INTRODUCTION
Since the successful introduction of laparoscopic colectomy by Jacobs et al[1], laparoscopic surgery, especially laparoscopic rectal surgery has been developed considerably[2–6]. Laparoscopic total mesorectal excision (TME) for rectal cancer whether hand-assisted, laparoscopy-assisted or robotic-assisted laparoscopic technique can offer advantages over open TME, such as greater comfort and an earlier return to daily activities while preserving the oncologic radicality of the procedure[7–10]. Moreover, the laparoscopy allows good exposure of the pelvic cavity because of magnification and good illumination. The laparoscope seems to facilitate pelvic dissection including identification and preservation of critical structures such as the autonomic nervous system[1112]. Laparoscopic TME for rectal cancer is feasible and safe; the short-, mid- and long-term outcomes of the operation are favorable compared with those of conventional open surgery[13–17]. However, the laparoscopic TME for rectal cancer is complicated and has some technical difficulties during operation; surgeons had to invent some methods to resolve the problem[18–22]. As ultrasonically activated scalpel (US) is able to grasp and divide tissues while sealing small vessels, the laparoscopic operation has become simpler, but the expensive medical instrument and high costs of the disposable materials can greatly increase the cost of laparoscopic TME for rectal cancer[23–25]. In order to reduce the cost of the operation, we tried to use monopolar electrocautery shovel (ES) in laparoscopic TME with anal sphincter preservation for rectal cancer, and compared it with US.
MATERIALS AND METHODS
Patients
Forty-two rectal cancer patients who were treated between June 2005 and June 2007 were chosen prospectively. The inclusion criteria are: patients with confirmed diagnosis of rectal cancer, non-emergency surgery, the tumor margin from the anal margin being more than 5 cm, no preoperative examination of liver, and other distant organ metastasis, and suitable for sphincter-saving surgery. Removal criteria are: patients whose tumor involved the bladder, uterus or pelvic metastasis, and not suitable for radical surgery. One patient in each group was excluded according to the removal criteria. The patients were randomly divided into laparoscopic US group and laparoscopic ES group.
Surgical techniques
The two groups of patients used the same method for preoperative preparation. All the procedures were performed by the same operation team. Each of them conformed to the radical treatment principles including en bloc resection, no-touch isolation technique, proximal lymph-vascular ligation, complete lymphadenectomy, wound protection, and adequate resected margin of the rectum and TME for rectal cancer.
Study parameters
The following parameters were measured prospectively in the two groups: white blood cells (WBC) in the peripheral blood before and after operation, the operative time, blood loss, postoperative pelvic drainage volume and the time of anal exhaust. The pain degree of patients after operation was assessed by visual analogue scales (VAS), “0” represents painless, and the “10” represents the most intense pain[26].
Statistical analysis
All the statistical analyses were performed using SPSS 11.5 software package. The data were expressed as mean ± SD. Student’s t test was used to analyze quantitative variables and χ2 test was used to analyze qualitative variables. P < 0.05 was considered statistically significant.
DISCUSSION
The electric power can be converted to mechanical energy by ultrasound frequency generator in US, which can generate 55.5 kHz mechanical oscillation. By the oscillation, the tissues can be cut and coagulated and vascular closure can be made. US can precisely cut and stop bleeding and produce less heat, thus not damaging the surrounding tissues because of the small thermal spread. When US produces less smog and less eschar, the operative field become more clearly. But US also has obvious drawbacks: US instrument is expensive, needs disposable material; and significantly increases costs of the laparoscopic operation[232728]. In clinical practice, we found that the laparoscopic rectal cancer operation can almost be conducted at the same anatomical space of rectum; monopolar electrocautery can also be applied in laparoscopic TME with anal sphincter preservation for rectal cancer because there is no large blood vessel in the space around the rectum.
The electric current through the tissue can produce high temperature from 100°C to 200°C because the resistance of tissues, the tissue degeneration, necrosis, drying, evaporation, carbonation, eschar, monopolar electrocautery can cut or stop bleeding[2930]. The laparoscopic surgery, according to different operations, can choose different shaped monopolar electrocautery components such as monopolar electrocautery knife, monopolar electrocautery hook, monopolar electrocautery scissors and monopolar ES. ES is particularly suitable for laparoscopic TME with anal sphincter preservation for rectal cancer. First of all, the metal tip of ES only exposes a small area, it has a complete laparoscopic vision so as to avoid injuring the tissues outside the vision during operation in the narrow pelvic space, therefore, the laparoscopic operation has become more secure. Secondly, ES with blunt tip and a flat disk shape, can be used for blunt dissection without electricity supply and sharp dissection with electricity supply, avoiding frequent exchange of surgical instruments through trocars, so it is very suitable for dissection in the space around the rectum. Finally, the relatively sharp edge of ES can be used for sharp dissection, the disk of ES can oppress the bleeding point and achieve electrocoagulation when the tissue was bleeding, it has a good hemostatic effect. During the laparoscopic operation, ES should always use electrocoagulation in order to reduce the smog and extravasate from space wound. This study showed no significant difference in the blood loss, the pelvic drainage volume, the time of anal exhaust flow with defecation, the VAS and WBC counts between the ES group and the US group, indicating that the local and systemic impact of the body due to ES had no significant difference compared with US in laparoscopic TME with anal sphincter preservation for rectal cancer.
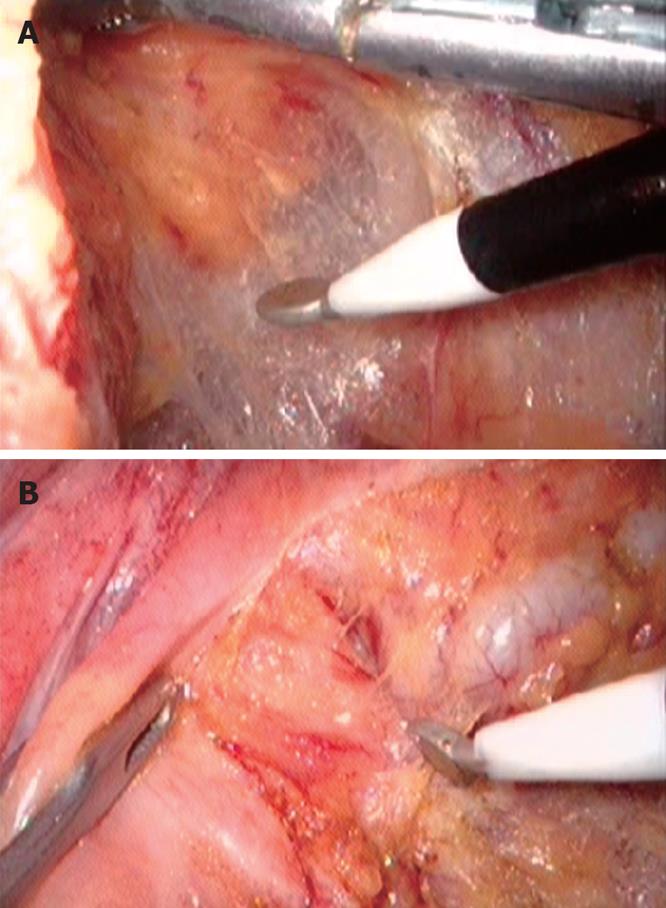
ES can produce a higher surface temperature when managing the tissues; the theoretical distance of thermal conduction is longer than that of US, which makes it easy to damage the surrounding tissues[31]. Therefore, it is particularly important for surgeons to understand how to use ES in laparoscopic TME with anal sphincter preservation for rectal cancer. The correct method is to maintain a certain tension on both sides of the separation space; let the ES slightly contact the tissue with its sharp edge, and then gently slide along the surface of tissue in order to form a large space (Figure 1A). The tissue was cut immediately into slide aside to expose deep layer tissue and the important organs in the deep layer tissue can easily be uncovered and avoid injury, thus reducing the possibility of the surrounding tissue necrosis due to “heat chemotactic effect”. At the important anatomical position, the operative speed must be slow, use “mm-class” dissection and sharp dissection in combination with blunt dissection in order to reduce bleeding and avoid injury of major blood vessels and organs (Figure 1B). There was no significant difference in postoperative complications such as anastomotic leakage and wound infection between ES group and US group in our study, indicating that ES is as safe as US in laparoscopic TME with anal sphincter preservation for rectal cancer. The operative time was almost the same between the two groups, although the cutting speed of ES was faster than that of US. On the other hand, the intraperitoneal CO2 must be exchanged regularly due to heavy smog generated by ES in order to maintain the clarity of operative vision, although it might slow the operative speed of ES in a certain extent. During operation, it must rely on the movement of metacarpophalangeal joint opening and closing repeatedly in order to control US. But in ES operation, surgeons might feel more comfortable as they can grasp ES, and rely on the push-pull movement of the arm, and the hand movement intensity might significantly decrease. Compared with US, ES has prominent advantages, including sturdiness, durability, low cost, and being suitable for laparoscopic TME with anal sphincter preservation for rectal cancer in less developed settings.
Figure 1 Intraoperative photograph.
A: Showing monopolar ES dissect the space around the rectum; B: Showing monopolar ES dissect the seminal vesicle and the rectum.
In conclusion, ES is a safe and feasible tool similar to US used in laparoscopic TME with anal sphincter preservation for rectal cancer on the basis of skillful laparoscopic technique and complete understanding of laparoscopic pelvic anatomy. Application of ES can not only reduce the operation costs but also benefit the popularization of laparoscopic operation for rectal cancer patients.
COMMENTS
Background
Since the successful introduction of laparoscopic colectomy by Jacobs et al, laparoscopic surgery, especially laparoscopic rectal surgery has been developed considerably. Compared with open operation, the laparoscopic operation has many advantages such as less pain, little blood loss, small incision, good exposure of the pelvic cavity, an earlier return to daily activities, etc. while preserving the oncologic radicality of the procedure. However, the laparoscopic operation is more difficult than the open operation. Ultrasonically activated scalpel (US) is able to grasp and divide tissues while sealing small vessels, making the laparoscopic operation simpler, whereas the expensive medical instrument and high costs of the disposable materials can greatly increase the cost of laparoscopic rectal cancer operation.
Research frontiers
It has been shown that the laparoscopic rectal cancer operation had the same short-term and long-term outcomes compared with open surgery, so how to overcome the operation difficulty and reduce the cost of laparoscopic rectal operation has become hotspots in laparoscopic surgery.
Innovations and breakthroughs
In this study, authors tried to use cheap and durable monopolar electrocautery shovel (ES) in laparoscopic operation for rectal cancer in order to reduce the cost of the laparoscopic operation, they also summarized the technique and skill of using monopolar ES, and compared with US.
Applications
ES is a safe and feasible tool similar to US used in laparoscopic TME for rectal cancer on the basis of skillful laparoscopic technique and complete understanding of laparoscopic pelvic anatomy. Application of ES can not only reduce the operation costs but also facilitate the popularization of laparoscopic operation for rectal cancer.
Terminology
US is an expensive medical instrument which can incise tissue and seal small vessels, it is often used in complicated laparoscopic operations, but it costs high for the disposable materials. So in laparoscopic operation, US can greatly increase the cost of operation. ES is often used in simple laparoscopic operations because it is not as good as US for hemostasis, but it is cheap and durable.
Peer review
This is an interesting manuscript looking into two different methods of dissecting the rectum laparoscopically. It is a good paper.