1040-1047. |
| 9. | Fardet L, Genereau T, Poirot JL, Guidet B, Kettaneh A, Cabane J. Severe strongyloidiasis in corticosteroid-treated patients: case series and literature review. J Infect. 2007;54:18-27. |
| 10. | Kishimoto K, Hokama A, Hirata T, Ihama Y, Nakamoto M, Kinjo N, Kinjo F, Fujita J. Endoscopic and histopathological study on the duodenum of Strongyloides stercoralis hyperinfection. World J Gastroenterol. 2008;14:1768-1773. |
| 11. | Thompson BF, Fry LC, Wells CD, Olmos M, Lee DH, Lazenby AJ, Monkemuller KE. The spectrum of GI strongyloidiasis: an endoscopic-pathologic study. Gastrointest Endosc. 2004;59:906-910. |
| 12. | Berry AJ, Long EG, Smith JH, Gourley WK, Fine DP. Chronic relapsing colitis due to Strongyloides stercoralis. Am J Trop Med Hyg. 1983;32:1289-1293. |
| 13. | Corsetti M, Basilisco G, Pometta R, Allocca M, Conte D. Mistaken diagnosis of eosinophilic colitis. Ital J Gastroenterol Hepatol. 1999;31:607-609. |
| 14. | Mylonaki M, Langmead L, Pantes A, Johnson F, Rampton DS. Enteric infection in relapse of inflammatory bowel disease: importance of microbiological examination of stool. Eur J Gastroenterol Hepatol. 2004;16:775-778. |