Published online May 28, 2008. doi: 10.3748/wjg.14.3259
Revised: March 31, 2008
Accepted: April 7, 2008
Published online: May 28, 2008
Small bowel diverticulosis represents an uncommon disorder (except for Meckel diverticulum) often misdiagnosed since it causes non-specific gastroin-testinal symptoms. Most of times the diagnosis is carried out in case of related complications, such as diverticulitis, hemorrhage, perforation or obstruction. Intestinal obstruction can be caused by inflammatory stenosis due to repeated episodes of diverticulitis, volvulus, intussusception or jejunal stones. Herein we report a case of multiple jejunal diverticula causing chronic gastrointestinal obstruction.
- Citation: Balducci G, Dente M, Cosenza G, Mercantini P, Salvi PF. Multiple giant diverticula of the foregut causing upper gastrointestinal obstruction. World J Gastroenterol 2008; 14(20): 3259-3261
- URL: https://www.wjgnet.com/1007-9327/full/v14/i20/3259.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3259
Multiple diverticulosis of the foregut is uncommon[1]. Although it is often asymptomatic, it can lead to severe complications, such as obstruction, hemorrhage, diverticulitis and perforation. Obstruction can be caused by inflammatory stenosis due to repeated episodes of diverticulitis, volvulus or intussusception, voluminous jejunal stones or dyskinesia of the small bowel[2–4]. We herein report a case of chronic gastrointestinal obstruction in a patient with a previous diagnosis of jejunal multiple giant diverticula.
A 49-year-old woman was admitted to our department, because of abdominal pain and vomiting together with a history of repeated episodes of obstructive gastrointestinal symptoms in the last two years.
In a previous diagnostic work out, she underwent contrast barium that showed multiple giant diverticula in the proximal small bowel tract (Figure 1).
At physical examination, she was dehydrated and her abdomen was distended but soft. A plain X-ray abdominal film showed distended small bowel loops and multiple gas-fluid levels
The actual clinical condition, the long duration of symptoms and the previous diagnosis were all considered indications for surgery.
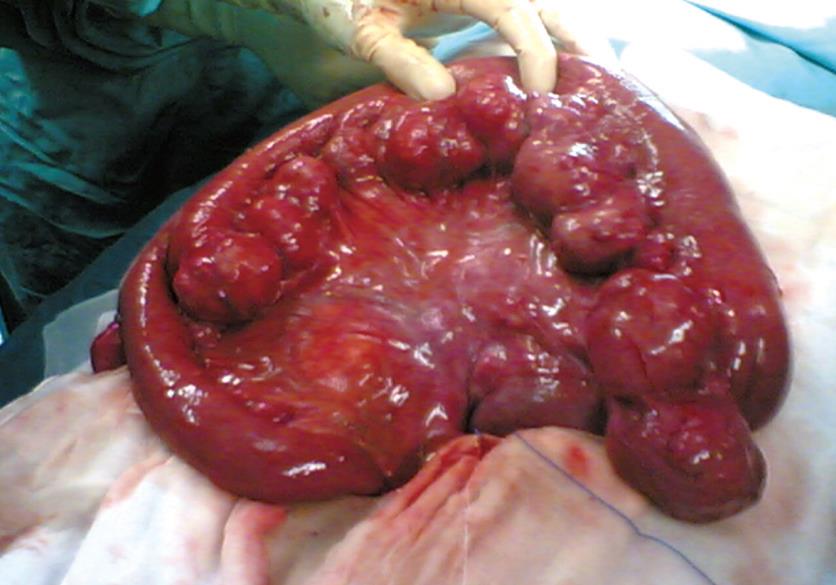
At the operation, diffuse giant diverticula were observed in the duodenum (Figure 2) and proximal jejunum so that duodenal diverticulectomy and jejunal resection were performed.
No postoperative complication was observed. During the 4-mo follow-up, the patient remained free of GI symptoms.
Jejunal diverticulosis is a rare entity with an incidence rate ranging from 0.3%-1.3% in autopsy series to 2.3% of radiographic findings[1].
Like colonic diverticula, small bowel diverticula other than Meckel’s, are false diverticula resulting from mucosal herniation at the point where blood vessels penetrate the intestinal wall. This also explains their typical location at the mesenteric side[2].
Aetiology of jejunal diverticula is still unclear since an anatomic wall defect seems not to be the only factor. Increased intraluminal pressure can play a main role as happens in case of colonic diverticulosis. Small bowel diverticula in fact can be seen in patients older than 50 years with peristaltic disorders, such as progressive systemic sclerosis, visceral myopathy and visceral neuropathies leading to increase of intraluminal pressure[3].
This condition is often misdiagnosed as it is often asymptomatic or causes minor, non-specific gastroin-testinal symptoms. Nevertheless, it could lead to severe complications, such as hemorrhage, diverticulitis, perforation and obstruction.
The small number of symptomatic patients may explain chronic post prandial abdominal pain, nausea and vomiting, borborygmi, alternating diarrhea and constipation, and weight loss, and present with anemia, steatorrhea, tenderness, and fever[14]. All these symptoms reflect inflammation, malabsorption, hemorrhage or mechanical obstruction.
Hemorrhage and perforation are the consequence of progressive ulceration in case of acute diverticulitis. While perforation is the result of progressive ulceration in case of acute diverticulitis, hemorrhage could be caused by diverticulitis with ulceration, or diverticulosis associated with trauma and irritation, or congenital arteriovenous malformations[5].
Obstruction can be caused by inflammatory stenosis due to repeated episodes of diverticulitis, volvulus or intussusception and voluminous jejunal stones. The latter seem to be caused by the intradiverticular milieu including alteration of the chemical environment and malabsorption, both of which are related to intestinal stasis and stagnant diverticula. Dyskinesia of the small bowel, in fact, causes an intraluminal stasis with bacterial overgrowth leading to deconjugation of bile acids. Deconjugated bile acid, together with choleic acid formed from bile salts and precipitate in aggregates, starts enterolith formation[67].
In our patient, intermittent occlusive symptoms were probably caused by hyperdistension of the voluminous diverticula (Figure 2), resulting in external obstruction of jejunal loops.
Asymptomatic diverticula are found only in case of radiography or surgery performed for unrelated causes.
The diagnostic work up in symptomatic patients can start with plain abdominal X-ray film that could show distension of jejunal loops and gas-fluid levels into voluminous diverticula. Upper gastrointestinal X-ray study by barium contrast clearly shows the presence of multiple diverticula.
In case of acute abdomen due to diverticular per-foration or intestinal obstruction, X-ray studies show typical signs of these conditions giving no information about the cause that will be recognized at surgery.
The treatment of choice for jejunal diverticulosis, often performed emergently, is resection of all the affected jejunum even in case of perforation or peridiverticular stenosis, in order to avoid further complications[48].
In case of obstruction due to an enterolith, some authors suggest conservative management by performing the manual breakage of all stones, intradiverticular and blocking ones, pushing their fragments to the colon[1489].
This treatment is to be discouraged because of the persisting risk of stone formation and diverticular complications.
In contrast to jejunal diverticulosis, duodenal diverticula have been treated with simple diverticulectomy. The decision to operate a duodenal diverticulum, however, should be made with great caution because postoperative complications such as fistula formation and pancreatitis are not rare given the periampullary location of many of these diverticula.
| 1. | Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13:2240-2242. |
| 2. | Hamada N, Ishizaki N, Shirahama K, Nakamura N, Murata R, Kadono J, Shimazaki T, Sameshima T, Misono T, Taira A. Multiple duodeno-jejunal diverticula causing massive intestinal bleeding. J Gastroenterol. 2000;35:159-162. |
| 3. | Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983;85:538-547. |
| 4. | Lempinen M, Salmela K, Kemppainen E. Jejunal diverticulosis: a potentially dangerous entity. Scand J Gastroenterol. 2004;39:905-909. |
| 5. | Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ. Jejunal diverticulosis and gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:412-414. |
| 6. | Crace PP, Grisham A, Kerlakian G. Jejunal diverticular disease with unborn enterolith presenting as a small bowel obstruction: a case report. Am Surg. 2007;73:703-705. |
| 7. | Hofmann AF, Mysels KJ. Bile acid solubility and precipitation in vitro and in vivo: the role of conjugation, pH, and Ca2+ ions. J Lipid Res. 1992;33:617-626. |
| 8. | Steenvoorde P, Schaardenburgh P, Viersma JH. Enterolith ileus as a complication of jejunal diverticulosis: two case reports and a review of the literature. Dig Surg. 2003;20:57-60. |
| 9. | Hayee B, Khan HN, Al-Mishlab T, McPartlin JF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883-884. |