Published online Mar 21, 2008. doi: 10.3748/wjg.14.1774
Revised: December 10, 2007
Published online: March 21, 2008
AIM: To determine factors affecting the outcome of patients with cirrhosis undergoing surgery and to compare the capacities of the Child-Turcotte-Pugh (CTP) and model for end-stage liver disease (MELD) score to predict that outcome.
METHODS: We reviewed the charts of 195 patients with cirrhosis who underwent surgery at two teaching hospitals over a five-year period. The combined endpoint of death or hepatic decompensation was considered to be the primary endpoint.
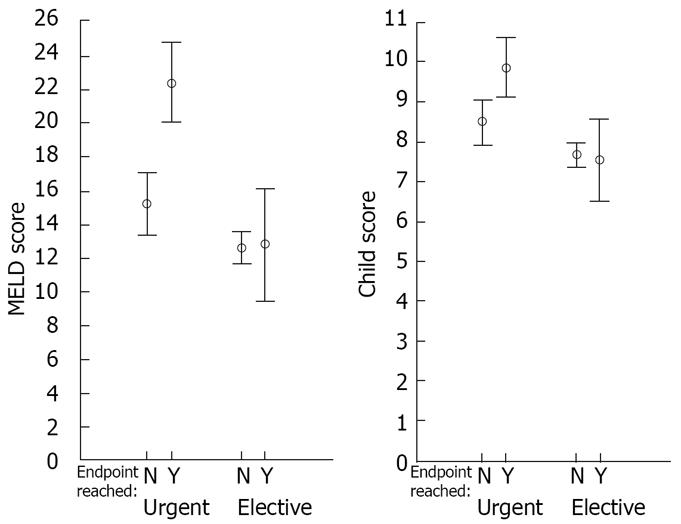
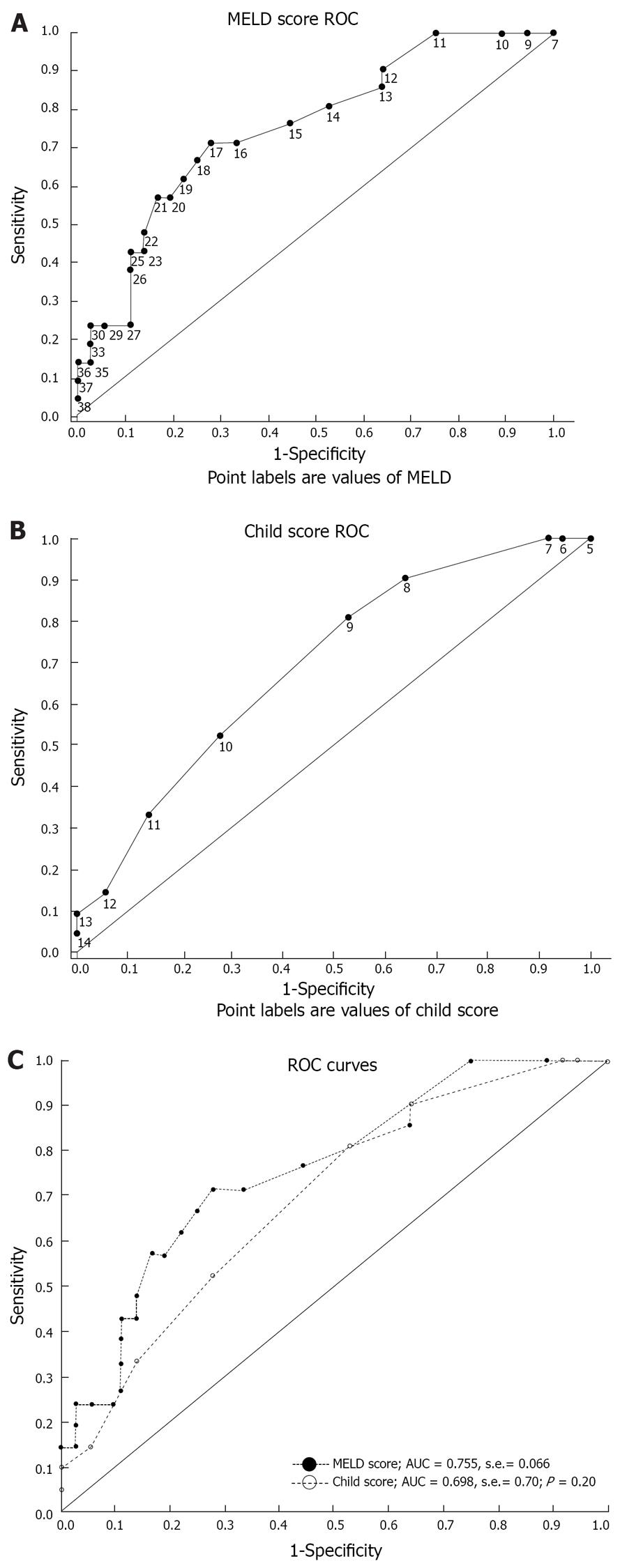
RESULTS: Patients who reached the endpoint had a higher MELD score, a higher CTP score and were more likely to have undergone an urgent procedure. Among patients undergoing elective surgical procedures, no statistically significant difference was noted in the mean MELD (12.8 ± 3.9 vs 12.6 ± 4.7, P = 0.9) or in the mean CTP (7.6 ± 1.2 vs 7.7 ± 1.7, P = 0.8) between patients who reached the endpoint and those who did not. Both mean scores were higher in the patients reaching the endpoint in the case of urgent procedures (MELD: 22.4 ± 8.7 vs 15.2 ± 6.4, P = 0.0007; CTP: 9.9 ± 1.8 vs 8.5 ± 1.8, P = 0.008). The performances of the MELD and CTP scores in predicting the outcome of urgent surgery were only fair, without a significant difference between them (AUC = 0.755 ± 0.066 for MELD vs AUC = 0.696 ± 0.070 for CTP, P = 0.3).
CONCLUSION: The CTP and MELD scores performed equally, but only fairly in predicting the outcome of urgent surgical procedures. Larger studies are needed to better define the factors capable of predicting the outcome of elective surgical procedures in patients with cirrhosis.
-
Citation: Hoteit MA, Ghazale AH, Bain AJ, Rosenberg ES, Easley KA, Anania FA, Rutherford RE. Model for end-stage liver disease score
versus Child score in predicting the outcome of surgical procedures in patients with cirrhosis. World J Gastroenterol 2008; 14(11): 1774-1780 - URL: https://www.wjgnet.com/1007-9327/full/v14/i11/1774.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1774
Patients with cirrhosis who undergo surgery under general anesthesia are at an increased risk of surgery and anesthesia-related complications[1]. The underlying liver dysfunction makes patients with cirrhosis particularly susceptible to bleeding and infection, two common post-surgical problems[2]. Moreover, the effect of surgery and anesthesia on the liver may be significant. Whereas the exact hemodynamic effect of different anesthetics on the hepatic circulation can be variable[3–5], the net result is usually a reduction in hepatic perfusion[6], thereby exposing the liver to the risk of ischemic injury. In addition, a number of anesthetic agents have a potential for direct, drug-induced hepatotoxicity[7–9]. Blood loss during surgery may result in hepatic hypoperfusion as well. Post-operative hypotension, sepsis and the subsequent use of medication with potential hepatotoxicity further increase the risk of liver injury[10]. A number of case series of patients with cirrhosis undergoing specific surgical procedures suggest a worse than expected outcome[11–15]. A review of 733 patients with cirrhosis undergoing various surgical procedures revealed a perioperative mortality rate of 11.6% and a postoperative complication rate of 30%, which is significantly higher than what would be expected in patients without liver disease[16].
The significant perioperative risks associated with surgery in patients with cirrhosis highlight the importance of preoperative assessment and appropriate patient selection for surgery. The Child-Turcotte-Pugh (CTP or “Child”) classification was initially designed to evaluate the risk of surgical portosystemic shunt procedures, and was subsequently found to predict long-term survival in patients with cirrhosis[17]. Interestingly, the more recently devised prognostic scoring system used in patients with cirrhosis, namely the Model for End-stage Liver Disease (MELD) score was also originally designed for the purpose of selection of cirrhotic patients for a portosystemic shunt procedure-the transjugular intrahepatic portosystemic shunt (TIPS)[18]. Whereas the CTP class has traditionally been used in preoperative risk stratification in cirrhotic patients undergoing surgery, the MELD score was found to be superior to the CTP score and class in predicting three-month survival in patients with cirrhosis[19].
There has been a recent interest in evaluating the role of the MELD score in preoperative risk assessment, with a number of recent publications on the subject[20–24]. The purpose of our study is to determine factors affecting the outcome of patients with cirrhosis undergoing surgical procedures under general anesthesia and to compare the capacities of the CTP and MELD scores in predicting that outcome.
We conducted a retrospective review of the charts of patients with cirrhosis undergoing surgical procedures under general anesthesia between January 1999 and December 2004 at two teaching hospitals, Emory University Hospital and Emory Crawford Long Hospital.
We used the computerized medical record system to screen charts for “liver cirrhosis” and “general anesthesia” using billing codes and International Classification of Diseases-9 codes. Patients in whom the chart review did not reveal documented cirrhosis were excluded. Patients were considered to have documented cirrhosis if they had a liver biopsy confirming cirrhosis, an intra-operative finding of a cirrhotic liver during laparotomy or laparoscopy, or a combination of imaging and laboratory profiles consistent with cirrhosis. Patients undergoing surgical procedures directly involving the liver, such as liver transplantation, hepatectomy and transjugular intrahepatic portosystemic shunts were excluded. Patients for whom the preoperative CTP or MELD score could not be computed because of insufficient data were also excluded. Approval of the protocol by the Institutional Review Board of Emory University was obtained prior to the conduction of the study. The protocol conforms with the provisions of the declaration of Helsinki as revised in Edinburgh in 2000.
Preoperative history, physical examination and laboratory values were used to calculate the CTP and MELD scores. Surgical procedures were classified by organ system and by whether the procedures are urgent or elective. Surgery was considered to be elective if the procedures could reasonably have been scheduled at a later date without the need for hospitalization in the interim. Procedures not satisfying this criterion were classified as urgent procedures. Patients were followed up for 30 post-procedure days.
The primary endpoint for the purpose of our study was the occurrence of death or hepatic decompensation during the follow-up period. Hepatic decompensation was defined as the occurrence of both clinical decompensation and biochemical evidence of worsening liver function. Occurrences of new or worsening ascites, new or worsening encephalopathy, or variceal bleeding during the follow-up period were considered to be an evidence of clinical decompensation. A rise in the international normalized ratio (INR) or bilirubin in combination with clinical decompensation was required for the endpoint to be reached.
Patient characteristics were tallied both overall and by achievement of the endpoint of death or hepatic decompensation, and descriptive statistics were calculated. Two-sample t-tests were used to compare means of the continuous measures between the endpoint groups. To compare categorical summaries, the chisquare test of independence was used. Where expected counts were too low, Fisher’s exact test was employed. The Cochran-Armitage Test for Trend was used to examine the score system and endpoint relationships across ordinal Child classifications (A, B, C) and MELD tertiles.
These tests revealed that both score systems and procedure urgency were important factors in predicting death or decompensation. In order to more precisely quantify the roles of these variables in predicting the endpoint, a logistic regression was performed with urgency and classification score (either MELD or CTP) as independent variables, and the combined endpoint as a dependent variable. To avoid multicollinearity, the CTP and MELD scale were included in separate models.
To further characterize the relationships between score, urgency and the endpoint, we used a two-factor analysis of variance (ANOVA) to compare mean CTP and MELD scores for a model which included urgency, endpoint achievement, and their interaction.
These analyses showed that the scores significantly differed only within the urgent patient population. This directed our use of receiver-operating characteristic (ROC) plots to examine the relationship between score and patient outcome for the urgent-procedure population only. Predictive values for each scale were assessed by measuring the area under the curve (AUC). The AUCs for the CTP and MELD systems were compared using the method proposed by DeLong et al[25] for two correlated ROC curves. All analyses were performed using SAS software version 9.1 (SAS Institute Inc., Cary, NC). The correlated AUC test was implemented using the ROC SAS macro provided by DeLong et al[26].
A total of 617 patients were identified on initial screening. Of the initial group of patients, 258 had documented cirrhosis. Forty-five patients were excluded for undergoing liver-related surgery, and 18 patients were excluded because of insufficient data. A total of 195 patients were included in the study.
Patients were mostly white with a male predominance. The mean patient age was 57.1 years. Hepatitis C was the leading etiology of cirrhosis, followed by cryptogenic cirrhosis and alcoholic cirrhosis. Most patients were CTP class B, with a mean ± SD CTP score of 8.0 ± 1.9. The mean ± SD MELD score was 14.2 ± 6.3 (Table 1). The most commonly performed procedures were gastrointestinal. A total of 138 procedures were classified as elective and 57 as urgent. The procedures performed are detailed in Table 2.
| Total (n =195) | Death or decompensation | P value | Odds ratio | ||
| No (n = 163) | Yes (n = 32) | ||||
| Mean age (yr) | 57.1 ± 11.2 | 57.2 ± 10.9 | 56.5 ± 12.5 | 0.73 | |
| Gender, n (%) | |||||
| Female | 79 (40.5) | 65 (39.9) | 14 (43.8) | ||
| Male | 116 (59.5) | 98 (60.1) | 18 (56.3) | 0.68 | |
| Ethnicity, n (%) | |||||
| White | 159 (81.5) | 135 (82.8) | 24 (75.0) | ||
| African American | 27 (13.8) | 20 (12.3) | 7 (21.9) | 0.32 | |
| Other | 9 (4.6) | 8 (4.9) | 1 (3.1) | ||
| Etiology, n (%) | |||||
| Hepatitis C | 73 (37.4) | 61 (37.2) | 12 (37.5) | 0.99 | |
| Cryptogenic | 51 (26.2) | 43 (26.4) | 8 (25.0) | 0.87 | |
| Alcohol | 35 (17.9) | 26 (16.0) | 9 (28.1) | 0.1 | |
| Hepatitis B | 7 (3.6) | 7 (4.3) | 0 (0.0) | - | |
| Autoimmune hepatitis | 5 (2.6) | 5 (3.1) | 0 (0.0) | - | |
| Primary sclerosing cholangitis | 5 (2.6) | 4 (2.5) | 1 (3.1) | - | |
| Primary biliary cirrhosis | 4 (2.1) | 4 (2.5) | 0 (0.0) | - | |
| A1 antitrypsin deficiency | 3 (1.5) | 3 (1.8) | 0 (0.0) | - | |
| Non-alcoholic steatohepatitis | 2 (1.0) | 2 (1.2) | 0 (0.0) | - | |
| Amyloidosis | 2 (1.0) | 2 (1.2) | 0 (0.0) | - | |
| Hemochromatosis | 1 (0.5) | 1 (0.6) | 0 (0.0) | - | |
| Cardiac cirrhosis | 1 (0.5) | 1 (0.6) | 0 (0.0) | - | |
| Cystic fibrosis | 1 (0.5) | 0 (0.0) | 1 (3.1) | - | |
| Unknown | 5 (2.6) | 4 (2.4) | 1 (3.1) | - | |
| Mean CTP score ± SD | 8.0 ± 1.9 | 7.8 ± 1.8 | 9.1 ± 1.9 | 0.00058 | |
| CTP class n (%) | |||||
| A | 41 (21.0) | 40 (24.5) | 1 (3.1) | 1 | |
| B | 115 (59.0) | 95 (58.3) | 20 (62.5) | 0.0018 | 8.42 |
| C | 39 (20.0) | 28 (17.2) | 11 (34.4) | 15.71 | |
| Mean MELD score ± SD | 14.2 ± 6.3 | 13.2 ± 5.2 | 19.1 ± 5.2 | < 0.0001 | |
| MELD score (Tertile) | |||||
| 6-11 (T1) | 77 (47.2) | 6 (18.8) | 1 | ||
| 12-15 (T2) | 46 (28.2) | 10 (31.3) | 0.0008 | 2.79 | |
| 16-40 (T3) | 40 (24.5) | 16 (50.0) | 5.13 | ||
| Surgery sites | |||||
| Gastrointestinal | 101 (51.8) | 84 (51.5) | 17 (53.1) | 0.87 | |
| Cardiovascular and thoracic | 28 (14.4) | 22 (13.5) | 6 (18.8) | 0.42 | |
| Genitourinary | 24 (12.3) | 22 (13.5) | 2 (6.3) | 0.38 | |
| Orthopedic | 24 (12.3) | 20 (12.3) | 4 (12.5) | - | |
| Head and neck | 18 (9.2) | 15 (9.2) | 3 (9.4) | - | |
| Surgery type | |||||
| Urgent | 57 (29.2) | 36 (22.1) | 21 (65.6) | ||
| Elective | 138 (70.8) | 127 (77.9) | 11 (34.4) | < 0.0001 | |
| Total | Elective | Urgent | |
| Procedures | 195 | 138 | 57 |
| Gastrointestinal | 101 | 66 | 35 |
| Hernia repair | 34 | 21 | 13 |
| Cholecystectomy | 23 | 17 | 6 |
| Exploratory/diagnostic | 10 | 6 | 4 |
| Biopsy of lesion | 9 | 9 | 0 |
| Colectomy | 6 | 3 | 3 |
| Abscess drainage | 3 | 1 | 2 |
| Hemorrhoid ligation | 3 | 2 | 1 |
| Pancreatectomy | 3 | 3 | 0 |
| Small bowel resection | 3 | 0 | 3 |
| Peptic ulcer oversewing | 2 | 0 | 2 |
| Appendectomy | 1 | 0 | 1 |
| Antrectomy (Billroth II) | 1 | 1 | 0 |
| Gastric bypass | 1 | 1 | 0 |
| Gastrostomy tube placement | 1 | 1 | 0 |
| Splenectomy | 1 | 1 | 0 |
| Cardiovascular and thoracic | 28 | 25 | 3 |
| Coronary artery bypass | 5 | 5 | 0 |
| Video-assisted thoracoscopic surgery | 5 | 4 | 1 |
| Abdominal aortic aneurysm repair | 4 | 4 | 0 |
| Arteriovenous fistula/graft construction | 4 | 4 | 0 |
| Cardiac valve replacement/repair | 3 | 3 | 0 |
| Lung biopsy, open | 3 | 3 | 0 |
| Pericardiectomy | 2 | 0 | 2 |
| Heart transplant | 1 | 1 | 0 |
| Pulmonary lobectomy | 1 | 1 | 0 |
| Genitourinary | 24 | 21 | 3 |
| Cystoscopy/ureteroscopy | 15 | 12 | 3 |
| Dilation and curettage | 4 | 4 | 0 |
| Hysterectomy | 3 | 3 | 0 |
| Oophorectomy | 1 | 1 | 0 |
| Transurethral resection of prostate | 1 | 1 | 0 |
| Orthopedic | 24 | 12 | 12 |
| Total hip replacement | 6 | 6 | 0 |
| Amputation | 5 | 3 | 2 |
| Infected hip prosthesis removal | 4 | 0 | 4 |
| Incision and drainage | 4 | 0 | 4 |
| Open reduction - internal fixation | 3 | 2 | 1 |
| Arthroscopy | 2 | 1 | 1 |
| Head and neck | 18 | 14 | 4 |
| Endoscopic sinus surgery | 3 | 3 | 0 |
| Laryngoscopy | 3 | 3 | 0 |
| Parathyroidectomy | 3 | 3 | 0 |
| Craniotomy | 2 | 1 | 1 |
| Facial fracture reduction | 1 | 0 | 1 |
| Mastoidectomy | 1 | 1 | 0 |
| Neck dissection | 1 | 1 | 0 |
| Parotidectomy | 1 | 1 | 0 |
| Scleral buckle | 1 | 1 | 0 |
| Teeth extraction | 1 | 0 | 1 |
| Ventriculo-peritoneal shunt | 1 | 0 | 1 |
Seventeen (8.7%) patients died during follow-up and 28 (14.4%) patients had evidence of hepatic decompensation. Among the 17 patients who died, 13 (76.5%) had evidence of hepatic decompensation as well. A total of 32 patients (16.4% of the total, 21/57 patients in the urgent surgery group and 11/138 patients in the elective surgery group) reached the study endpoint of death or decompensation in the postoperative period. The causes of death were sepsis in 47.1% (8/17), gastrointestinal bleeding in 23.6% (4/17), and sudden cardiac arrest in 5.9% (1/17) cases. The cause of death was unknown in 4 patients. New or worsening hepatic encephalopathy was observed in 20 (10.3%) patients, new or worsening ascites in 9 (4.6%) patients, and variceal bleed in 8 (4.1%) patients.
Bivariate analyses revealed a significantly different trend between the proportion of patients that reached the study endpoint in each MELD tertile, as well as each CTP class (P = 0.0008 for MELD, P = 0.0018 for CTP). Those who experienced death or decompensation tended to be in the higher score classifications. Patients who reached the endpoint were also more likely to have had an urgent procedure (P < 0.0001). No inter-group difference was found in the other baseline characteristics (Table 1). Logistic regression analyses revealed that the MELD score, CTP score and the urgency of the procedure were significantly associated with the study endpoint (Table 3).
| Odds ratio | 95% CI | P | |
| A: MELD model | |||
| MELD (1 unit increase) | 1.1 | [1.03-1.17] | 0.0044 |
| MELD (5 unit increase) | 1.58 | [1.16-2.19] | |
| Elective (no vs yes) | 4.34 | [1.81-10.71] | 0.0011 |
| B: CTP model | |||
| CTP (1 unit increase) | 1.25 | [1.00-1.57] | 0.0554 |
| Elective (no vs yes) | 5.18 | [2.20-12.22] | 0.0002 |
Among patients undergoing elective surgical procedures, no statistically significant difference was noted in the mean ± SD MELD score (12.8 ± 3.9 vs 12.6 ± 4.7, P = 0.9) or in the mean ± SD CTP score (7.6 ± 1.2 vs 7.7 ± 1.7, P = 0.8) between patients who reached the endpoint and patients who did not. Conversely, both the mean ± SD MELD score and mean CTP score were higher in patients reaching the endpoint in the case of urgent procedures (MELD: 22.4 ± 8.7 vs 15.2 ± 6.4, P = 0.0007; CTP: 9.9 ± 1.8 vs 8.5 ± 1.8, P = 0.008, Figure 1).
When evaluating the capacities of the CTP and MELD scores to predict the occurrence of the study endpoint in the 57 patients undergoing urgent surgical procedures, the performances of both scoring systems were found to be fair: the area under the receiver operating characteristics curve (AUC) for MELD was 0.755 ± 0.066, the AUC for CTP was 0.696 ± 0.070 (Figure 2A and B). No statistically significant difference was found between the AUC for MELD and the AUC for CTP for these patients (P = 0.20, Figure 2C). A MELD score of 17 had a sensitivity of 71% and a specificity of 72% in predicting the outcome of death or decompensation in urgent surgical procedures. A CTP score of 9 had a sensitivity of 81% and specificity of 47% in predicting the outcome. Among the patients undergoing urgent surgical procedures, none of the 15/57 patients with a preoperative MELD score of ≤ 11 and none of the 15/57 patients with a preoperative CTP score of ≤ 7 had any evidence of death or hepatic decompensation in the post-operative period.
Gastroenterologists and hepatologists are often asked to evaluate patients with cirrhosis prior to undergoing non-liver-related surgical procedures for an opinion about the perioperative risk entailed and potential ways to reduce that risk. Unfortunately, the available evidence to support answers to these questions is relatively limited and is uniformly based on retrospective data.
Early studies addressing preoperative evaluation in cirrhosis identified the Child-Pugh score as a useful preoperative parameter in predicting surgical risk in patients undergoing abdominal surgery with a mortality rate of 10% for Child class A patients, 30%-31% for Child class B, and 76%-82% for Child class C patients[2728]. Compared to the Child score, the MELD score has an advantage of relying entirely on objective parameters for its computation, since it does not require an evaluation of the degree of ascites and the degree of encephalopathy. Also, the MELD score is a variable with a wider range of possible numeric values (6 to 40 for MELD compared to 5 to 15 for Child), thereby potentially allowing a better discrimination between patients with different degrees of hepatic dysfunction. Perkins et al[22] did not find a difference in the performances of the MELD score and the Child score in predicting the morbidity of cholecystectomy in 33 patients with cirrhosis. The authors favored the use of the MELD score because it is more objectively defined, and suggested a MELD score of 8 as a cut-off point that predicts an increased morbidity. Data about the urgency of the procedure was not provided[22]. In evaluating the outcome of 66 patients with cirrhosis undergoing predominantly elective cardiac surgery, Suman et al[21] found that the Child score and the MELD score were comparable in predicting the occurrence of hepatic decompensation in the postoperative period. The Child score cut-off point of 7, however, had a higher sensitivity in predicting mortality than a MELD cut-off of 13. In reviewing their experience with cardiac surgery in 27 patients with cirrhosis, Filsoufi et al[29] noted that the Child score was a better predictor of hospital mortality than the MELD score. On the other hand, Befeler et al[23] found the MELD score to be a better predictor of poor outcome than the Child class in 53 cirrhotic patients undergoing abdominal surgery, although in this case the MELD score was compared to Child class categories, and not to the numeric value of the Child score.
Our study included 195 patients with documented cirrhosis undergoing various surgical procedures under general anesthesia. The patients included in our study had fairly advanced liver disease with 57.4% of patients having a MELD score ≥ 12 and 79% being Child class B or C. The operative mortality (8.7%) that we observed is similar to the mortality observed in a large series of patients with cirrhosis undergoing surgery[16].
We found the urgency of the procedure to be a powerful predictor of the outcome, with the occurrence of the combined endpoint of death or hepatic decompensation being observed more than 4 times more often in the patients undergoing urgent surgery compared to the patients undergoing elective surgery. This effect persisted when controlling for the MELD or Child score in multivariate analysis (Table 3). Furthermore, when the data was stratified by the urgency of the procedure, neither the MELD nor the Child score was able to predict the outcome of elective surgery. This may be due to the lower event rate in patients undergoing elective surgery, as might be expected. It is conceivable as well that if a larger number of patients were included, the MELD score and Child score might have had a better discriminatory ability in predicting the outcome of elective surgery. This finding emphasizes, however, the importance of making a distinction between elective procedures and urgent procedures when studying the effect of variables on surgical outcome in patients with cirrhosis. In prior similar studies addressing predictors of operative outcomes in cirrhotic patients, this important distinction was not always made.
In the group of patients undergoing urgent surgery, the MELD score and Child score performed equally in predicting the occurrence of death or hepatic decompensation in the postoperative period. The performance of both scoring systems was only fair in that regard, with an AUC of 0.755 for MELD and 0.696 for Child, which is reflected in the lack of a cut-off point with both a high sensitivity and a high specificity in predicting the outcome for either scoring system. This is unlike the case of other studies where higher AUCs were noted[2122]. Studies with higher AUC values had studied specific surgical procedures, and the reason for the lower AUC in our study is likely to be the fact we studied a variety of procedures with different inherent risks to the patient. This problem could be circumvented by devising a classification system of surgical procedures by their inherent risk to patients with liver dysfunction, similar to the established system used in the case of perioperative risk assessment in cardiovascular disease[30]. In their seminal study on perioperative risk in patients with cirrhosis, Ziser et al[16] provided some useful guidance in this direction; however, this remains an area in need of further study.
We noted that among patients in our study undergoing urgent surgery with either a MELD score ≤ 11 or a Child ≤ 7, none had evidence of death or decompensation postoperatively. Patients falling into this low-risk category represented a substantial proportion (20/57, 35.1%) of the total number of patients undergoing urgent surgery, suggesting that these cut-off points may be useful in practice.
It is likely that the role of preoperative evaluation in patients with cirrhosis is more critical in the case of elective surgical procedures than it is in the case of urgent procedures. In many instances, patients undergoing urgent surgery may have no reasonable alternative to surgery, and may have little time for any preoperative intervention that could potentially reduce the risk of complications. Therefore, the best opportunity for Gastroenterologists or Hepatologists to intervene in a manner that may reduce surgical risk or to provide useful guidance as to whether or not to proceed with surgery is probably in the case of elective surgery rather than urgent surgery. We could not demonstrate that MELD score and Child score were helpful in determining the outcome of elective surgery. Furthermore, larger studies are needed to better define the roles of the Child and MELD scores in predicting the outcome of surgical procedures in patients with cirrhosis, particularly in the case of elective surgery.
Patients with cirrhosis who undergo surgeries under general anesthesia are at an increased risk of complications. The Child-Turcotte-Pugh (CTP) class has been used to assess the risk of surgery in patients with cirrhosis. The model for end-stage liver disease (MELD) score is a more recently devised tool to assess the severity of liver disease.
Previous studies comparing the CTP score and the MELD score in predicting the outcome of surgery in cirrhosis yielded variable results, generally pointing in the direction of both scoring systems being good predictors of the outcome of non-hepatic surgery in cirrhosis. Only few studies made the distinction between elective and urgent surgery.
The urgency of the surgical procedure was found to be a major predictor of the outcome, with the complication rate of elective procedures being generally low. In elective procedures, the CTP score and MELD score were not predictive of the outcome. In urgent procedures, the MELD score and CTP score performed equally in predicting an adverse outcome.
The MELD score and CTP score could be used alternatively in evaluating the risk of an urgent surgical procedure. Studies are needed to assess the risk of elective procedures in patients with cirrhosis.
The CTP and MELD scores are both measures of the severity of liver disease in cirrhosis. The MELD score is computed entirely using objective laboratory data. The computation of the CTP scores requires an assessment of non-objective parameters, including the severity of ascites and of encephalopathy.
In this retrospective study, the authors determined the factors affecting the outcome of surgeries under general anesthesia in patients with cirrhosis and compared the capacities of the CTP and MELD scores to predict that outcome. They concluded that CTP and MELD scores performed equally, but only fairly in predicting the outcome of urgent surgical procedures.
| 1. | Friedman LS. The risk of surgery in patients with liver disease. Hepatology. 1999;29:1617-1623. |
| 2. | Maze M, Bass NM. Anesthesia and the Hepatobiliary System. Anesthesia. 5th ed. Edinburgh: Churchill Livingstone 2000; 1960-1973. |
| 3. | Ngai SH. Effects of anesthetics on various organs. N Engl J Med. 1980;302:564-566. |
| 4. | Strunin L. Anesthetic management of patients with liver disease. Liver and Biliary Disease. London: Saunders 1992; 1381-1391. |
| 5. | Batchelder BM, Cooperman LH. Effects of anesthetics on splanchnic circulation and metabolism. Surg Clin North Am. 1975;55:787-794. |
| 6. | Gelman S. General anesthesia and hepatic circulation. Can J Physiol Pharmacol. 1987;65:1762-1779. |
| 7. | Walton B, Simpson BR, Strunin L, Doniach D, Perrin J, Appleyard AJ. Unexplained hepatitis following halothane. Br Med J. 1976;1:1171-1176. |
| 8. | Kenna JG. Immunoallergic drug-induced hepatitis: lessons from halothane. J Hepatol. 1997;26 Suppl 1:5-12. |
| 9. | Berghaus TM, Baron A, Geier A, Lamerz R, Paumgartner G. Hepatotoxicity following desflurane anesthesia. Hepatology. 1999;29:613-614. |
| 10. | Rosenberg PM, Friedman LS. The liver in circulatory failure. 8th ed. Philadelphia: Lippincott-Raven 1999; 1215-1227. |
| 11. | Hayashida N, Shoujima T, Teshima H, Yokokura Y, Takagi K, Tomoeda H, Aoyagi S. Clinical outcome after cardiac operations in patients with cirrhosis. Ann Thorac Surg. 2004;77:500-505. |
| 12. | Cohen SM, Te HS, Levitsky J. Operative risk of total hip and knee arthroplasty in cirrhotic patients. J Arthroplasty. 2005;20:460-466. |
| 13. | Metcalf AM, Dozois RR, Wolff BG, Beart RW Jr. The surgical risk of colectomy in patients with cirrhosis. Dis Colon Rectum. 1987;30:529-531. |
| 14. | Puggioni A, Wong LL. A metaanalysis of laparoscopic cholecystectomy in patients with cirrhosis. J Am Coll Surg. 2003;197:921-926. |
| 15. | Lund L, Jepsen P, Vilstrup H, Sorensen HT. Thirty-day case fatality after nephrectomy in patients with liver cirrhosis--a Danish population-based cohort study. Scand J Urol Nephrol. 2003;37:433-436. |
| 16. | Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42-53. |
| 17. | Child CG, Turcotte JG. Surgery and portal hypertension. The Liver and Portal Hypertension. Philadelphia: Saunders 1964; 50-58. |
| 18. | Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-871. |
| 19. | Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-96. |
| 20. | Farnsworth N, Fagan SP, Berger DH, Awad SS. Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg. 2004;188:580-583. |
| 21. | Suman A, Barnes DS, Zein NN, Levinthal GN, Connor JT, Carey WD. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol. 2004;2:719-723. |
| 22. | Perkins L, Jeffries M, Patel T. Utility of preoperative scores for predicting morbidity after cholecystectomy in patients with cirrhosis. Clin Gastroenterol Hepatol. 2004;2:1123-1128. |
| 23. | Befeler AS, Palmer DE, Hoffman M, Longo W, Solomon H, Di Bisceglie AM. The safety of intra-abdominal surgery in patients with cirrhosis: model for end-stage liver disease score is superior to Child-Turcotte-Pugh classification in predicting outcome. Arch Surg. 2005;140:650-654; discussion 655. |
| 24. | Cucchetti A, Ercolani G, Vivarelli M, Cescon M, Ravaioli M, La Barba G, Zanello M, Grazi GL, Pinna AD. Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis. Liver Transpl. 2006;12:966-971. |
| 25. | DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837-845. |
| 26. | Nonparametric comparison of areas under correlated ROC curves. Available from: URL: http://support.sas.com/ctx/ samples/index.jsp?sid=520. Accessed November 28th, 2006. |
| 27. | Garrison RN, Cryer HM, Howard DA, Polk HC Jr. Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199:648-655. |
| 28. | Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122:730-735; discussion 735-736. |
| 29. | Filsoufi F, Salzberg SP, Rahmanian PB, Schiano TD, Elsiesy H, Squire A, Adams DH. Early and late outcome of cardiac surgery in patients with liver cirrhosis. Liver Transpl. 2007;13:990-995. |
| 30. | Eagle KA, Berger PB, Calkins H, Chaitman BR, Ewy GA, Fleischmann KE, Fleisher LA, Froehlich JB, Gusberg RJ, Leppo JA. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery---executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation. 2002;105:1257-1267. |