INTRODUCTION
Biliary papillomatosis is a rare disease with less than 100 cases reported in the literature[12]. Biliary adenomatosis is a disease of advanced age and more common in males than in females. Similar to the adenoma-carcinoma sequence found in colon cancer, a progression to cholangiocarcinoma is presumed for biliary adenoma[3]. Therefore, patients with bile duct adenomatosis are at an increased risk of developing malignancies[1]. So far, resection of the involved liver segments and liver transplantation are the only established therapeutic options for patients with biliary papillomatosis[45]. Because of the advanced age and concomitant cardiovascular risk factors, many patients are neither eligible for extended liver resection nor transplantation, limiting the therapeutic options for the majority of patients with bile duct papillomatosis.
Photodynamic therapy (PDT) is a relatively new endoscopic procedure established in the local therapy for Barrett’s esophagus[6], non small-cell lung cancer[7] and newly established for the palliative treatment of malignant neoplasms of the bile duct[8–13]. After local or systemic application of a photosensitizer, the agent accumulates in neoplastic tissue while it is cleared from most other tissues within 40-60 h. Local radiation of the neoplasm with non-thermal laser activates the compound resulting in destruction of the neoplasm by a photochemical process generating oxygen radicals[11]. Effects occur with a penetration depth of 5-6 mm, depending on the physical attributes of the surrounding tissue (particle scatter, light absorption, etc.). This procedure was first reported in 1991 by Mc Coughan in the treatment of bile duct cancer[14]. In this palliative setting, PDT shows good results in terms of quality of life, relief from cholestasis and extension of lifespan[810]. Side effects include fever, abdominal pain, nausea, vomiting and insomnia though rare. Increased photosensitivity of the skin and eyes is observed and precautions should include avoidance of direct sunlight and bright indoor light. The skin should be covered and sunglasses should be worn when being outdoors.
CASE REPORT
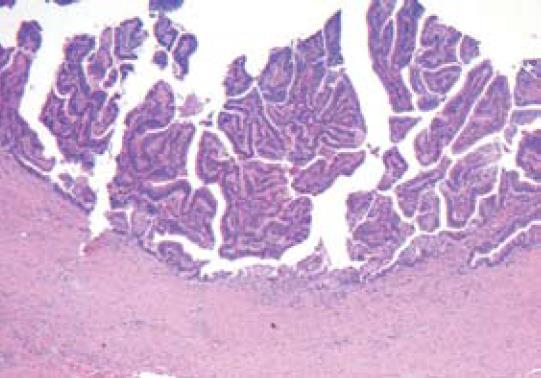
A previously healthy 65-years old male developed jaundice and right upper abdominal quadrant pain in 1996. An ERCP revealed a tumor in the common bile duct. Thus a Whipple procedure was performed. Histologically, a villous adenoma of the distal bile duct was diagnosed. The patient recovered well until he became symptomatic again in 2002. Another large adenoma was seen in a previously performed cholangioscopy of the right hepatectomy and hepatico-jejunostomy. The histological examination again revealed a villous adenoma with mild inflammation of the adjacent proximal parts of the bile duct and the surrounding liver tissue (Figure 1).
Figure 1 HE staining for samples collected at the right-sided hemihepatectomy and hepatico-jejunostomy of the left hepatic duct (× 40) showing a villous adenoma with mild inflammation of the adjacent proximal parts of the bile duct and the surrounding liver tissue but no invasive growth.
Two years later, the patient developed cholestasis again. After drainage of the left hepatic duct with a percutaneous transhepatic cholangial drainage (PTCD) catheter, a recurrent biliary adenomatosis was diagnosed via cholangioscopy. Following the Whipple-procedure, hemihepatectomy and hepatico-jejunostomy in the past, another surgical procedure was found to be of little benefit for the 72-years old patient. Thus we decided to perform a therapeutic trial of photodynamic therapy (PDT). Forty-eight hours after injection of 2 mg/kg of photosensitizer Photofrin II®, we performed laser irradiation (633 nm) of the bile duct via videocholangioscopy (Olympus) with 400 W/cm. A Yamakawa catheter was placed for drainage of the biliary tract. The patient was instructed to protect against sunlight for the following 6 wk and discharged. No side effects of the PDT procedure were seen. He recovered well and was regularly readmitted 6 mo later for a follow-up cholangioscopy.
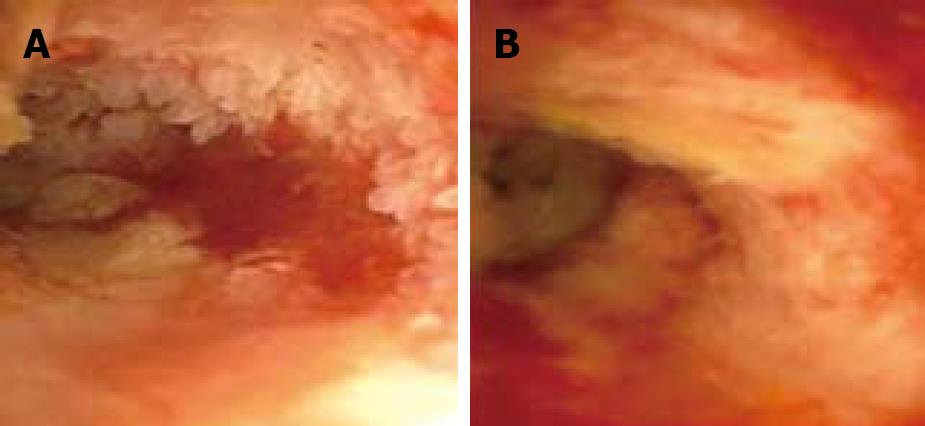
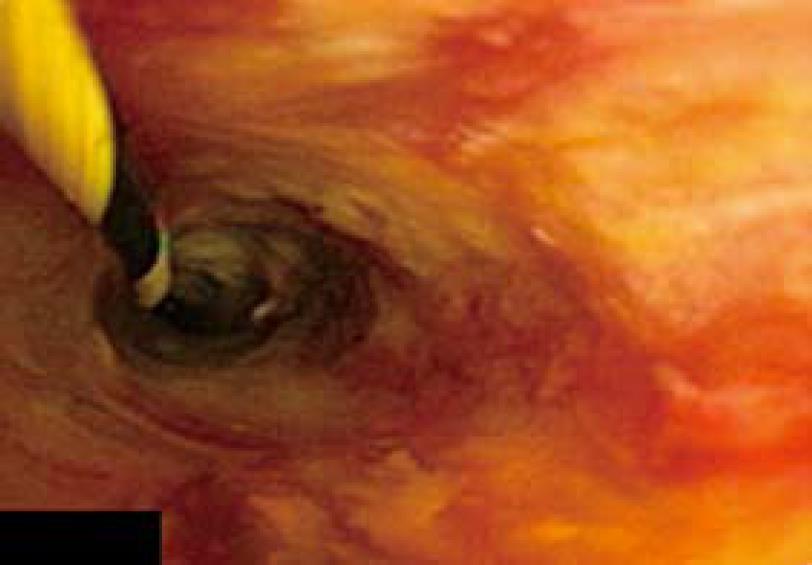
This time, the biliary papillomatosis appeared less extensive and the Yamakawa-drain was exchanged. Another PDT procedure was performed using the same protocol as in the first attempt. In June 2005, the patient was regularly readmitted for another follow-up. This time a mild recurrent papillomatosis was diagnosed and another PDT procedure was performed (Figure 2). Three months later, we repeated photodynamic therapy with only remnants of the papillomatosis seen cholangioscopically. By that time histology revealed a papillary adenoma with focal high-grade dysplasia. The patient remained asymptomatic for months. Three months after the third treatment, the bile duct epithelium appeared normal and the patient had no signs of adenomata or dysplasia, both macroscopically and histologically. Another follow-up cholangioscopy in late 2005 revealed only a small adenoma without the need for intervention (Figure 3).
Figure 2 Recurrent papillomatosis before the third course of photodynamic therapy without signs of a functional stenosis of the bile duct (A) and one month after the second course of PDT (B).
Figure 3 Cholangioscopy showing only minor adenomatosis 3 mo after the third course of PDT.
In early 2006, the patient presented with signs of end-stage liver disease accompanying portal hypertension, ascites, spontaneous bacterial peritonitis and caput medusae. The underlying liver disease was most likely secondary biliary cirrhosis, caused by chronic cholestasis in the past. In March 2006, he was admitted to hospital with severe pneumonia and decompensated liver cirrhosis. A few weeks later, the patient died of multi organ failure. By that time, he had no clinical or sonographical signs of extrahepatic cholestasis or cholangitis.
DISCUSSION
We report the first successful photodynamic therapy for biliary adenomatosis without any serious side effects. Photodynamic therapy is an established intervention in the treatment of Barret’s esophagus[6], lung cancer[7] and bile duct cancer[8]. It was reported that photodynamic therapy can improve the quality of life and the survival of such patients[8101516].
Our patient survived ten years after the diagnosis of biliary papillomatosis was established, exceeding the average survival time of biliary adenomatosis patients ranging from 28[1] to 32 mo[2]. Yeung et al[2] reviewed 78 cases of biliary papillomatosis and postulated a median survival of 28 mo after radical resection irrespective of the histological signs of dysplasia, while the median survival time was only 11 mo when no radical resection was performed. Only few cases having a survival time of more than 4 years after the diagnosis of biliary papillomatosis have been reported. In the patient presented here, the first biliary adenoma was diagnosed in 1996 and recurred in 2002, resulting in hemihepatectomy. After initiation of the PDT, the patient survived another four years with a good quality of life until admission for decompensated liver cirrhosis, a few weeks before he died. From the first manifestation of the disease he even survived 10 years.
Depending on the location and extension of the disease so far, the Whipple procedure and hemihepatectomy are the therapies of choice for biliary papillomatosis resulting in an average survival time of approximately 17 mo[217]. Extensive preoperative diagnosis is required to determine the resectability and the extent of the disease by ERCP, CT, cholangioscopy and intraoperative ultrasound studies[18]. In cases of diffuse hepatic manifestations, liver transplantation should be considered[4]. Bile duct papillomatosis is a disease of the elderly (mean age at time of diagnosis: 63 years), thus many patients would not be eligible for transplantation limiting the therapeutic options.
Apart from other local palliative procedures (i.e. stenting, drainage), few cases of local ablation have been reported[1920], most of them in the palliative setting with advanced disease plus cholangiocarcinoma were treated with a conventional laser. Data on the long term survival of these patients are lacking so far. However, PDT ablation seems to be more specific targeting dysplastic tissue with less harm to the surrounding tissue[11]. Thus, using PDT in this particular setting might improve the quality of life and prolong life expectation of this group of patients without exposing them to risky procedures. The use of PDT in this setting has not been reported in the literature so far.
Side effects of PDT include fever, abdominal pain, nausea, vomiting and insomnia though rare. Increased photosensitivity of the skin and eyes is observed and precautions should include avoidance of direct sunlight and bright indoor light[11]. In this case only minor adverse effects are reported including mild inflammatory reaction two days after the PDT and mild skin reaction. The quality of life was significantly improved with relief from cholestasis and cholangitis for months and the patient exceeded the survival rate of most other cases reported in literature[2].
In conclusion, PDT might be a therapeutic option for patients with recurrent biliary papillomatosis after resection as well as for those who are not eligible for surgery. Further studies are needed to prove the role of PDT in the treatment of biliary papillomatosis.
Peer reviewer: Yusuf Bayraktar, Professor, Department of
Gastroenterology, School of Medicine, Hacettepe University,
Ankara 06100, Turkey