Published online May 28, 2008. doi: 10.3748/wjg.14.3195
Revised: March 7, 2008
Accepted: March 14, 2008
Published online: May 28, 2008
AIM: To evaluate the factors that influence outcome of both non-invasive and invasive treatment of polycystic liver disease.
METHODS: Analysis of clinical files of patients with complete follow-up from July 1986 to June 2006.
RESULTS: Forty-one patients (male, 7; female, 34), 47.8 ± 11.9 years age, and 5.7 ± 6.7 years follow-up, were studied. Alkaline phosphatase (AP) elevation (15% of patients) was associated with the requirement of invasive treatment (IT, P = 0.005). IT rate was higher in symptomatic than non-symptomatic patients (65.4% vs 14.3%, P = 0.002), and in women taking hormonal replacement therapy (HRT) (P = 0.001). Cysts complications (CC) were more frequent (22%) in the symptomatic patients group (P = 0.023). Patients with body mass index (BMI) > 25 (59%) had a trend to complications after IT (P = 0.075). Abdominal pain was the most common symptom (56%) and indication for IT (78%). Nineteen patients (46%) required a first IT: 12 open fenestration (OF), 4 laparoscopic fenestration (LF) and 3 fenestration with hepatic resection (FHR). Three required a second IT, and one required a third procedure. Complications due to first IT were found in 32% (OF 16.7%, LF 25%, FHR 66.7%), and in the second IT in 66.7% (OF 100%). Follow-up mortality rate was 0.
CONCLUSION: Presence of symptoms, elevated AP, and CC are associated with IT requirement. HRT is associated with presence of symptoms and IT requirement. Patients with BMI > 25 have a trend be susceptible to IT complications. The proportions of complications are higher in FHR and second IT groups. RS is more frequent after OF.
- Citation: Barahona-Garrido J, Camacho-Escobedo J, Cerda-Contreras E, Hernández-Calleros J, Yamamoto-Furusho JK, Torre A, Uribe M. Factors that influence outcome in non-invasive and invasive treatment in polycystic liver disease patients. World J Gastroenterol 2008; 14(20): 3195-3200
- URL: https://www.wjgnet.com/1007-9327/full/v14/i20/3195.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.3195
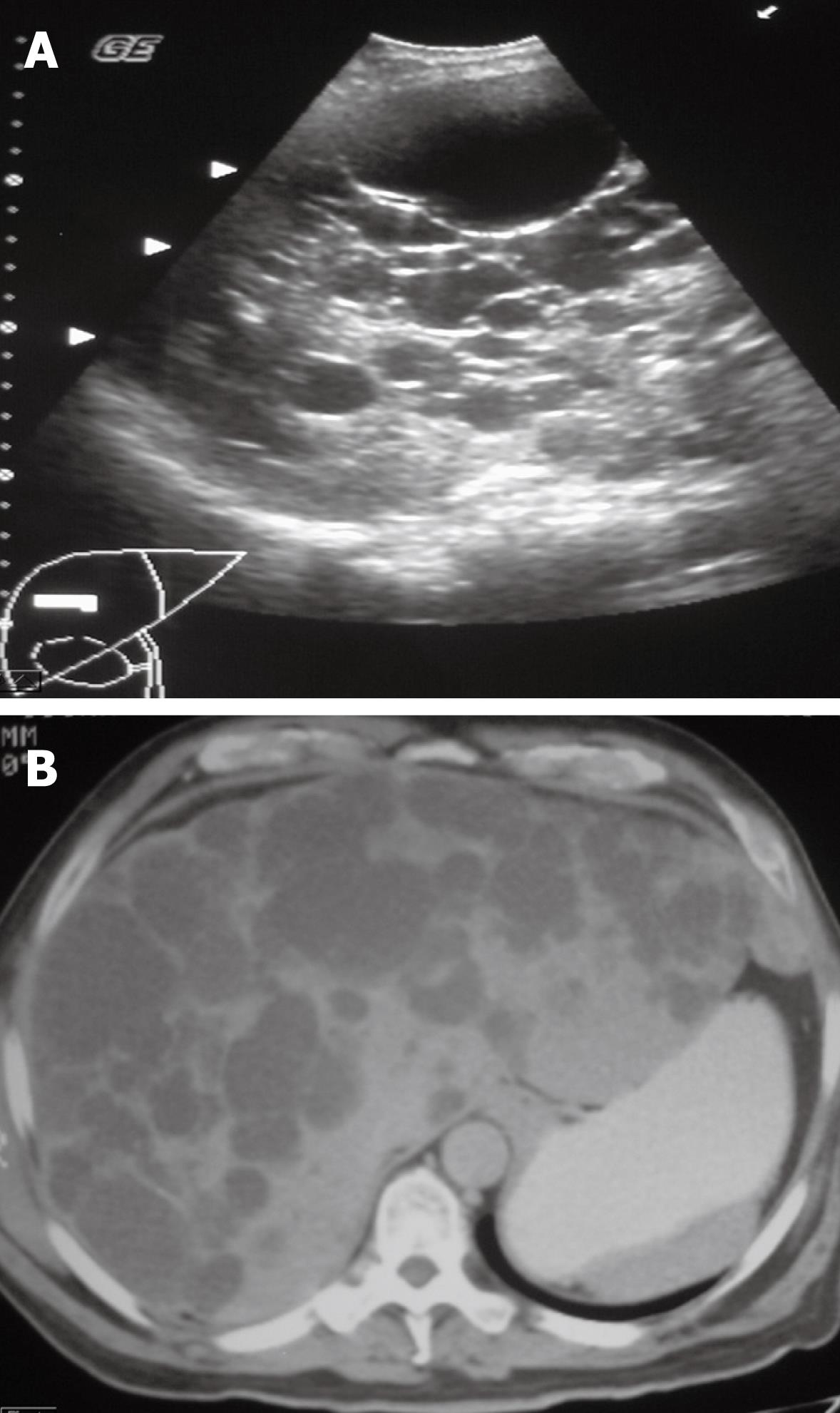
Polycystic liver disease (PLD) is an autosomic dominant disease related to chromosome 19 alterations in patients with hepatic involvement alone and in chromosomes 4 and 16 in those with renal cysts[1]. At autopsy, the prevalence appears to be 0.13%-0.6%, and the association to renal cysts about 30%[2–4]. PLD is generally asymptomatic and incidentally diagnosed. Abdominal pain, distension, early satiety, nausea and vomiting are common and hepatic function is rarely affected. Ultrasound (US) and computed tomography (CT) are common diagnostic methods. PLD is considered when more than 5 cysts are observed in the liver that typically appear anechoic, round and smooth-walled with distal echo enhancement in the US[5] (Figure 1A); and in CT with homogeneous fluid density and without wall or content enhancement after contrast administration[6] (Figure 1B). Invasive treatment (IT) such as cyst aspiration with sclerotherapy, open fenestration (OF), laparoscopic fenestration (LF), fenestration plus hepatic resection (FHR), and hepatic transplantation in selected cases are preferred[147–10]. Symptoms are controlled with surgical liver volume reduction[11]. In a Mexican population, surgery for PLD has shown to modify quality of life[12]. We report a descriptive analysis of 41 patients with clinical and imaging diagnosis of PLD that have a complete follow-up during July 1986 to June 2006, making special emphasis on factors that influence outcome of both non-invasive and invasive treatment.
This is a descriptive study of all patients diagnosed with PLD diagnosis from July 1986 to June 2006 at the National Institute of Health Sciences and Nutrition “Salvador Zubirán”. Forty-nine clinical records with PLD diagnosis were reviewed; however, 8 patients were excluded from the analysis because the follow-up was not completed.
Variables as gender, age at diagnosis, time of diagnosis delay, BMI, symptoms, diagnosis method, cyst diameter, cyst complications (CC), liver function tests (LFT: bilirubin, transaminases, AP, lactic dehydrogenase, gamma glutamyl transpeptidase, albumin, prothrombin time, glucose and complete blood count at diagnosis, 1 and 6 months, and at 1, 5, 10, 15 and 20 years), comorbidity, extrahepatic cysts, hormonal replacement therapy (HRT) intake, IT requirement, IT complications, recurrence of symptoms (RS), and follow up procedures and outcome were analyzed.
Statistical data are expressed as mean ± SD. Numerical variables were analyzed by t-test and the categorical with χ2 test or Fisher’s exact test. A P value ≤ 0.05 was accepted as being statistically significant. The SPSS 13.0 software (SPSS Inc., Chicago, Illinois, 2004) statistical program was used for the analysis.
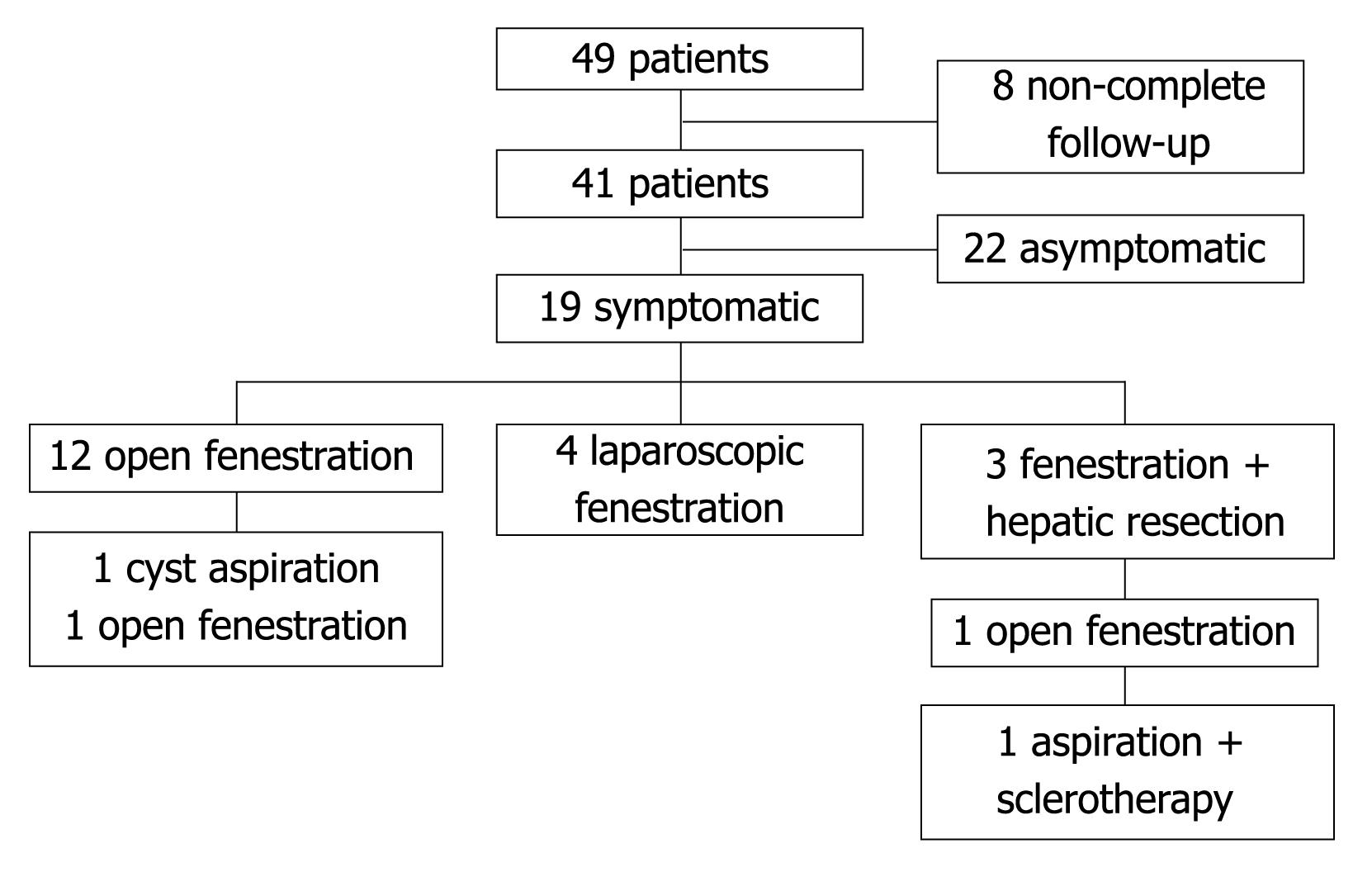
A total of 49 patients with PLD were evaluated in our institution. Eight patients lost follow-up and were not included for the analysis. Forty-one (male 7, female 34) complete patients files were included (Figure 2). The mean age at diagnosis was 47.8 ± 11.9 years (range 27-82) and the mean follow-up time was 5.7 years. Eighteen (44%) patients had familiar history of PLD. Demographical data is shown in Table 1.
| N (Male/Female) | 41 (7/34) |
| Age at diagnosis (range, yr) | 47.8 ± 11.9 (27-82) |
| Mean diagnosis retard time (range, yr) | 2.8 (0-9) |
| Mean follow up time (yr) | 5.7 |
| Familiar history of PLD | 44% |
| Body mass index at diagnosis | |
| ≤ 25 | 41% |
| > 25-≤ 30 | 44% |
| > 30 | 15% |
| Largest cyst diameter (range, cm) | 8.2 ± 4.9 (2-25) |
| Extrahepatic cysts | |
| Renal cysts | 68% |
| Pancreatic cysts | 15% |
| Spleen cysts | 8% |
| Ovary cysts | 2% |
| Comorbidity | |
| Arterial hypertension | 46% |
| Chronic renal insufficiency | 24% |
| Dyslipidemia | 15% |
| Hypothyroidism | 7% |
| Type 2 diabetes | 5% |
| Gastroesophageal reflux | 5% |
We found that 23.8% of postmenopausal women were taking HRT. In those patients the prevalence of symptoms at diagnosis was significantly higher than those without HRT (100% vs 43.8%, P = 0.039; OR = 2.286; 95% CI, 1.311-3.984). The requirement of IT also was higher in the HRT group than in non-HRT (80% vs 6.3%, P = 0.001; OR = 20; 95% CI, 35-115). The size of the major cyst was not associated with HRT (P > 0.05). The oral contraceptive intake was not associated with occurrence of symptoms (P > 0.05).
Based on the initial symptoms the mean time of diagnosis delay was 2.8 (range 0-9) years. We found that 65.4% of the symptomatic versus 14.3% of non-symptomatic patients at diagnosis required IT (P = 0.002, OR = 11.333, 95% CI, 2.068-62.105). The symptoms described were abdominal pain 56%, early satiety 42%, increase of the abdominal perimeter 34%, and nausea 12%. Two patients (4.9%) had portal hypertension manifested by esophageal varices and splenomegaly, and none of them was found with ascites or encephalopathy.
During the follow up time, symptomatic patients at diagnosis developed more CC than non-symptomatic (29.6% vs 0, P = 0.023). At this time, nine (22%) patients had CC: cyst infection 5 (55.6%), cyst bleeding 3 (33.3%), and cholangitis 1 (11.1%), at a mean time of 4 months (range 0-9, Table 2). In this group of patients, four (44.4%) had a complication at the time of diagnosis (cyst infection 2, cyst bleeding 2).
| Symptomatic patients at diagnosis | 27 (66%) |
| Abdominal pain | 15 |
| Early satiety | 12 |
| Increase of abdominal perimeter | 9 |
| Nausea | 3 |
| Complications during follow up | 9 (22%) |
| Cyst infection | 5 |
| Cyst hemorrhage | 3 |
| Cholangitis | 1 |
| Invasive treatment patients | 19 (46%) |
| Open fenestration | 12 |
| Laparoscopic fenestration | 4 |
| Fenestration + hepatic resection | 3 |
| Overall symptoms recurrence | 4 (17%) |
| Open fenestration | 3 |
| Laparoscopic fenestration | 0 |
| Fenestration + hepatic resection | 1 |
| Surgery complications | 6 (32%) |
| Bleeding | 3 |
| Infection | 2 |
| Pain | 1 |
Renal cysts were present in 68% of PLD patients (Table 1). Liver CC were seen in 25% of patients with renal cysts, and in 7.7% of patients without them (P > 0.05).
At diagnosis, overweight (BMI > 25 but ≤ 30), was found in 44%; and obesity (BMI > 30), in 15%. Patients with BMI > 25 had a trend to develop surgical complications (P = 0.075) such as abdominal pain, bleeding or infection (Table 1), and no significant association was found with the presence of symptoms, largest cyst diameter, CC, or IT requirement (P > 0.05).
Diagnosis was achieved by US in 78% and by CT in 22%. The largest cyst mean diameter was 8.2 ± 4.9 cm (range 2-25) and no association to symptoms or require-ment of IT (P > 0.05) were found. The largest cyst mean diameter was 12.3 ± 8.8 cm in postmenopausal women taking HRT vs 8.3 ± 3.9 cm in those without HRT (P > 0.05).
No significant alterations in bilirubin, transaminases, lactic dehydrogenase, gamma glutamyl transpeptidase, albumin, prothrombin time, glucose, and in complete blood count, were found at diagnosis or during follow up.
Because we considered IT requirement as an end point in PLD patients, we studied its association with elevated levels of LFT at diagnosis, finding that AP was elevated (≥ 132 IU/mL) in 15.5% of patients. During follow-up, 100% of patients in the elevated AP group required IT versus 35.5% in the normal AP group (P = 0.005, OR = 2.818, 95% CI, 1.753-4.530).
Abdominal pain was the most common indication for surgery (78%). Other indications were satiety (10%), cyst hemorrhage (5%), and cyst infection (5%).
Nineteen patients (46%) required IT (OF 12, LF 4, FHR 3) to control symptoms (Figure 2), at a mean time of 19 months (range 0-85) after PLD diagnosis. Mean age for the first IT was 47 ± 10 years.
Because of RS, 3 patients required a second IT at a mean time of 19 months (range 8-24): 2 (16.7%) in the OF group (cyst aspiration 1, OF 1) and 1 (33.3%) in the FHR group (OF 1). The last patient required a third IT (aspiration + sclerotherapy) 6 months later. None of the patients in the LF group showed RS.
Complications due to the first IT were found in 6 (32%) patients. Three (16.7%) patients had complications in the OF group (bleeding 3), 1 (25%) in the LF group (severe abdominal pain 1), and 2 (66.7%) in the FHR group (bleeding 1, infection 1; Table 2). No significant difference in complications between OF and LF was found.
Two (66.7%) patients after a second IT (OF 2) developed important complications (hemorrhage 1, pleural effusion 1), and the one who required a third IT had severe abdominal pain. Follow up mortality rate was 0.
This is one of the largest series published to date and includes a large follow-up time in both symptomatic and non-symptomatic patients with a detailed description and associations to anthropometric and biochemical data, HRT intake, CC, IT requirement, IT complications, and outcome.
As in other case series[1910], female gender predominated (83%), suggesting a possible role of estrogens in the development of liver cysts.
Data shows selective increase in liver cyst and parenchymal volume in female patients receiving postmenopausal estrogen therapy[13], but it is not clear if it correlates with symptoms and IT requirement. The association found between HRT, the presence of symptoms and IT requirement supports that HRT has an important role in the development of symptoms and so in the requirement of IT in PLD patients. Interestingly HRT was not associated to the size of the major cyst, suggesting that symptoms are not due to the size of cysts but maybe to the number of cysts or the liver volume occupied by them. As in other liver diseases, PLD may contraindicate HRT. Further and prospective studies are recommended to confirm such associations.
As others centers that inform that the diagnosis is more common during the fourth and the fifth decade of life[914], in Mexican patients seems to be equal.
No other series report the time evolution of PLD patients. We found a diagnosis delay time near to 3 years. This data may indicate that symptoms at the beginning of the disease are absent or mild and appear or increase as time advances, so patients search for medical attention.
Symptoms predicted IT requirement and were associated to a higher incidence of CC (bleeding, infection, etc). Most of the series report that the majority of patients are asymptomatic at diagnosis[1], but we found a high prevalence of symptoms (66%) in Mexican patients. We found a higher prevalence of abdominal pain (56%) than reported in other studies (36.5%)[9].
Hepatic failure in PLD patients is rare and few cases have been reported[1516]. We found 2 (4.9%) cases of portal hypertension and none with ascites or encephalopathy. The cause of portal hypertension in these patients is not clear, but might be due to the mass effect that comprises vessels of the portal circulation. A reported rate of 2.5% for portal hypertension has been described[9]. Despite hepatomegaly, portal hypertension and its complications (ascites, variceal bleeding, etc) remain quite rare[1], interestingly; we report a higher rate of portal hypertension in our patients, maybe due to a longer follow-up time.
In our knowledge this is one of the largest follow-up in a PLD case series (5.7 years). Bistritz et al[9] reported that in 40 patients with a follow-up time of 4.69 years, 22.5% had cyst bleeding, 12.5% cyst rupture, 12.5% cyst infection, and 2.5% developed portal hypertension. During follow-up symptomatic patients of our study developed similar incidence of CC. We found a significant association between prevalence of symptoms and the development of CC during follow-up (P = 0.023). It suggests that symptomatic patients have increased risk factors that predispose CC. The presence of renal cysts did not significantly increase the incidence of liver CC (P > 0.05).
The association between anthropometric data and symptoms in PLD has not been studied. We found a trend to surgical complications in patients with BMI > 25 (P = 0.075), and no significant association with symptoms, largest cyst diameter, CC, or IT requirement. The BMI is not a reliable data because it is influenced by the large amount of hepatic weight in PLD patients, so other anthropometric measurement must be achieved in future studies, especially to quantify fat tissue. It is known that fat tissue is a hormonal-active tissue, though may influence the clinical presentation and outcome of PLD patients, as happens with HRT.
By far, US is reported as the most used method for diagnosis[1]. Our finding supports that US is a good and reliable method to achieve PLD diagnosis and brings important data such as number of cysts, cyst diameter and cyst complications. It is unclear if the cyst diameter is associated to symptoms or IT requirement. We found that despite a large cyst diameter, symptoms or requirement of IT are not related to it. It suggests that what determines the occurrence of symptoms or indicates surgical therapy is not the cyst diameter, but the number of cysts or the liver volume occupied by them. Further studies are necessary to determine the clinical value of these measures, including measure of liver volume.
The LFT in our patients usually were normal and were not associated to symptoms or outcome. We did not find significant alterations at diagnosis or during follow up. In his review, Arnold[1] described that LFT are often normal, but in symptomatic patients, AP levels may be elevated in 30%-47%, GGT in 60%-70%, aspartate aminotransferase in up to 27%, and bilirubin in 17%. We studied those variables, and only the elevation of AP (≥ 132 mg/dL) at diagnosis was significantly associated with requirement of IT. This association suggests that elevated AP may be an important serological marker of disease activity and could be used to indicate IT to control symptoms.
Symptoms and complications are reported indications for IT. According to Chen[4] and Que et al[17] these indications include abdominal distention, abdominal pain, early satiety, fatigue, supine dyspnea, infected cysts, dialysis hypotension, bile duct obstruction, severe ascites and uterine prolapse. We found similar indications in our patients, being pain the most frequent.
RS is frequent with the majority of IT modalities. The reported rate of RS for cyst aspiration is up to 100% and probably does not provide definitive therapy[18]. The RS for OF is less common. One of the largest series is the one reported by Koperna et al[19] who described a RS rate of 21%, but also rates between 11%-33% had been reported[20–23]. For LF, a recent case series of 6 PLD patients reported by Garcea et al[24] showed 16% of RS, but also has been reported in up to 4.5%-71%[2225]. In our patients, the RS after a first IT was low (16.7% for OF, 0% for LF, and 33.3% for FHR). The RS rate for OF and for FHR was as expected, interestingly the non-RS after LF is much lower than reported[232426]. We think those findings may be due to patient selection criteria.
For OF the reported morbidity rate is 0%-56%[2127], for LF 0%-54%[2128], and for FHR varies from 20% to 100%[2930]. The higher rate of complications in the LF group compared to the OF group may be due to procedure selection criteria. The rate of complications after FHR was high but as expected. Randomized studies are necessary to know the real rate of complications and RS with each procedure, but as the prevalence of the disease is low, studies are difficult to perform.
In summary, the presence of symptoms at diagnosis, and CC during follow-up time is associated with IT requirement. The HRT is associated to the presence of symptoms and IT requirement. The prevalence of symptoms in PLD patients is high and abdominal pain is the most common. Patients with BMI > 25 have a trend to suffer from complications after IT. Cyst diameter is not associated with the presence of symptoms or need for IT. The AP elevation was associated with IT requirement, suggesting that AP may be a marker of disease severity. In near half of the patients, a first IT is performed and complications are frequent, especially in the FHR group, but the proportion of complications due to the second IT is higher. The RS is more frequent after OF, but this fact may be due to patient selection bias.
Polycystic liver disease (PLD) is generally asymptomatic and incidentally diagnosed. For symptomatic patients invasive treatment (IT) such as cyst aspiration with sclerotherapy, fenestration with or without hepatic resection, and hepatic transplant are options of treatment. There are no known associations that could help clinicians to determine the outcome of invasive or non-invasive treatment.
Larger and prospective studies are required in order to find other variables that may affect outcome. It is important to evaluate the physiological basis of the impact of hormonal replacement therapy (HRT) on the outcome of PLD patients.
Knowledge of factors associated with IT requirement, complications, and recurrence of symptoms.
Helpful to determine outcome in both invasive and non-invasive treatment of PLD patients.
This is a retrospective study investigating the association for invasive or noninvasive treatment of polycystic liver disease and biochemical abnormalities. It is a well-written and well-designed paper.
| 1. | Arnold HL, Harrison SA. New advances in evaluation and management of patients with polycystic liver disease. Am J Gastroenterol. 2005;100:2569-2582. |
| 2. | Milutinovic J, Fialkow PJ, Rudd TG, Agodoa LY, Phillips LA, Bryant JI. Liver cysts in patients with autosomal dominant polycystic kidney disease. Am J Med. 1980;68:741-744. |
| 3. | Thomsen HS, Thaysen JH. Frequency of hepatic cysts in adult polycystic kidney disease. Acta Med Scand. 1988;224:381-384. |
| 4. | Chen MF. Surgery for adult polycystic liver disease. J Gastroenterol Hepatol. 2000;15:1239-1242. |
| 5. | Spiegel RM, King DL, Green WM. Ultrasonography of primary cysts of the liver. AJR Am J Roentgenol. 1978;131:235-238. |
| 6. | Mortele KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001;21:895-910. |
| 7. | Koyama I, Fuchinoue S, Urashima Y, Kato Y, Tsuji K, Kawase T, Murakami T, Tojimbara T, Nakajima I, Teraoka S. Living related liver transplantation for polycystic liver disease. Transpl Int. 2002;15:578-580. |
| 8. | Tan YM, Ooi LL. Highly symptomatic adult polycystic liver disease: options and results of surgical management. ANZ J Surg. 2004;74:653-657. |
| 9. | Bistritz L, Tamboli C, Bigam D, Bain VG. Polycystic liver disease: experience at a teaching hospital. Am J Gastroenterol. 2005;100:2212-2217. |
| 10. | Everson GT, Taylor MR, Doctor RB. Polycystic disease of the liver. Hepatology. 2004;40:774-782. |
| 11. | van Keimpema L, Ruurda JP, Ernst MF, van Geffen HJ, Drenth JP. Laparoscopic fenestration of liver cysts in polycystic liver disease results in a median volume reduction of 12.5%. J Gastrointest Surg. 2008;12:477-482. |
| 12. | Orozco H, Mercado MA, Hinojosa CA. [Evaluation of 20 years of experience and quality of life in patients surgically treated for liver cystic disease]. Rev Gastroenterol Mex. 2001;66:179-186. |
| 13. | Sherstha R, McKinley C, Russ P, Scherzinger A, Bronner T, Showalter R, Everson GT. Postmenopausal estrogen therapy selectively stimulates hepatic enlargement in women with autosomal dominant polycystic kidney disease. Hepatology. 1997;26:1282-1286. |
| 14. | Kornprat P, Cerwenka H, Bacher H, El-Shabrawi A, Tillich M, Langner C, Mischinger HJ. Surgical therapy options in polycystic liver disease. Wien Klin Wochenschr. 2005;117:215-218. |
| 15. | Elias TJ, Bannister KM, Clarkson AR, Faull RJ. Progressive hepatic failure secondary to adult polycystic kidney disease. Aust N Z J Med. 1999;29:282-283. |
| 16. | Nakanuma Y, Hoso M, Hayashi M, Hirai N. Adult polycystic liver presenting with progressive hepatic failure. J Clin Gastroenterol. 1989;11:592-594. |
| 17. | Que F, Nagorney DM, Gross JB Jr, Torres VE. Liver resection and cyst fenestration in the treatment of severe polycystic liver disease. Gastroenterology. 1995;108:487-494. |
| 18. | Saini S, Mueller P, Ferrucci J. Percutaneous aspiration of hepatic cysts does not provide definitive therapy. Am J Roentgenol. 1983;141:559-560. |
| 19. | Koperna T, Vogl S, Satzinger U, Schulz F. Nonparasitic cysts of the liver: results and options of surgical treatment. World J Surg. 1997;21:850-854; discussion 854-855. |
| 20. | Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Laparoscopic management of symptomatic multiple hepatic cysts: a combination of deroofing and radical excision. JSLS. 2007;11:466-469. |
| 21. | Gigot JF, Jadoul P, Que F, Van Beers BE, Etienne J, Horsmans Y, Collard A, Geubel A, Pringot J, Kestens PJ. Adult polycystic liver disease: is fenestration the most adequate operation for long-term management? Ann Surg. 1997;225:286-294. |
| 22. | van Erpecum KJ, Janssens AR, Terpstra JL, Tjon A Tham RT. Highly symptomatic adult polycystic disease of the liver. A report of fifteen cases. J Hepatol. 1987;5:109-117. |
| 23. | Martin IJ, McKinley AJ, Currie EJ, Holmes P, Garden OJ. Tailoring the management of nonparasitic liver cysts. Ann Surg. 1998;228:167-172. |
| 24. | Garcea G, Pattenden CJ, Stephenson J, Dennison AR, Berry DP. Nine-year single-center experience with nonparastic liver cysts: diagnosis and management. Dig Dis Sci. 2007;52:185-191. |
| 25. | Bai XL, Liang TB, Yu J, Wang WL, Shen Y, Zhang M, Zheng SS. Long-term results of laparoscopic fenestration for patients with congenital liver cysts. Hepatobiliary Pancreat Dis Int. 2007;6:600-603. |
| 26. | Katkhouda N, Hurwitz M, Gugenheim J, Mavor E, Mason RJ, Waldrep DJ, Rivera RT, Chandra M, Campos GM, Offerman S. Laparoscopic management of benign solid and cystic lesions of the liver. Ann Surg. 1999;229:460-466. |
| 27. | Hansman MF, Ryan JA Jr, Holmes JH 4th, Hogan S, Lee FT, Kramer D, Biehl T. Management and long-term follow-up of hepatic cysts. Am J Surg. 2001;181:404-410. |
| 28. | Kabbej M, Sauvanet A, Chauveau D, Farges O, Belghiti J. Laparoscopic fenestration in polycystic liver disease. Br J Surg. 1996;83:1697-1701. |
| 29. | Soravia C, Mentha G, Giostra E, Morel P, Rohner A. Surgery for adult polycystic liver disease. Surgery. 1995;117:272-275. |
| 30. | Yang GS, Li QG, Lu JH, Yang N, Zhang HB, Zhou XP. Combined hepatic resection with fenestration for highly symptomatic polycystic liver disease: A report on seven patients. World J Gastroenterol. 2004;10:2598-2601. |