Published online Mar 14, 2008. doi: 10.3748/wjg.14.1514
Revised: January 28, 2008
Published online: March 14, 2008
AIM: To investigate if transnasal endoscopic retrograde cholangiopancreatography (n-ERCP) using an ultrathin forward-viewing scope may overcome the disadvantages of conventional oral ERCP (o-ERCP) related to the large-caliber side-viewing duodenoscope.
METHODS: The study involved 50 patients in whom 25 cases each were assigned to the o-ERCP and n-ERCP groups. We compared the requirements of esophagogastroduodenoscopy (EGD) prior to ERCP, rates and times required for successful cannulation into the pancreatobiliary ducts, incidence of post-procedure hyperamylasemia, cardiovascular parameters during the procedure, the dose of a sedative drug, and successful rates of endoscopic naso-biliary drainage (ENBD).
RESULTS: Screening gastrointestinal observations were easily performed by the forward-viewing scope and thus no prior EGD was required in the n-ERCP group. There was no significant difference in the rates or times for cannulation, or incidence of hyperamylasemia between the groups. However, the cannulation was relatively difficult in n-ERCP when the scope appeared U-shape under fluoroscopy. Increments of blood pressure and the amount of a sedative drug were significantly lower in the n-ERCP group. ENBD was successfully performed succeeding to the n-ERCP in which mouth-to-nose transfer of the drainage tube was not required.
CONCLUSION: n-ERCP is likely a well-tolerable method with less cardiovascular stress and no need of prior EGD or mouth-to-nose transfer of the ENBD tube. However, a deliberate application is needed since its performance is difficult in some cases and is not feasible for some endoscopic treatments such as stenting.
- Citation: Mori A, Ohashi N, Maruyama T, Tatebe H, Sakai K, Shibuya T, Inoue H, Takegoshi S, Okuno M. Transnasal endoscopic retrograde chalangiopancreatography using an ultrathin endoscope: A prospective comparison with a routine oral procedure. World J Gastroenterol 2008; 14(10): 1514-1520
- URL: https://www.wjgnet.com/1007-9327/full/v14/i10/1514.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1514
Ultrathin endoscopy has been developed to perform unsedated transnasal esophagogastroduodenoscopy (EGD) as an alternative procedure to conventional oral endoscopy[1–6]. Although the evaluation of the ultrathin endoscope has not been established yet[7–10], it has been suggested that transnasal EGD with an ultrathin scope diminishes the cardiopulmonary complications, lowers the cost because of dispensability of post-procedure monitoring related to consciousness sedation, and improves the patient’s acceptability[1112]. We have also demonstrated that nasal EGD is better accepted by unsedated patients with less cardiovascular stress compared to conventional oral EGD[13–15].
Very recently, our preliminary studies have shown further application of an ultrathin upper endoscope to endoscopic retrograde cholangiopancreatography (ERCP) through the nasal[16] and gastric stomal routes[17]. Some complications of ERCP including cardiovascular stress may be related to a large-caliber endoscope[18] and furthermore a side-viewing scope usually used in ERCP is not feasible for the screening of esophagogastroduodenal tract. Thus, the use of an ultrathin forward-viewing scope for ERCP might be beneficial to lessen those disadvantages. In fact, we have shown that transnasal ERCP with an ultrathin scope decreased cardiovascular stress as compared to the conventional oral method[16]. Another advantage to use an ultrathin scope is no need of mouth-to-nose transfer of a drainage tube in performing endoscopic naso-biliary drainage (ENBD) because the scope is inserted via the transnasal approach[16]. Moreover, we as well as others have recently reported the direct cholangioscopy by utilizing an ultraslim endoscope for the diagnosis and treatment of choledocholithiasis[19–21].
Therefore, the application of an ultrathin endoscope to ERCP would be worthy of evaluation. However, limited information is available so far regarding transnasal ERCP with an ultrathin scope. Here, we report a prospective study to estimate the usefulness of an ultrathin scope in performing ERCP comparing to a conventional endoscope. We have used a transnasal method with an ultrathin scope, which may be advantageous in performing ENBD.
Fifty consecutive patients, who underwent ERCP for the diagnosis and treatment of the pancreatobiliary disorders in Inuyama Chuo Hospital between March 2006 and March 2007 (Table 1), were enrolled in the present study. The patients were assigned alternately to two groups: 25 patients each underwent either transnasal ERCP with an ultrathin endoscope (n-ERCP group) or transoral ERCP with a conventional scope (o-ERCP group). We excluded the patients with a history of esophagogastrointestinal surgery and cardiovascular diseases and those who were expected to undergo sphincterotomy, papillary balloon dilatation. All patients gave written informed consent before participating into the study. The study was performed in compliance with the Declaration of Helsinki and was approved by the review board for human research of our hospital.
| Groups | o-ERCP | n-ERCP | P-value |
| Number of patients | 25 | 25 | |
| Male/Female | 17/8 | 17/8 | 0.76 |
| Median age (range) | 69 (32-89) | 74 (35-85) | 0.07 |
| Systolic blood pressure (mmHg) | 129 ± 20 | 133 ± 19 | 0.50 |
| Pulse rate (/min) | 71 ± 12 | 65 ± 11 | 0.08 |
| SpO2 (%) | 99 ± 1.6 | 98 ± 1.6 | 0.35 |
| Indication for ERCP (n) | |||
| Cholecyst lithiasis | 6 | 2 | |
| Choledochus lithiasis | 11 | 10 | |
| Cancer | 6 | 10 | 0.50 |
| Pancreatitis | 1 | 2 | |
| Others | 1 | 1 |
ERCP was performed by three senior endoscopists with more than 10 years’ experience. Two types of endoscopes were used; an ultrathin endoscope (EG530N, Fujinon-Toshiba, Tokyo, Japan with an outer diameter of 5.9 mm, biopsy channel diameter of 2 mm and working length of 1100 mm; forward viewing 120 degree; tip deflection 210 degree up, 90 degree down, and 100 degree right and left) for the transnasal approach and a conventional duodenal endoscope (ED450XT8, Fujinon-Toshiba, Tokyo, Japan with an outer diameter of 13.5 mm) for the oral approach. The nasal cavity was prepared before transnasal ERCP by spraying three doses of 0.111% tramazoline hydrochloride (Alfresa Pharma, Osaka, Japan), followed by the insertion of an 18 Fr catheter covered with 8% lidocaine liquid (Astra Zeneca, Tokyo, Japan) for 3 min. Pharyngeal anesthesia was performed by lidocaine jelly (approximately 5 mL of 2% gel) before the oral endoscopy. Atropine sulfate (0.5 mg) and glucagon (1 USP) were given intramuscularly just before both procedures. Conscious sedation was carried out by an intravenous injection of midazolam (Astellas, Tokyo, Japan) during both ERCP procedures.
In performing n-ERCP, an ultrathin endoscope was inserted through the nasal cavity and reached the second or third portion of the duodenum after screening observations of the upper gastrointestinal tract. There was no difficulty in observing the papilla of Vater and the cannulation for cholangiopancreatography was performed using a conventional ERCP tube through the biopsy channel of the ultrathin scope as reported previously[16]. In case of need, an ERCP tube was easily replaced by an ENBD tube (ENBD-5-NAG, Cook, Bloomington, USA) using a guide-wire (Jagwire 0.025/450 Boston Scientific, Natick, USA). Thereafter, the scope was withdrawn carefully through the nasal cavity, leaving the ENBD catheter in the bile duct.
We have compared between the two procedures the rates of successful cannulation into the common bile duct and/or pancreatic duct, the times required for the first cannulation into either of the ducts, the doses of the sedative drug, the incidence of post-procedural hyperamylasemia and the successful rates of ENBD. The patients with increased serum amylase levels more than twice of normal range after two hours of ERCP were diagnosed hyperamylasemia.
Pulse (P), systolic blood pressure (BP) and peripheral blood oxygen saturation (SpO2) were measured using a monitor unit (DS-7100 Dynascope, Fukuda Denshi, Nagoya, Japan) at the right upper arm. The parameters were determined at rest before the examination, just before the cannulation of the papilla of Vater and at the completion of the procedure. Patients lay quietly in the prone position during the procedure. The rate-pressure product was calculated by a multiplication of BP and P. Changes of the parameters (ΔP, ΔBP, ΔSpO2 and Δrate-pressure product) were calculated by the following equation: (values during the endoscopy) - (values before the endoscopy).
According to our preliminary study[16], the required sample size was estimated for α = 5% (two-sided) and β = 10% as well as concerning a risk of cannulation failure in n-ERCP (approximately 30%). With the aim of detecting a standardized difference of 30 mmHg and a standard deviation of 25 mmHg in ΔBP, a sample size of 25 patients per group was needed.
Results were expressed by a median value and interquartile as well as 10%-90% quantity range for nonparametric data, and by a mean ± SD and mean ± SE for parametric data. Statistical analysis was carried out using Welch-t test or paired t-test as a parametric test for P, BP, SpO2 and changes of the parameters. Mann-Whitney-U test and chi-squared test were used for as a nonparametric data and categorical data. All analyses were performed with the SPSS for Windows (SPSS Japan, Tokyo, Japan). A P value less than 0.05 was considered significant.
No significant difference was found in the gender, age or types of diseases between the two groups (Table 1). Requirement of EGD prior to ERCP is shown in Table 2. It is notable that no prior EGD was needed in the n-ERCP group, whereas EGD was routinely performed before ERCP in all the cases in the o-ERCP group in order to avoid the gastrointestinal injury possibly caused by the side-viewing scope. The diagnoses with the screening EGD involved not a few numbers (approximately 20%) of the esophageal disorders that would be difficult to find by a side-viewing scope (Table 2).
| Groups | o-ERCP | n-ERCP |
| Number of patients | 25 | 25 |
| EGD prior to ERCP | 25 | 0 |
| Diagnosis | ||
| Normal finding | 8 | 10 |
| Pathological findings | 17 | 15 |
| Reflux esophagitis | 1 | 2 |
| Sliding hernia | 4 | 2 |
| Esophageal diverticulum | 1 | 0 |
| Atrophic gastritis | 10 | 11 |
| Duodenal ulcer scar | 1 | 4 |
| Gastric adenoma | 1 | 1 |
| Gastric SMT | 0 | 1 |
Procedure-related measurements are presented in Table 3. We have successfully performed n-ERCP in 23 of 25 cases (92%) except two cases with gallbladder cancer and choledocholithiasis due to the insertion failure of the endoscope into the second portion of the duodenum. In the n-ERCP group we have completed the cannulation into the common bile duct in 18 of 25 cases (72%) and into the pancreatic duct in 21 of 23 attempted cases (91%). There was no difference in the procedure time required for the cannulation between the groups (Table 3).
| Groups | o-ERCP | n-ERCP | P-value |
| Successful cannulation (%) | |||
| Either of the ducts | 25/25 | 23/25 | 0.510 |
| (100) | (92) | ||
| Common bile duct | 24/25 | 18/25 | 0.053 |
| (96) | (72) | ||
| Pancreatic duct | 24/25 | 21/23 | 0.940 |
| (96) | (91) | ||
| Median time for cannulation, min (%) | 8 | 7 | 0.590 |
| (2-24) | (4-20) | ||
| Post-procedural hyperamylasemia (%) | 7/25 | 5/23 | 0.870 |
| (28) | (22) | ||
| Successful ENBD (%) | 20/21 | 13/15 | 0.340 |
| (95) | (87) |
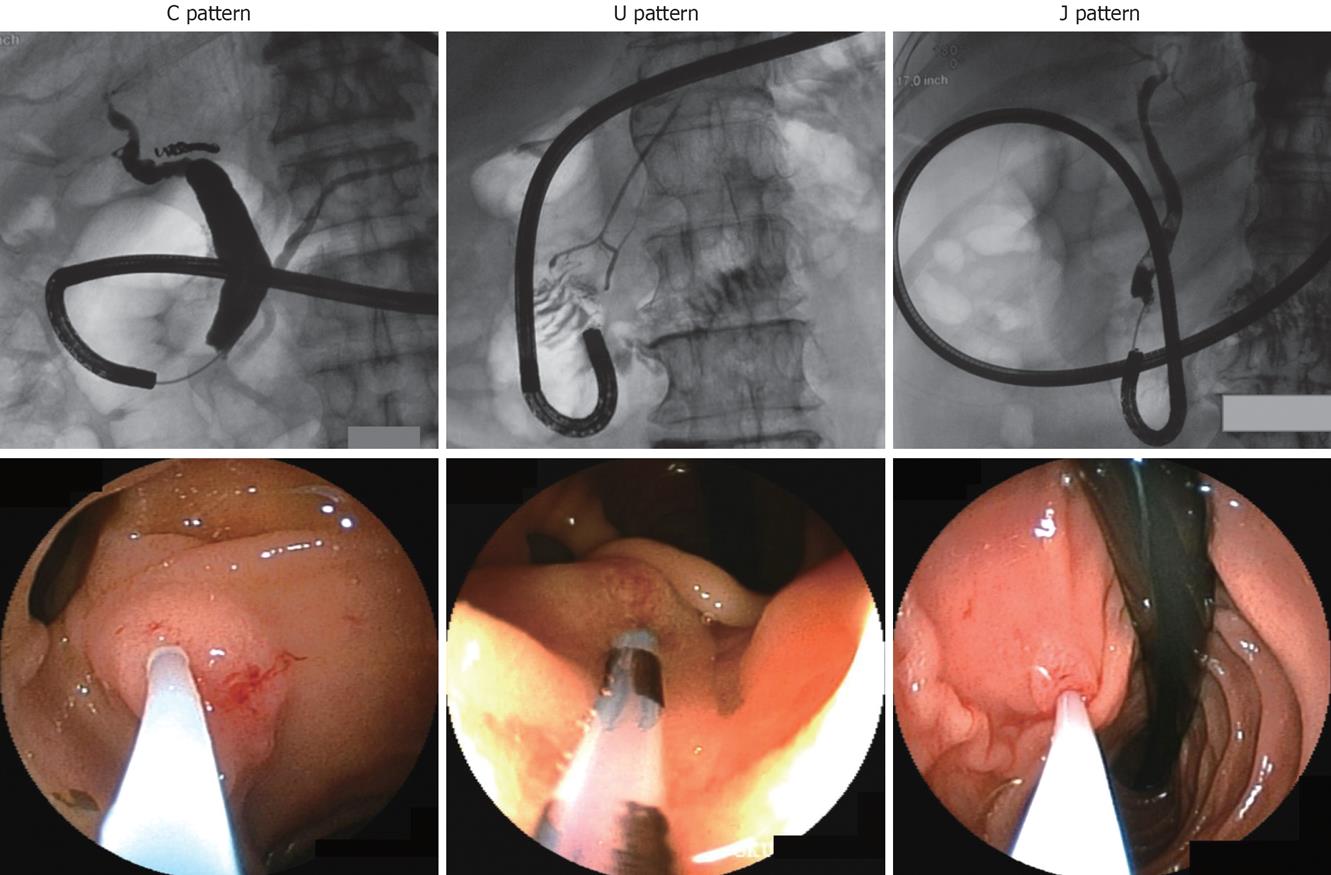
Although no significant difference was found in the rate of successful cannulation between the two groups, there was a tendency to a lower success rate of cannulation into the common bile duct in the n-ERCP group (Table 3). Therefore, we have further analyzed the relationship between the successful insertion rate and the patterns of endoscopic shapes during the approaches to the papilla of Vater. We have classified the manners of approaches into three categories: C, U and J patterns according to the endoscopic shape observed under fluoroscopy (Figure 1). In the C and U patterns the scope was inserted along the duodenal loop in the second and third portions. In the C pattern a front view of the papilla of Vater was observed easily, whereas in the U pattern its observation was more difficult, where the papilla could only be looked up from the third portion of the duodenum (Figure 1). The J pattern was the reverse shape of the U loop. The papilla of Vater was also looked up from the downward in the J pattern, however, its view was obtained more easily than in the U pattern. Favorable results were obtained in the C and J patterns regarding both the cannulation rates and its required times (Table 4). However, because in the U pattern the angle to observe the papilla of Vater was sharpest, we had difficulty in the cannulation, resulting in the lowest cannulation rate into the common bile duct as well as the longest time for cholangiography among the patterns (Table 4).
| Patterns | C | U | J | Total |
| Successful cannulation (%) | ||||
| Either of the ducts | 6 | 14 | 3 | 23 |
| Common bile duct | 6/6 | 9/14 | 3/3 | 18/23 |
| (100) | (64) | (100) | (78) | |
| Pancreatic duct | 5/5 | 14/14 | 2/2 | 21/21 |
| (100) | (100) | (100) | (100) | |
| Median time for cannulation, min (%) | ||||
| Either of the ducts | 6.5 | 7.3 | 7 | 7 |
| (5-8) | (4-20) | (4-14) | (4-20) | |
| Common bile duct | 10.5 | 20 | 16 | 17 |
| (8-37) | (7-35.5) | (6-19) | (6-37) | |
| Pancreatic duct | 6 | 13 | 6 | 9 |
| (5-8) | (6-26) | (5-7) | (5-26) | |
| Termination | 31 | 34 | 24 | 33 |
| (14-38) | (11-61) | (12-34) | (11-61) |
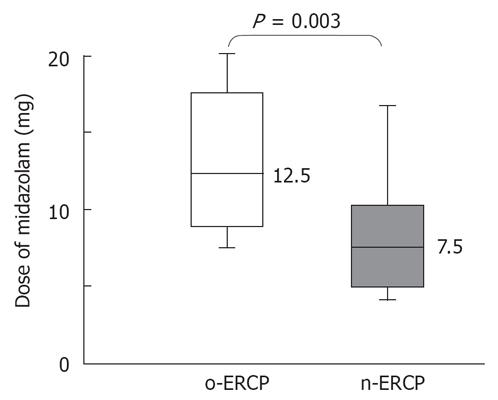
Post-procedural hyperamylasemia was found in 22% and 28% in the n-ERCP and o-ERCP groups, respectively, which was not significantly different (Table 3). Pancreatitis was not encountered in either procedure, suggesting no disadvantage of n-ERCP regarding procedure-associated complications. Interestingly, the dose of a sedative drug (midazolam) required during the procedure was significantly smaller in the n-ERCP group than in the o-ERCP group (P = 0.003, Figure 2). Insertion of an ENBD tube was attempted in 15 cases in the n-ERCP group and was successfully performed in 13 cases (87%), except two cases with the incomplete deep cannulation into the common bile duct (Table 3). No significant difference was found in the successful rate of ENBD between the groups.
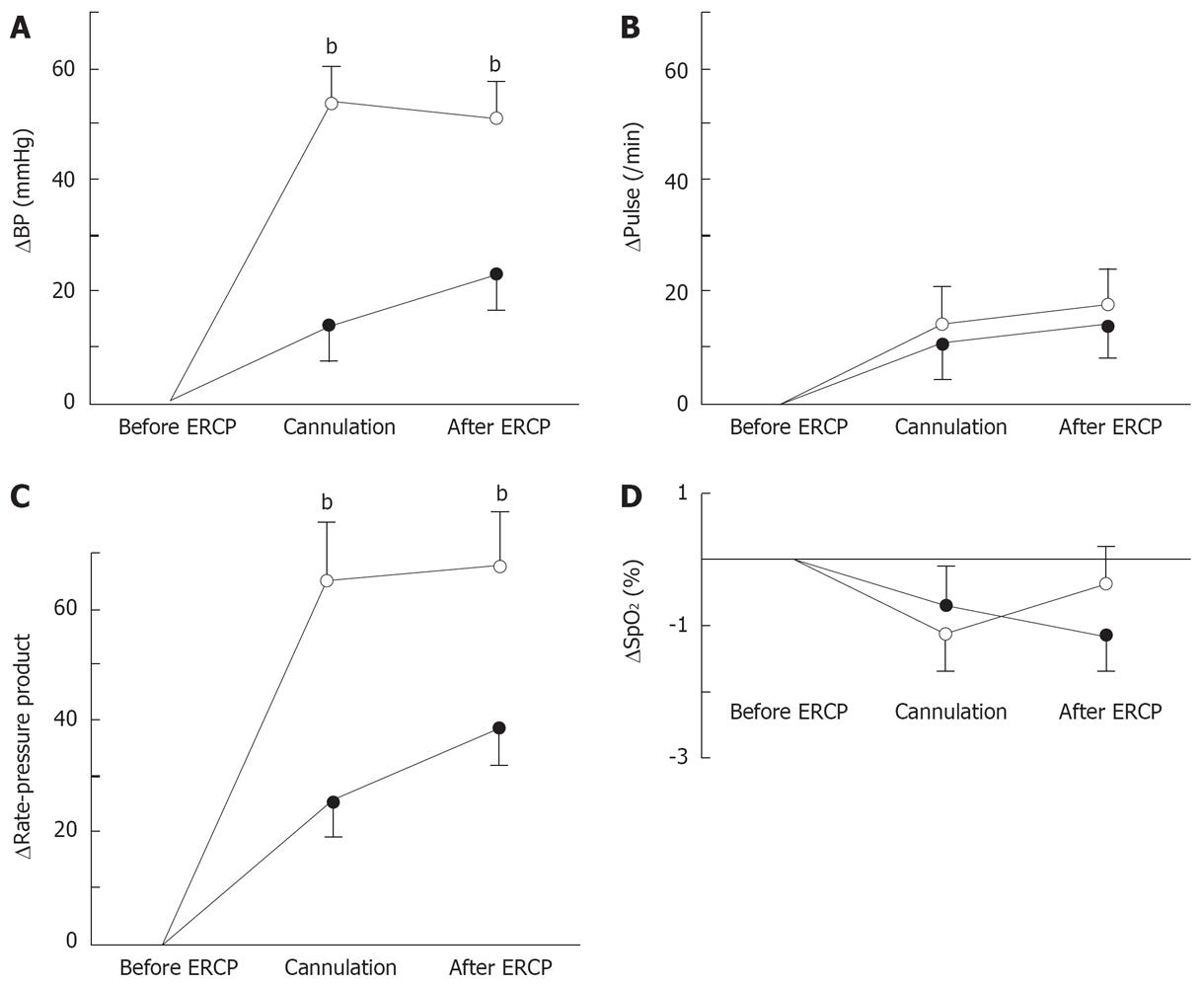
There was no significant difference in the baseline cardiovascular parameters measured before ERCP between the n-ERCP and o-ERCP groups (Table 1). Both ΔBP and Δrate-pressure product measurements just before the cannulation of the papilla of Varter and at the end of ERCP procedure were significantly smaller (P < 0.001, respectively) in the n-ERCP group than in the o-ERCP group (Figure 3A and C). There was no significant difference in ΔP (Figure 3B) and ΔSpO2 (Figure 3D) between the two groups both just before the cannulation and at the end of ERCP.
ERCP is a widespread technique essential for the diagnosis and treatment of the pancreatobiliary disorders. Although ERCP is an established method, there are still several disadvantages in its performance including the procedure-related morbidity[11]. Here, we have focused upon the following unfavorable aspects of the conventional ERCP: (1) a side-viewing duodenoscope is not suitable for the screening observation of the esophagogastroduodenal tract prior to performing ERCP, (2) a large caliber scope may exacerbate the cardiovascular stress, and (3) transfer of a drainage tube from the oral to nasal cavity is necessary in performing ENBD. We have investigated in the present study if those disadvantages could be overcome by the transnasal approach employing an ultrathin forward-viewing endoscope.
Most of the patients with acute pancreatobiliary disorders have the symptoms indistinguishable from those of the esophagogastrointestinal diseases and in fact the gastrointestinal complications are often encountered in such patients. Therefore, the observation with EGD prior to ERCP is preferable, as we have routinely performed in the present study. However, since a forward-viewing scope employed for n-ERCP is usually used to examine the upper gastrointestinal tract, additional EGD was not necessarily performed prior to n-ERCP. Simultaneous screening of the gastrointestinal tract may not only shorten the time required for the diagnosis but also assist performing safer ERCP by reducing a risk of the esophagogastroduodenal injuries that might occur during the conventional ERCP procedure with a side-viewing scope. Moreover, a forward-viewing scope has an advantage in examining the esophageal diseases that would be hardly diagnosed by a side-viewing scope. In fact, not a few numbers of esophageal diseases were found in the present study.
A large-caliber endoscope has been suggested to exacerbate cardiovascular stress[18]. Here, we have also shown that n-ERCP with an ultrathin scope reduced the cardiovascular stress as we have reported previously[16]. A significantly lower increment of the rate-pressure product in n-ERCP may strongly support the reduction of the risk of cardiovascular complications as compared to conventional o-ERCP[22]. Furthermore, we have found that n-ERCP required a significantly lower dose of the sedative drug than o-ERCP. These observations suggest the reduced physical as well as presumably less mental stress in performing n-ERCP. Previous studies have suggested that the sedative used during EGD is an important factor in the genesis of cardiopulmonary complications and thus milder sedation could diminish its incidence[1123]. Therefore, a lower requirement of a sedative drug in n-ERCP might also be advantageous to lessen the cardiovascular complications. In fact, n-ERCP with an ultrathin endoscope has been anticipated being advantageous to reduce myocardial ischemia because of its less mechanical irritation[24–27].
A guideline for the diagnosis and treatment of acute cholangitis and cholecystitis has recently been proposed in which an early biliary drainage is strongly recommended[28]. ENBD is a valuable and safe technique for the urgent biliary drainage. We have successfully performed ENBD in succession to n-ERCP without any complications. Because there is no need of EGD prior to ERCP, n-ERCP may be valuable in performing urgent ENBD. Another advantage of transnasal approach is no need to transfer the ENBD tube from oral to nasal cavity.
Those observations in our study suggest that n-ERCP is a well-tolerable technique that may overcome some disadvantages of conventional o-ERCP. However, it should be noted that there are significant limitations in performing n-ERCP due to a narrow channel of the scope. For instance, the technique is not feasible for sphincterotomy, papillary balloon dilatation, and stenting using a large-size stent with a diameter of 5 Fr or more. Therefore, we do understand the necessity and widespread utility of o-ERCP, and thus we do not intend to emphasize excessively the usefulness of n-ERCP. Moreover, in some cases n-ERCP is difficult to perform and thus would be better replaced with o-ERCP. Particularly, in cases with the U pattern of the endoscopic shape the successful cannulation rate was relatively low and requires a longer time, which might lead to an increased risk of the procedure-related complications such as acute pancreatitis[29] and ischemic heart injury[26]. Therefore, we propose the following strategy to perform n-ERCP in the clinical practice. In cases who are not expected to undergo sphincterotomy or papillary balloon dilatation, transnasal EGD is routinely performed prior to ERCP using an ultrathin scope that usually reaches the papilla of Vater. Then, when the approach pattern is C or J under fluoroscopy the cannulation for cholangiopancreatography seems to be easily and safely performed and thus n-ERCP may be attempted. However, in cases with the U pattern the scope may better be replaced with a conventional side-viewing duodenoscope when an endoscopist had difficulty in the cannulation. In addition, we have experienced successful n-ERCP in several cases in whom the papilla of Vater was hard to observe using a side-view scope and thus we failed to perform o-ERCP. N-ERCP may also be a good indication in such cases.
Future advancement of ERCP techniques using an ultrathin scope might allow the minimally invasive interventions that otherwise can hardly be carried out by conventional ERCP. For example, endoscopic diagnosis and therapy for the pancreatobiliary disorders may extend to the elderly as well as to the patients with difficulties in oral insertion, including those with esophagogastrointestinal stenosis and gastric stoma as we have reported previously[17]. Very recently, we have successfully performed lithotomy under direct cholangioscopy utilizing the same ultrathin scope used in the present study[1920]. Thus, it is possible to remove a biliary stone in succession to n-ERCP in cases who had undergone sphincterotomy. Future development of an ultrathin duodenoscope designed especially for ERCP would bring the wide spread of the transnasal ERCP.
Conventional oral endosccopic retrograde cholangiopancreatograpy (ERCP) has several disadvantages related to a large caliber side-viewing duodenoscope, including the cardiovascular stress caused by a large-caliber scope, difficulty in observing the esophagogastroduodenal tract prior to performing ERCP, and necessity of mouth-to-nose transfer in performing endoscopic naso-biliary drainage (ENBD). Transnasal upper endoscopy using an ultraslim scope has been shown to be better tolerated with less cardiovascular stress.
Very recently, our preliminary studies have shown the better cardiovascular tolerance of transnasal ERCP using an ultraslim forward-viewing scope as well as an application of the scope to direct cholangioscopy. The highlight of the present study is to demonstrate the feasibility of the ultrathin scope in performing ERCP, comparing with conventional oral ERCP.
Little information has been available regarding the application of an ultrathin upper endoscope to ERCP. The present study is the first report showing the utility and safety of transnasal ERCP with an ultraslim scope. We have demonstrated that nasal ERCP can be performed safely with similar successful rates of cannulation into the pancreatobiliary ducts as compared with those of the conventional method, and that nasal ERCP is less stressful to the cardiovascular system and is advantageous in performing ENBD due to no necessity of mouth-to-nose transfer of a drainage tube.
ERCP using an ultrathin scope may allow endoscopic diagnosis and therapy for the pancreatobiliary disorders in patients with difficulties in insertion, including those with esophagogastroduodenal stenosis and gastric stoma. Future development of the ultrathin duodenoscope might bring the widespread of transnasal ERCP.
The present study is the first demonstration of the feasibility and safety of transnasal ERCP utilizing an ultraslim upper endoscope. The findings are novel and the study design is well organized.
| 1. | Faulx AL, Catanzaro A, Zyzanski S, Cooper GS, Pfau PR, Isenberg G, Wong RC, Sivak MV Jr, Chak A. Patient tolerance and acceptance of unsedated ultrathin esophagoscopy. Gastrointest Endosc. 2002;55:620-623. |
| 2. | Saeian K, Staff D, Knox J, Binion D, Townsend W, Dua K, Shaker R. Unsedated transnasal endoscopy: a new technique for accurately detecting and grading esophageal varices in cirrhotic patients. Am J Gastroenterol. 2002;97:2246-2249. |
| 3. | Saeian K, Townsend WF, Rochling FA, Bardan E, Dua K, Phadnis S, Dunn BE, Darnell K, Shaker R. Unsedated transnasal EGD: an alternative approach to conventional esophagogastroduodenoscopy for documenting Helicobacter pylori eradication. Gastrointest Endosc. 1999;49:297-301. |
| 4. | Dean R, Dua K, Massey B, Berger W, Hogan WJ, Shaker R. A comparative study of unsedated transnasal esophagogastroduodenoscopy and conventional EGD. Gastrointest Endosc. 1996;44:422-424. |
| 5. | Dumortier J, Napoleon B, Hedelius F, Pellissier PE, Leprince E, Pujol B, Ponchon T. Unsedated transnasal EGD in daily practice: results with 1100 consecutive patients. Gastrointest Endosc. 2003;57:198-204. |
| 6. | Preiss C, Charton JP, Schumacher B, Neuhaus H. A randomized trial of unsedated transnasal small-caliber esophagogastroduodenoscopy (EGD) versus peroral small-caliber EGD versus conventional EGD. Endoscopy. 2003;35:641-646. |
| 7. | Bajaj JS, Shaker R. Another indication for transnasal, unsedated upper-GI endoscopy. Gastrointest Endosc. 2005;62:667-668. |
| 8. | Botoman VA. Ultrathin crossroads: is smaller better? Gastrointest Endosc. 2003;57:377-380. |
| 9. | Birkner B, Fritz N, Schatke W, Hasford J. A prospective randomized comparison of unsedated ultrathin versus standard esophagogastroduodenoscopy in routine outpatient gastroenterology practice: does it work better through the nose? Endoscopy. 2003;35:647-651. |
| 10. | Zaman A, Hahn M, Hapke R, Knigge K, Fennerty MB, Katon RM. A randomized trial of peroral versus transnasal unsedated endoscopy using an ultrathin videoendoscope. Gastrointest Endosc. 1999;49:279-284. |
| 11. | Saeian K. Unsedated transnasal endoscopy: a safe and less costly alternative. Curr Gastroenterol Rep. 2002;4:213-217. |
| 12. | Yagi J, Adachi K, Arima N, Tanaka S, Ose T, Azumi T, Sasaki H, Sato M, Kinoshita Y. A prospective randomized comparative study on the safety and tolerability of transnasal esophagogastroduodenoscopy. Endoscopy. 2005;37:1226-1231. |
| 13. | Mori A, Fushimi N, Asano , T , Maruyama T, Ohashi N, Okumura S, Inoue H, Takekoshi S, Friedman SL. Cardiovascular tolerance in unsedated upper gastrointestinal endoscopy: prospective randomized comparison between transnasal and conventional oral procedures. Dig Endosc. 2006;18:282-287. |
| 14. | Mori A, Ohashi N, Maruyama T, Tatebe H, Sakai K, Shibuya T, Inoue H, Okuno M. Cardiovascular tolerance in upper gastrointestinal endoscopy using an ultrathin scope: a prospective randomized comparison between transnasal and transoral procedures. Dig Endosc. 2008;18:In press. |
| 15. | Mori A, Ohashi N, Tatebe H, Maruyama T, Inoue H, Takegoshi S, Kato T, Okuno M. Autonomic nervous function in upper gastrointestinal endoscopy: A prospective randomized comparison between transnasal and oral procedures. J Gastroenterol. 2008;43:38-44. |
| 16. | Mori A, Asano T, Maruyama T, Ohashi N, Inoue H, Takekoshi S, Okuno M. Transnasal ERCP/ENBD using an ultrathin esophagogastroduodenoscope. J Gastroenterol. 2006;41:1237-1238. |
| 17. | Mori A, Ohashi N, Maruyama T, Tatebe H, Sakai K, Inoue H, Takegoshi S, Okuno M. Endoscopic retrograde cholangiopancreatography through gastric stoma using ultrathin endoscope: a novel approach. Endoscopy. 2007;39:E323. |
| 18. | Lieberman DA, Wuerker CK, Katon RM. Cardiopulmonary risk of esophagogastroduodenoscopy. Role of endoscope diameter and systemic sedation. Gastroenterology. 1985;88:468-472. |
| 19. | Mori A, Tatebe H, Ohashi N, Maruyama T, Sakai K, Shibuya T, Okuno M. Balloon-assisted insertion of a cholangioscope into the common bile duct: a novel technique. Endoscopy. 2008;88:In press. |
| 20. | Mori A, Sakai K, Ohashi N, Maruyama T, Tatebe H, Shibuya T, Inoue H, Okuno M. Electrohydraulic lithotripsy of the common bile duct stone under transnasal direct cholangioscopy. Endoscopy. 2008;88:In press. |
| 21. | Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853-857. |
| 22. | Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721-731. |
| 23. | Hart R, Classen M. Complications of diagnostic gastrointestinal endoscopy. Endoscopy. 1990;22:229-233. |
| 24. | Christensen M, Hendel HW, Rasmussen V, Hojgaard L, Schulze S, Rosenberg J. Endoscopic retrograde cholangiopancreatography causes reduced myocardial blood flow. Endoscopy. 2002;34:797-800. |
| 25. | Johnston SD, McKenna A, Tham TC. Silent myocardial ischaemia during endoscopic retrograde cholangiopancreatography. Endoscopy. 2003;35:1039-1042. |
| 26. | Fisher L, Fisher A, Thomson A. Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc. 2006;63:948-955. |
| 27. | Christensen M, Milland T, Rasmussen V, Schulze S, Rosenberg J. ECG changes during endoscopic retrograde cholangio-pancreatography and coronary artery disease. Scand J Gastroenterol. 2005;40:713-720. |
| 28. | Miura F, Takada T, Kawarada Y, Nimura Y, Wada K, Hirota M, Nagino M, Tsuyuguchi T, Mayumi T, Yoshida M. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:27-34. |
| 29. | Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139-147. |