Published online Apr 14, 2008. doi: 10.3748/wjg.14.2277
Revised: February 14, 2008
Published online: April 14, 2008
Biliary duct injuries are frequently iatrogenic, being associated with surgery for gallbladder stones. However, blunt abdominal trauma such as a motor vehicle crash is a rare cause of extrahepatic biliary stricture. A few reports have been published on biliary strictures treated with endoscopic therapy. In the present study, we describe a suprapancreatic biliary stricture associated with mesenteric tear following road traffic accident. We performed endoscopic stent placement, which was successful in relieving the biliary stricture.
- Citation: Kang DO, Kim TH, You SS, Min HJ, Kim HJ, Jung WT, Lee OJ. Successful endoscopic treatment of biliary stricture following mesenteric tear caused by blunt abdominal trauma. World J Gastroenterol 2008; 14(14): 2277-2279
- URL: https://www.wjgnet.com/1007-9327/full/v14/i14/2277.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2277
Benign bile duct strictures are uncommon and usually follow surgery for gallbladder stones, both open surgery and laparoscopic surgery[1]. However, development of biliary stricture after blunt abdominal trauma is an extremely rare condition[2–4]. No definitive treatment has been proposed for biliary strictures caused by blunt abdominal trauma. Recently, nonsurgical intervention using endoscopic approach has been used, with promising results[45]. We present a patient with a suprapancreatic biliary stricture that developed following a mesenteric tear caused by blunt abdominal trauma due to a traffic accident. The patient was treated successfully with endoscopic plastic stent placement.
A 36-year-old man had blunt abdominal trauma due to a traffic accident. The patient was the driver and suffered full impact with the steering wheel. The patient was hospitalized for the treatment of hemoperitoneum caused by a mesenteric tear. Surgery was performed and the mesenteric tear was repaired. Two weeks after the accident, the patient developed jaundice and was transferred to our hospital for further evaluation and management.
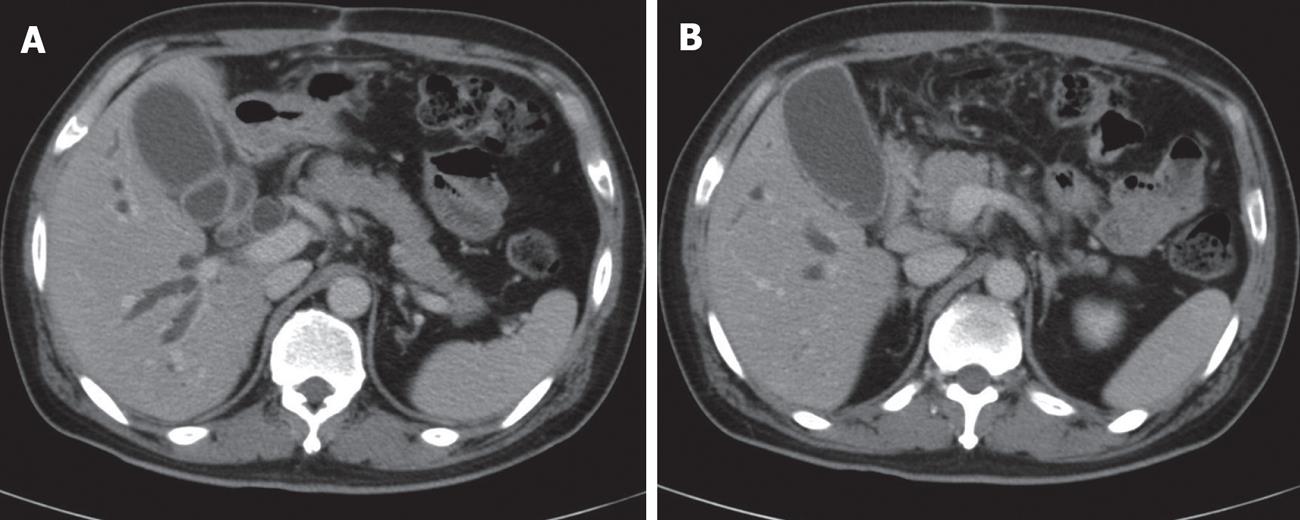
At admission, the patient had overt jaundice with itching over the entire body. The vital signs were stable. Physical examination showed no abdominal pain, or tenderness to palpation. The bowel sounds were normal. The initial liver function tests were as follows: aspartate aminotransferase 60 U/L (normal range, 0-37 U/L), alanine aminotransferase 92 U/L (normal range, 0-41 U/L), alkaline phosphatase 317 U/L (normal range, 35-130 U/L), gamma-glutamyl transferase 107 U/L (normal range, 8-61 U/L), total bilirubin 16.9 mg/dL (normal range, 0-1.2 mg/dL), and direct bilirubin 11.3 mg/dL (normal range, 0-0.3 mg/dL). The amylase and lipase levels were within the normal range. Computer tomography (CT) scan of the abdomen revealed dilatation of both intrahepatic (IHD) and extrahepatic biliary ducts (EHD) with abrupt cut-off of the suprapancreatic portion of the common bile duct (CBD) (Figure 1). There was no evidence of pancreatitis.
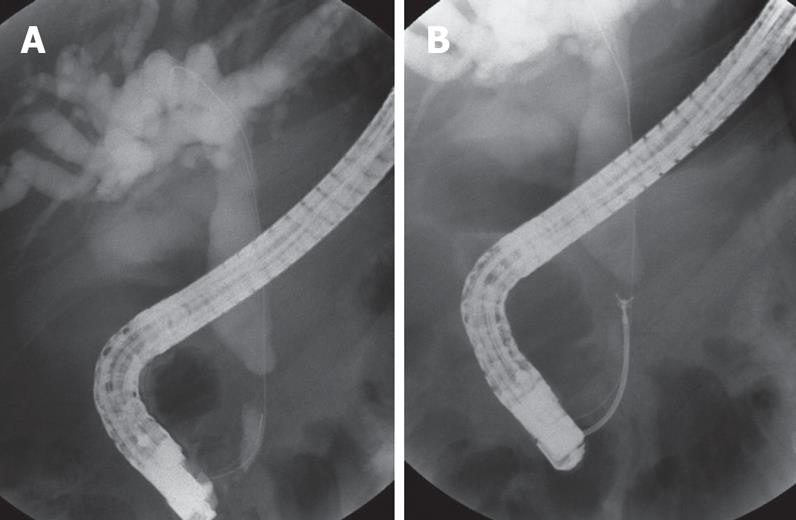
An endoscopic retrograde cholangiopancreatography (ERCP) was performed to determine the cause of the jaundice. The cholangiogram revealed a 1 cm long stenosis of the distal CBD just above the pancreas, with ductal dilatation above the narrowed portion. Endoscopic biliary sphincterotomy using a pull-type papillotome and brushing and biopsy of the narrowed part were performed (Figure 2). At the end of the procedure, an endoscopic nasobiliary drain (ENBD) was placed. After the procedure, the serum bilirubin levels decreased gradually. The cytology and biopsy results were negative for malignancy.
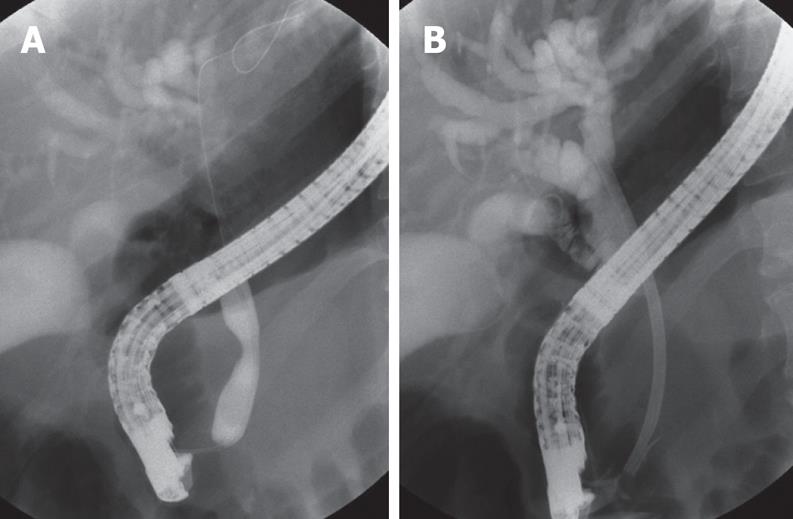
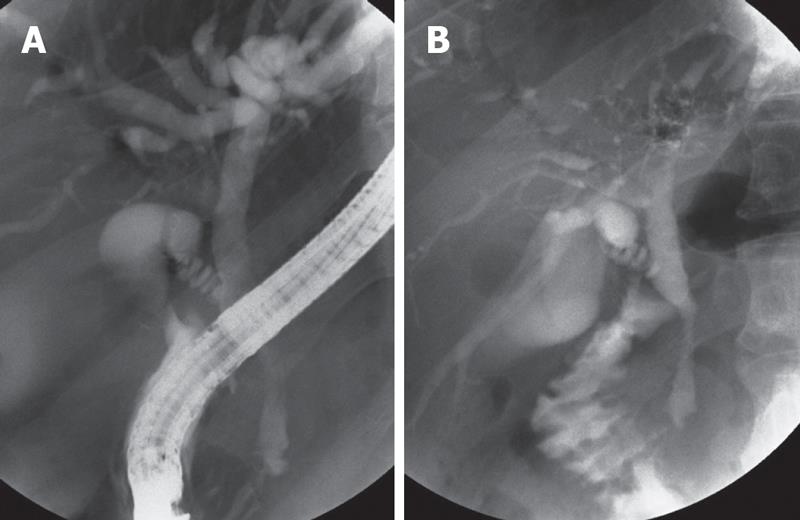
A repeat ERCP was performed 5 d after the first procedure and the CBD was dilated with TTS balloons. However, the stricture could not be dilated effectively. Therefore, a 12 Fr. plastic stent, 7 cm in length, was inserted and placed at the site of the lesion (Figure 3). Three months later, the patient was readmitted for a follow-up ERCP. The liver function tests were within the normal range and the patient did not have jaundice. The cholangiogram showed improvement of the CBD stricture. The plastic stent was removed after observing normal passage of radiocontrast material (Figure 4). During a follow-up period of 26 mo, there has been no recurrence of the biliary stricture as judged by laboratory tests and radiological imaging studies.
The bile ducts are located deep within the abdomen and are protected by the ribs, liver and mesentery. Therefore, non iatrogenic bile duct injuries secondary to blunt abdominal trauma are extremely rare. It is most commonly seen following motor vehicle accidents when an unrestrained driver has an impact with the steering wheel[2–4].
The proposed mechanisms of extrahepatic biliary strictures after blunt trauma differ based on their location. The possible mechanisms underlying the development of a suprapancreatic biliary stricture are: (1) local inflammation followed by fibrosis and stricture formation secondary to ductal tear; (2) disruption of the blood supply to the bile duct, and (3) compression of the biliary duct by an intramural or extrabiliary hematoma[3–5]. The possible mechanisms for the development of an intrapancreatic biliary stricture include the following: posttraumatic pancreatitis with swelling of the pancreatic head, and compression of the intrapancreatic portion of the CBD; this usually resolves as the swelling of the pancreas subsides[6]. We believe that the suprapancreatic biliary stricture in our patient was caused by disruption of the blood supply and extrinsic compression by a hematoma. The hepatobiliary area was not entered during the surgery, thus reducing the possibility of an iatrogenic trauma.
Most patients with a biliary stricture secondary to blunt abdominal trauma develop jaundice as the initial symptom. The onset of symptoms is insidious[35]. The condition may be mistaken for cholangiocarcinoma, if history of abdominal trauma is not available[7], and may result in unnecessary surgery.
The correct diagnosis may be difficult to determine based on imaging studies such as abdominal CT and ERCP, in the absence of a complete history[578]. Therefore, a high index of suspicion is required to ensure a proper diagnosis. To prevent irreversible fibrosis, an early diagnosis of biliary stricture is essential in order to allow timely treatment with percutaneous or endoscopic intervention[359]. Several workers have suggested that endoscopic stent placement is an effective treatment for suprapancreatic biliary strictures caused by blunt abdominal trauma[51011]. Park et al[5] reported eight patients with suprapancreatic biliary stricture due to blunt abdominal trauma. The median length of the stricture was 1 cm. Balloon dilatation was performed in only 1 patient. The median duration of plastic stent placement was 2.9 mo. The patients were all successfully treated with the endoscopic stent placement and there was no recurrence during the follow-up period (median 33 mo). Our case was similar in terms of clinical features and outcome compared to previously reported cases. Endoscopic stenting for biliary stricture after blunt abdominal trauma is associated with low morbidity and excellent long-term outcome[51011]. Therefore, endoscopic stenting is the treatment of choice for biliary strictures that develop after blunt abdominal trauma. Surgery should only be undertaken if endoscopic intervention fails[1213].
In summary, we report a patient with a suprapancreatic biliary stricture secondary to blunt abdominal trauma, which was treated successfully with endoscopic stent placement. The excellent results obtained in our patient suggest that endoscopic stent placement should be considered as the primary treatment for patients who develop an extrahepatic biliary stricture after blunt abdominal trauma. Endoscopic treatment is safe and has a favorable long-term outcome.
| 1. | Sawaya DE Jr, Johnson LW, Sittig K, McDonald JC, Zibari GB. Iatrogenic and noniatrogenic extrahepatic biliary tract injuries: a multi-institutional review. Am Surg. 2001;67:473-477. |
| 2. | Ivatury RR, Rohman M, Nallathambi M, Rao PM, Gunduz Y, Stahl WM. The morbidity of injuries of the extra-hepatic biliary system. J Trauma. 1985;25:967-973. |
| 3. | Horiguchi J, Ohwada S, Tanahashi Y, Sawada T, Ikeya T, Ogawa T, Aiba S, Shiozaki H, Yokoe T, Iino Y. Traumatic biliary stricture successfully treated by percutaneous transhepatic bile duct dilatation: a case report. Hepatogastroenterology. 1998;45:2038-2041. |
| 4. | Yoon KH, Ha HK, Kim MH, Seo DW, Kim CG, Bang SW, Jeong YK, Kim PN, Lee MG, Auh YH. Biliary stricture caused by blunt abdominal trauma: clinical and radiologic features in five patients. Radiology. 1998;207:737-741. |
| 5. | Park do H, Kim MH, Kim TN, Son HY, Lee TY, Kwon S, Oh HC, Lee SS, Seo DW, Lee SK. Endoscopic treatment for suprapancreatic biliary stricture following blunt abdominal trauma. Am J Gastroenterol. 2007;102:544-549. |
| 6. | Rohrmann CA Jr, Baron RL. Biliary complications of pancreatitis. Radiol Clin North Am. 1989;27:93-104. |
| 7. | Osei-Boateng K, Ravendhran N, Haluszka O, Darwin PE. Endoscopic treatment of a post-traumatic biliary stricture mimicking a Klatskin tumor. Gastrointest Endosc. 2002;55:274-276. |
| 8. | Gupta A, Stuhlfaut JW, Fleming KW, Lucey BC, Soto JA. Blunt trauma of the pancreas and biliary tract: a multimodality imaging approach to diagnosis. Radiographics. 2004;24:1381-1395. |
| 9. | Born P, Rosch T, Bruhl K, Sandschin W, Allescher HD, Frimberger E, Classen M. Long-term results of endoscopic and percutaneous transhepatic treatment of benign biliary strictures. Endoscopy. 1999;31:725-731. |
| 10. | Smith MT, Sherman S, Lehman GA. Endoscopic management of benign strictures of the biliary tree. Endoscopy. 1995;27:253-266. |
| 11. | Matlock J, Freeman ML. Endoscopic therapy of benign biliary strictures. Rev Gastroenterol Disord. 2005;5:206-214. |