INTRODUCTION
Appendiceal mucocele (AM) is a rare entity that can present with a variety of clinical symptoms or occur as an incidental surgical finding. The incidence is 0.2%-0.4% of all appendectomied specimens[1–3]. AM is a progressive dilatation of the appendix from the intraluminal accumulation of the mucoid substance[34]. It may be a benign or malignant process. There are four histological types, which lead to individualized surgical treatment and course in each case[3].
Preoperative diagnosis that distinguishes AM from acute appendicitis (AA) is essential for the best choice of surgical approach (open vs laparoscopic) to prevent peritoneal dissemination and perform the appropriate surgery[35]. Herein, we report 5 cases, discuss the diagnostic procedures and management algorithm of these patients, and review briefly the relevant literature. We also aimed to define the incidence of the AM in a tertiary referral centre in Northern Black Sea region of Turkey.
CASE REPORTS
Case 1
An 82-year-old man was admitted to the hospital because of pain in the right lower quadrant of the abdomen for 3 d. Standard laboratory tests, serum levels of CA 19-9 and carcino-embryonic antigen (CEA) were within normal ranges. Ultrasonography (USG) and computerized tomography (CT) demonstrated a well demarcated, elliptical 7 cm × 5 cm cystic mass with parietal calcifications in the right lower quadrant of the abdomen. There was an indentation in the cecum by colonoscopy. Surgical exploration revealed the mass to be an AM. Simple appendectomy was performed. Pathological examination revealed a mucinous cystadenoma with dimensions of 8 cm × 6 cm × 5.5 cm. AM restricted to the appendix and cecum was free of the disease. The patient’s postoperative course was unremarkable, and he was discharged home on the 4th postoperative day.
Case 2
A 65-year-old woman was referred to the emergency department with a diagnosis of AA. She complained of an abdominal pain which started 3 d before referral to our hospital. She had a history of coronary by-pass surgery 3 years ago. Physical examination showed diffuse peritoneal irritation. Plain radiography showed gas-fluid levels in the right lower quadrant. She also had mild leukocytosis. USG and CT scans of the abdomen showed presence of free fluid in the intra-abdominal spaces.
An emergency operation revealed ileal and cecal mesenteric ischemia. Partial ileum and cecum resection was performed. Histopathological diagnosis was ischemia of the intestine and simple mucocele of the appendix with a diameter of 5 mm, incidentally. Postoperative recovery was uneventful and she was discharged home on the 7th postoperative day.
Case 3
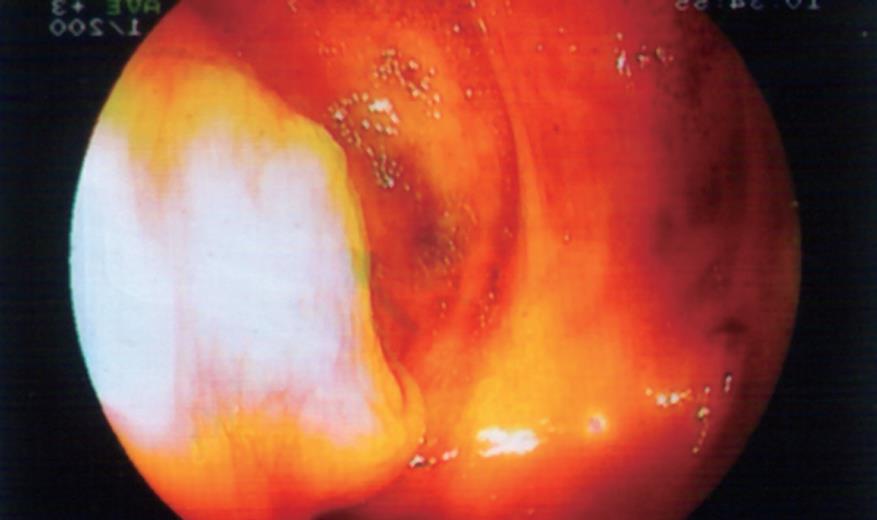
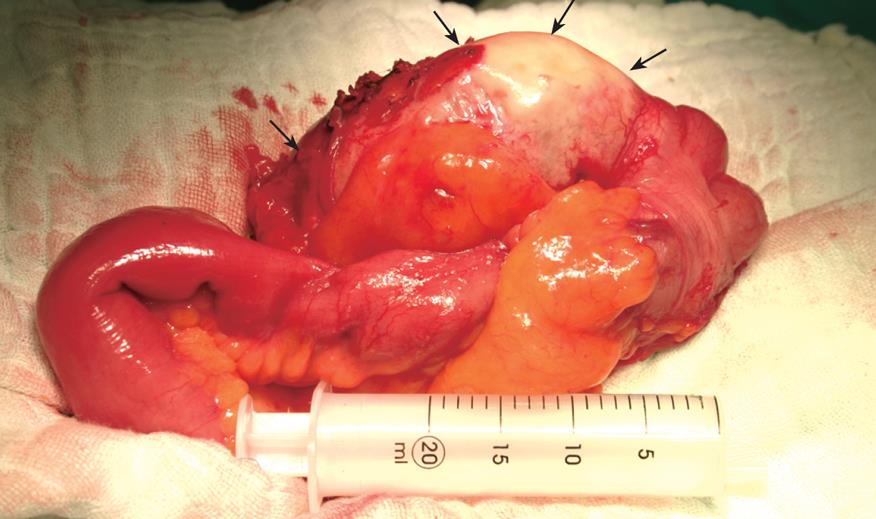
A 66-year-old woman was referred to the endoscopy unit for evaluation of a mass in the right lower quadrant of the abdomen with the suspicion of malignant tumor. She had visited another health care unit where the mass was revealed by ultrasound examination. She had been suffering from decreased appetite, nausea, and weakness lasting for a week. She had a history of upper GI hemorrhage managed medically 16 years ago and her surgical history was significant for cholecystectomy 14 years ago. Routine laboratory tests, including complete blood count and serum chemistry were unremarkable. Serum levels of CA19-9 and CEA were also within the normal ranges. USG of the abdomen showed a heterogenic mass (95 mm × 40 mm × 32 mm in dimensions) involving ileocecal part of the intestines. CT imaging revealed a soft tissue mass measuring 8 cm × 4 cm with peripheral enhancement in the region of the cecum (Figure 1). The patient underwent colonoscopy, which revealed a sub-mucosal protrusion to the lumen of the cecum, in the region of the appendiceal orifice. Orifice of the appendix was uncertain (Figure 2). Remaining of the colon was unremarkable. The patient was treated surgically. Surgical exploration revealed a mass in the appendix whitish-grey in color (Figure 3). Resection of cecum was followed by an ileocolic anastomosis. Frozen section examination revealed benign mucoid lesion. Formal pathologic report was hyperplastic type mucocele with evidence of secondary changes and chronic inflammatory mucosa of the intestine. The mucocele was 9.5 cm × 4 cm × 2 cm in dimensions with a wall thickness of 2 mm. There was no evidence of malignancy. Postoperative course was unremarkable and she was discharged home on the 5th postoperative day.
Figure 1 CT imaging of a soft tissue mass indicated by black arrows in the region of the cecum.
Figure 2 Colonoscopic view of the sub-mucosal mass.
Figure 3 Intra-operative view of the AM.
Arrows indicate the mucine filled appendix.
Case 4
A 58-year-old man was referred to the general surgery department for surgical treatment of toxic multi-nodular goitre. He had multiple previous admittances to internal medicine department and emergency department because of pain in the right lower quadrant of the abdomen and anemia. Physical examination was negative for abdominal mass or perianal or rectal lesions. The patient underwent endoscopy to investigate the etiology of anemia. Colonoscopy revealed a submucosal cecal mass. Abdominal CT revealed a polipoid a soft tissue mass measuring 4 cm × 3 cm with peripheral enhancement in the region of the cecum. The patient underwent total thyroidectomy and appendectomy. Histopathological diagnosis was benign cystadenoma without cecal involvement. Postoperative course was unremarkable and he was discharged home on the 6th postoperative day.
Case 5
A 72-year-old man underwent an open inguinal herniorrhaphy due to recurrent right inguinal hernia. He had complained of bulging and right groin pain which were exacerbated with activity. An appendiceal mass was defined during laparoscopic herniorrhaphy. Open access to the abdominal cavity was chosen. Simple appendectomy was performed with a clinical suspicion of appendiceal mucocele. Frozen section examination revealed appendiceal mucocele. Pathological examination reported a mucinous cystadenoma measuring 12.5 cm and 5.5 cm without cecal involvement. Postoperative course was unremarkable and he was discharged home on the 7th postoperative day in good conditions.
DISCUSSION
Mucocele of the appendix is an uncommon tumor, with an incidence of 0.29%-0.4% of all appendectomied specimens[1–36]. There has been no exact reported incidence of AM in Turkey. Histopathological examinations revealed 5 patients with AM among 240 patients who underwent appendectomies from January 2001 to October 2007 at our institution. The incidence of AM is revealed as 2.01%, which is higher than that reported in literature[78]. This may be related to the fact that our centre is a tertiary referral centre.
Although a small portion of AM is asymptomatic, clinical manifestations include right lower abdominal pain, palpable abdominal mass, or gastrointestinal bleeding in majority of the AM[1379–12]. Among the five cases reported above, three had abdominal pain secondary to mucocele while one had symptoms related to groin hernia and the last patient had abdominal pain due to intestinal infarction. AM was an incidental finding for those two patients.
USG, CT and colonoscopic examinations can facilitate preoperative diagnosis of AM[113–15]. Ultrasound is the first-line diagnostic modality for patients with acute abdominal pain or mass. Different sonographic findings of AM and AA have been described[31617]. Appendix diameter 15 mm or more in USG examination has been determined as the threshold for AM diagnosis with a sensitivity of 83% and a specificity of 92%[3]. Outer diameter threshold for AA diagnosis has been established as 6 mm[18]. USG examination revealed a cystic mass in the right lower quadrant in two of our patients. These findings revealed suspicion of AM.
CT is also an effective diagnostic tool for AM. CT can determine the relation between lesion and the neighbouring organs, and help confirm the diagnosis[15161920]. CT reveals a cystic mass with enhancing wall nodularly in the expected area of the appendix, especially in older patients, in whom AM should be considered[9151621]. AM could be visualized by CT in three of our patients. CT examination was normal in respect of AM for the third patient. AM was an incidental finding for this lady. Radiological investigation was not performed for the patient who had herniorrhaphy for recurrent groin hernia.
USG and CT findings are non-specific and the differential diagnosis should be established with benign appendiceal neoplasms and other pathologies such as carcinoid, lymphoma, mesenteric cysts, ovarian masses, and malign neoplasms of the appendix[722]. We did not perform fine needle aspiration as dictated in the literature in order to avoid dissemination of the mucus leading to pseudomyxoma peritonei[16].
Colonoscopy in patients with abdominal pain is a useful tool for determination of mucocele[223]. Generally, an elevation of the orifice of the appendix is seen. A yellowish mucous discharge would be visible from appendiceal orifice during colonoscopy. It is also important for the diagnosis of synchronous or metachronous colon tumor which would be as high as 29%[12713–152425]. Colonoscopic examinations on three of our patients revealed indentation in the cecum due to AM. The remaining colon was unremarkable in all of them. The 4th patient in emergency conditions was treated surgically based on the diagnosis of mesenteric ischemia and the 5th patient underwent surgery with the diagnosis of groin hernia without colonoscopic examination.
The spontaneous and surgery induced complications of AM include intestinal obstruction, intussusceptions[2022], intestinal bleeding[111325], fistula formation[1526], and volvulus[2728]. The worst complication is pseudomyxoma peritonei, characterized by peritoneal dissemination caused by iatrogenic or spontaneous rupture of the mucocele[5]. The tissues should be handled carefully during surgery in order to avoid rupture of the mucocele. Thus, conventional surgery is preferred rather than laparoscopic approaches for the treatment in our cases[25822]. Laparoscopic approach has an increased risk of rupture and subsequent pseudomyxoma peritonei formation[258]. Moreno et al[5] suggest conversion to an open appendectomy in case of mucocele when laparoscopic appendectomy is intended. Few authors still recommend a minimally invasive approach in selected patients for this rare entity[92729]. However, in these reports, laparoscopic approach has been adopted for a small number of patients. Thus, we need a large series to substantiate recommendations of laparoscopic approach.
A simple and thorough evaluation of these patients with a new algorithm has been suggested by Dhage-Ivatury and Sugarbaker[30]. Simple appendectomy is the choice of surgical treatment for patients with benign mucocele that has negative margins of resection without perforation. No long term follow-up is needed for these patients[282730]. Appendectomy was performed for three of our patients with a mucocele limited to the appendix. For patients with perforated mucocele, with positive margins of resection, positive cytology and positive appendiceal lymph nodes, right colectomy/cytoreductive surgery (CRS)/heated intraperitoneal chemotherapy (HIIC) and early postoperative intraperitoneal chemotherapy (EPIC) should be performed. Long term follow-up is obligatory for these patients[5243031].
Perforated mucocele with positive margins of resection, positive cytology, and negative appendiceal lymph nodes necessitate cecectomy/CRS/HIIC and EPIC. Long term follow-up is also obligatory for these patients[23032]. Cecectomy had been performed for one of the patients to obtain negative surgical margins, since the appendiceal wall was contiguous with the cecum and the intraoperative pathology indicated benign mucocele. Long term follow-up in this case has been carried out in the outpatient clinics. Perforated mucocele with positive cytology but negative margins of resection and negative appendiceal lymph nodes should be treated with appendectomy/CRS/HIIC and EPIC[2630]. We did not apply these treatment modalities as none of our patients had had positive lymph nodes or perforated mucocele.