Published online May 14, 2008. doi: 10.3748/wjg.14.2920
Revised: March 19, 2008
Published online: May 14, 2008
The paper studies the combined radiologic and endoscopic approach (rendez vous technique) to the treatment of the biliary complications following liver transplant. The “rendez-vous” technique was used with an electrokinetic lithotripter, in the treatment of a biliary anastomotic stricture with multiple biliary stones in a patient who underwent orthotopic liver transplant. In this patient, endoscopic or percutaneous transhepatic management of the biliary complication failed. The combined approach, percutaneous transhepatic and endoscopic treatment (rendez-vous technique) with the use of an electrokinetic lithotritor, was used to solve the biliary stenosis and to remove the stones. Technical success, defined as disappearance of the biliary stenosis and stone removal, was obtained in just one session, which definitively solved the complications. The combined approach of percutaneous transhepatic and endoscopic (rendez-vous technique) treatment, in association with an electrokinetic lithotritor, is a safe and feasible alternative treatment, especially after the failure of endoscopic and/or percutaneous trans-hepatic isolated procedures.
- Citation: Pisa MD, Traina M, Miraglia R, Maruzzelli L, Volpes R, Piazza S, Luca A, Gridelli B. A case of biliary stones and anastomotic biliary stricture after liver transplant treated with the rendez - vous technique and electrokinetic lithotritor. World J Gastroenterol 2008; 14(18): 2920-2923
- URL: https://www.wjgnet.com/1007-9327/full/v14/i18/2920.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2920
Biliary complications after liver transplant are a very common and important problem (8%-50%)[12]. Untreated biliary complications are associated with high morbidity and mortality rates. Magnetic resonance is an effective technique in the diagnosis of the biliary complications[3], whereas Endoscopic retrograde cholangiopancreatography (ERCP)[45], and Percutaneous Transhepatic Cholangiography (PTC) remain the gold standard therapeutic options (with successful results in between 70% and 80% of cases)[67]. Common biliary complications after liver transplant are leaks and strictures, which are divided into anastomotic and non-anastomotic groups. Other less frequent complications include stones, cuts, and oddities[89].
We report a case of biliary anastomotic stenosis with multiple biliary stones in a patient after orthotopic liver transplantation, treated with a combined percutaneous radiologic and endoscopic approach (rendez - vous technique) and with the use of an electrokinetic lithotritor.
A 67-year-old man underwent orthotopic liver transplantation for HCV related cirrhosis in 2000, with a choledocho - choledocho anastomosis. The surgical procedure was complicated by renal failure which was treated with hemodialysis for 1 mo. No vascular abnormalities were present at the Doppler ultrasound examination. Five years later, after an unsuccessful antiviral treatment for HCV recurrence, medium size esophageal varices were diagnosed. Other co-morbidities present at that time were severe obesity and hypertension.
The patient was recently admitted to our facility because of the onset of severe cholestasis with episodes of cholangitis, and for a general reassessment of the liver disease.
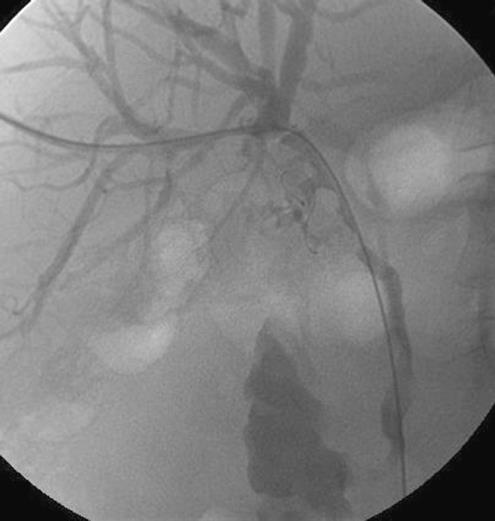
At admission, physical examination showed severe obesity (BMI > 30) and umbilical laparocele (Figure 1). Laboratory data were the following: AST/ALT 130/187 U/L (normal, 5/65 U/L-40/65 U/L), bilirubin tot/dir 26.46/19.69 mg/dL (0-1.5 mg/dL), alkaline phosphates 357 U/L (40 U/L-134 U/L), gamma-GT 1161 mg/L (5 U/L-85 U/L). A Magnetic Resonance Cholangiography was not performed because of the severe obesity; ERCP was therefore planned. Under general anesthesia, the choledochus was cannulated, showing a mild anastomotic stricture with a very tight angle, just above the stricture, multiple stones above the stenosis and at the confluence, and mild intrahepatic biliary dilation (Figure 2). A guide wire was passed through the stenosis, but because of the stones and the kinking, it was impossible to cross, by the guide wire, either Dormia basket, Fogarty or other catheters. Because of ERCP failure, a PTC was planned. In the angiographic room, under sonographic and fluoroscopic control, a peripheral right biliary duct was punctured with a 20 G needle. A cholangiogram showed a mild biliary dilation and multiple filling defects. It was impossible to put a guide wire into the choledochus, and thus a 6.6 F Ring external cathether (Boston Scientific, MA, USA) was placed for bile drainage. One week later, a second cholangiogram was performed and a 6.6 Fr external - internal biliary catheter (Boston Scientific) was successfully placed (Figure 3).
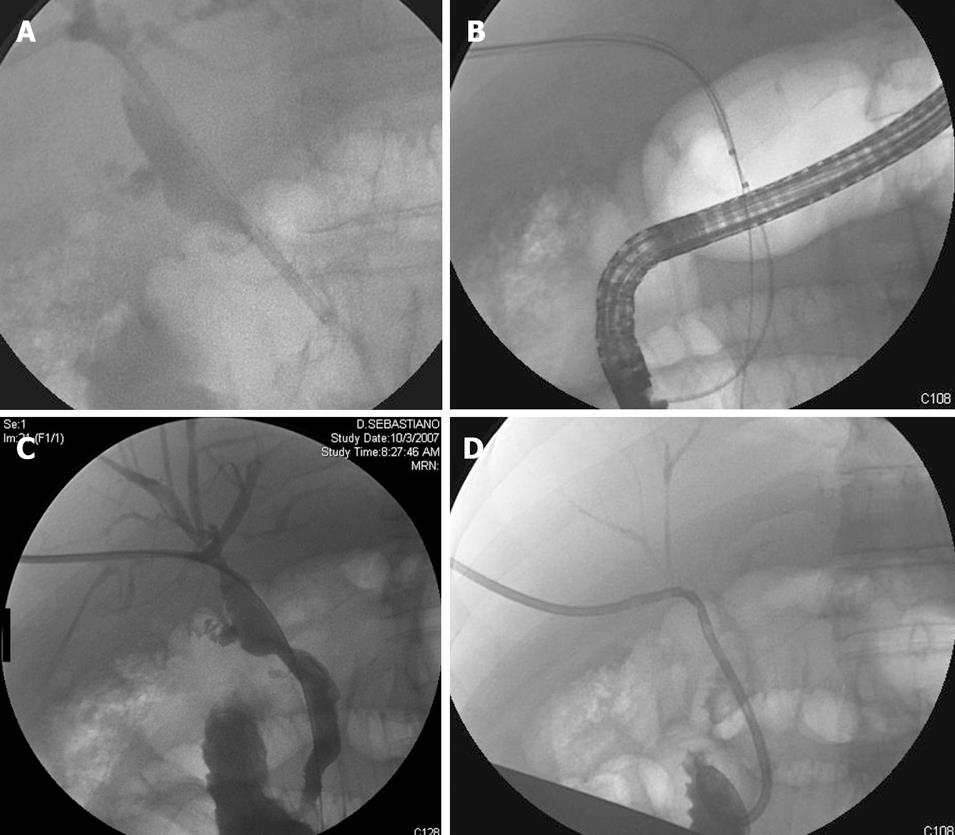
In the following days, because of worsening jaundice (bilirubin tot/dir 34.22/28.78 mg/dL), a combined radiologic and endoscopic technique (rendez vous technique) was performed. In the angiographic suite under general anesthesia, the patient was monitored continuously with electrocardiography, pulse oximeter and automatic recording of blood pressure and pulse. Intravenous antibiotic prophylaxis was given before the procedure. After visualizing the biliary tree, and under fluoroscopic control, on an Amplatz guide wire, the biliary drainage was changed with a 7 Fr vascular introductory (St. Jude Medical, Minnetonka, USA).
With an electro - kinetic lithotriptor, a ballistic lithotripter which uses high-energy magnetic fields (Electro Medical Supplies, LTD), placed trough the introductory, percutaneous lithotripsy was performed (Figure 4A). A percutaneous balloon dilatation of the anastomotic stricture was then performed using an 8 mm balloon catheter (Bluemax, Boston Scientific, MA, USA) and, at the same time, under endoscopic control, the stones were completely removed with a Fogarty balloon and a Dormia basket (Figure 4B). A final cholangiogram showed no filling defects or stricture (Figure 4C) and, at the end of the procedure, a 12 Fr external - internal biliary drainage was finally placed (Boston Scientific, MA, USA) (Figure 4D).
Two days later, laboratory data showed: AST/ALT 28/29 U/L (normal, 5/65-40/65 U/L), bilirubin tot/dir 6.5/5.3 mg/dL (0-1.5 mg/dL), alkaline phosphates 104 U/L (40-134 U/L), gamma-GT 107 mg/L (5-85 U/L).
Two months after the procedure, the patient has a biliary catheter in place, is asymptomatic, in good general condition, without signs of cholestasis and in follow up for biliary catheter removal.
Biliary complications after liver transplant are common and biliary stones represent a small part of these[12]. In the majority of cases, ERCP alone is not only the best diagnostic and therapeutic treatment with a successful result in 70%-80% of cases[4510] but is also considered the least invasive procedure, although with some important complications[9]. Western studies showed the efficacy of percutaneous transhepatic choledochoscopy (PTHC) and holmium:yttrium-aluminum-garnet (YAG) laser to remove biliary stones in patients unable or unwilling to undergo endoscopic or surgical removal, but this technique requires much time and prolonged biliary access[11].
In our patient, endoscopic management was attempted first, but we were unable to place a stent in a correct position or to remove the stones, because of the severe biliary stenosis. By a percutaneous transhepatic approach however, we were able to place an external - internal biliary catheter, though not to remove the stones or solve the stenosis.
By a combined technique - radiologic and endoscopic procedure (i.e. the “rendez-vous” technique), associated with the use of a ballistic lithotripter which usually fragments nearly all urinary calculi, we were able to remove the stones and to solve the stenosis.
The rendez-vous technique has been described in the treatment of benign or malignant biliary obstruction, in traumatic bile duct injury repair and in the treatment of large biliary leaks in a liver transplant recipient[12–15]. But, to our knowledge, this is the first report of the use of this technique in treatment of biliary stones and anastomotic stenosis, with the use of a ballistic lithotripter in a patient after liver transplantation.
In conclusion, the radiological/endoscopic rendez-vous technique, associated with an electrokinetic lithotritor, is a feasible alternative for stone removal and biliary stricture treatment, especially after the failure of endoscopic and/or percutaneous trans-hepatic isolated procedures. Also, this combined approach improve costs, timing and effectiveness in the therapy of biliary complications.
| 1. | Stratta RJ, Wood RP, Langnas AN, Hollins RR, Bruder KJ, Donovan JP, Burnett DA, Lieberman RP, Lund GB, Pillen TJ. Diagnosis and treatment of biliary tract complications after orthotopic liver transplantation. Surgery. 1989;106:675-683; discussion 683-684. |
| 2. | Greif F, Bronsther OL, Van Thiel DH, Casavilla A, Iwatsuki S, Tzakis A, Todo S, Fung JJ, Starzl TE. The incidence, timing, and management of biliary tract complications after orthotopic liver transplantation. Ann Surg. 1994;219:40-45. |
| 3. | Boraschi P, Braccini G, Gigoni R, Sartoni G, Neri E, Filipponi F, Mosca F, Bartolozzi C. Detection of biliary complications after orthotopic liver transplantation with MR cholangiography. Magn Reson Imaging. 2001;19:1097-1105. |
| 4. | Pfau PR, Kochman ML, Lewis JD, Long WB, Lucey MR, Olthoff K, Shaked A, Ginsberg GG. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation. Gastrointest Endosc. 2000;52:55-63. |
| 5. | Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int. 2003;23:156-162. |
| 6. | Ernst O, Sergent G, Mizrahi D, Delemazure O, L'Hermine C. Biliary leaks: treatment by means of percutaneous transhepatic biliary drainage. Radiology. 1999;211:345-348. |
| 7. | Cozzi G, Severini A, Civelli E, Milella M, Pulvirenti A, Salvetti M, Romito R, Suman L, Chiaraviglio F, Mazzaferro V. Percutaneous transhepatic biliary drainage in the management of postsurgical biliary leaks in patients with nondilated intrahepatic bile ducts. Cardiovasc Intervent Radiol. 2006;29:380-388. |
| 8. | Pascher A, Neuhaus P. Bile duct complications after liver transplantation. Transpl Int. 2005;18:627-642. |
| 9. | Khuroo MS, Al Ashgar H, Khuroo NS, Khan MQ, Khalaf HA, Al-Sebayel M, El Din Hassan MG. Biliary disease after liver transplantation: the experience of the King Faisal Specialist Hospital and Research Center, Riyadh. J Gastroenterol Hepatol. 2005;20:217-228. |
| 10. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. |
| 11. | Piraka C, Shah RJ, Awadallah NS, Langer DA, Chen YK. Transpapillary cholangioscopy-directed lithotripsy in patients with difficult bile duct stones. Clin Gastroenterol Hepatol. 2007;5:1333-1338. |
| 12. | Hazey JW, McCreary M, Guy G, Melvin WS. Efficacy of percutaneous treatment of biliary tract calculi using the holmium:YAG laser. Surg Endosc. 2007;21:1180-1183. |
| 13. | Wayman J, Mansfield JC, Matthewson K, Richardson DL, Griffin SM. Combined percutaneous and endoscopic procedures for bile duct obstruction: simultaneous and delayed techniques compared. Hepatogastroenterology. 2003;50:915-918. |
| 14. | Aytekin C, Boyvat F, Yimaz U, Harman A, Haberal M. Use of the rendezvous technique in the treatment of biliary anastomotic disruption in a liver transplant recipient. Liver Transpl. 2006;12:1423-1426. |
| 15. | Miraglia R, Traina M, Maruzzelli L, Caruso S, Di Pisa M, Gruttadauria S, Luca A, Gridelli B. Usefulness of the "rendezvous" technique in living related right liver donors with postoperative biliary leakage from bile duct anastomosis. Cardiovasc Intervent Radiol. 2008;31:999-1002. |